Vaginal Hysterectomy (VH) is frequently performed gynaecological procedure, next only to cesarean section [1]. Most common indication for this surgery is third degree uterovaginal prolapse which is prevalent in parous women. First step of VH is creation of vaginal flaps by dissecting through vesicovaginal space anteriorly and rectovaginal space posteriorly. Dissection through right plane is important to decrease blood loss which is the prime concern to both surgeons and anaesthetists. Minimising blood loss not only facilitates surgery by clearing the operative field but also reduces postoperative morbidity i.e., pain and infection. Several methods have been used to control surgical blood loss including hydro dissection with saline, use of electrocautery, tourniquets or clamps and local infiltration with vasoconstrictive agents. Vasoconstrictors have been used to control blood loss in several gynaecological surgeries such as in myomectomy, abdominal and VH and hysteroscopy [2-4]. The various agents used for haemostasis are norepinephrine, vasopressin and saline infiltration etc.
Vasopressin (8-L-arginine) a nona-peptide is synthesised as a prohormone in the paraventricular and supraoptic nuclei of the hypothalamus. Three types of vasopressin receptors (V1A, V1B and V2) are described in literature. It is a drug that causes vasospasm and uterine muscle contractions. The half-life of this agent is 10-20 minutes. It is available as an ampoule with 20 U/mL and has been used upto 8U in dilution in various studies. In gynaecological surgeries it has been used in myomectomy, abdominal hysterectomy, dilatation, evacuation and curettage and hysteroscopy [2-4]. There are case reports of using vasopressin for control of hemorrhage caused by accreta at the time of caesarean. Recent studies have demonstrated that the use of vasopressin in various gynaecological surgeries is associated with reduced blood loss, decreased operative time and decrease the risk of infection [5-8]. It has been used in dilution with saline and infiltrated paracervically under the vaginal mucosa. This helps in dissection and reduces blood loss by vasoconstriction [1].
The main risk associated with local vasopressin injection include transient increase in Blood Pressure (BP), bradycardia, inadvertent intravascular infiltration and rarely cuff cellulitis [2,4]. Through this study, it was planned to evaluate the efficacy of submucosal infiltration with vasopressin in reducing blood loss in VH.
Materials and Methods
A randomised control trial was done in the Department of Obstetrics and Gynaecology in collaboration with Department of Anaesthesiology at a tertiary hospital in Delhi from November 2017 to April 2019. Prior approval was taken from Institutional Ethical Committee (IEC-HR/2017/32/63). Patients were taken for the surgery after informed consent. This trial was registered in CTRI (Clinical Trial Registry- India) and the registration number is - CTRI/2020/10/028377. Seventy Women of age <65 years with POP-Q stage III/IV prolapse [9] were recruited from the outpatient department as per inclusion and exclusion criteria and randomised into two groups. Trial design was parallel, allocation ratio was 1:1. There were no changes to methods after trial commencement.
Inclusion criteria: Women of age less than 65 years with POP-Q stage III/IV uterovaginal prolapse undergoing VH under neuraxial anaesthesia were included in the study.
Exclusion criteria: Women with haemoglobin less than 10 gm/dL, history of medical disorders like hypertension, ischemic heart disease, hepatic or renal disease, chronic obstructive pulmonary disease, history of migraine and epilepsy, known case of coagulopathy, history of previous pelvic surgery and any co-existing pelvic pathology or enlarged uterus were excluded from the study.
Sample size calculation: Sample size was calculated using prior study [10]; with SD values of 52.0 and 81.5 in study and control group respectively, at alpha 5% and power 80%, to estimate a difference of 46 mL in blood loss, a sample size of 35 subjects was required in each group.
The Socio-economic status scoring was done using Modified Kuppuswamy Classification [11], which is based on
a) Education of the head of the family
b) Occupation of head of family (if retired, last occupation)
c) Per capita income (Rupees/month)
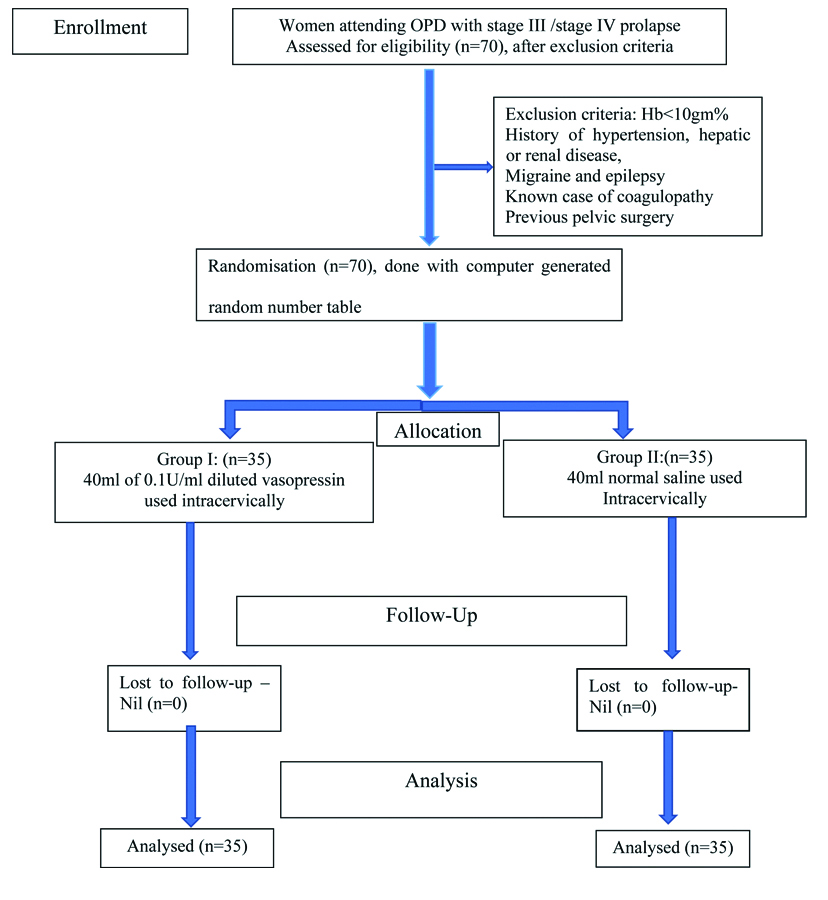
Participants were allocated in two groups using computer generated random number table. Simple randomisation was done. Author and her mentor did random number allocation sequence and enrollment of participants to interventions. There was no blinding. Consort flow diagram is in [Table/Fig-1].
Detailed history, examination and preoperative investigations were done. Indication of elective surgery was POP-Q stage III/IV uterovaginal prolapse. The patients were taken up for surgery after pre-anaesthetic clearance. Surgery was performed under neuraxial anaesthesia. Group I was intervention group (n=35), received infiltration under the vaginal mucosa with diluted vasopressin prior to the incision. A dilute solution of 0.1 U/mL of vasopressin was prepared by adding 20 unit of vasopressin in 200cc of normal saline. In group I patients, 40 mL of this solution (total 4 U) was injected in 2, 4, 8 and 10 O’ clock position around the cervix under the vaginal mucosa. In group II, 40cc of normal saline was used for infiltration. Anaesthetist was informed prior to the infiltration. Immediate blanching of vaginal mucosa postinfiltration with vasopressin was observed. An inverted T incision was given on the anterior vaginal wall extending it curvilinearlly around the external os. Vaginal flaps were created by dissecting anteriorly through vesicovaginal space and posteriorly through rectovaginal space. The standard surgical procedure of VH remained the same in both the groups. The primary outcome was to estimate operative blood loss, which was calculated by: a) difference in the weight of wet sponges used in surgery pre and post procedure; b) difference in the weight of Kelly’s pad pre and postsurgery; c) measuring the blood collected in the suction canister. Secondary surgical parameters i.e., ease of dissection, use of electrocautery, duration of surgery etc., were also noted. Patients were followed-up in postoperative period from the day of surgery till their hospital stay. Complications i.e., pain, discharge, urinary complains and wound infection were noted.
Statistical Analysis
All the qualitative parameters were compared between the two groups by chi-square test and quantitative parameters by unpaired t-test. Inter and intragroup comparisons were done by Repetitive Measure ANOVA followed by Tukey’s test. The parameters which did not follow the Gaussian distribution were compared by non-parametric Mann-Whitney test between the two groups. A p-value <0.05 was considered as significant. All the data analysis was carried out in SPSS version 20.0.
Results
The mean age of the patients in group I and group II was 48.34±9.56 years and 50.83±7.79 years respectively. This was not statistically significant and it was comparable (p=0.237). In group I, 20 out of 35 (57.2%) patients had parity more than three, while in group II, 17 out of 35 (48.6%) patients had parity more than three. This difference was also not statistically significant (p=0.632) [Table/Fig-2].
Comparison of demographic profile in both groups.
| Parameter | Group I (n=35) | Group II (n=35) | p-value |
|---|
| Age (years) | 48.34±9.56 | 50.83±7.79 | 0.237 |
| Parity | ≤3 | 15 (42.8%) | 18 (51.4%) | 0.632 |
| >3 | 20 (57.2%) | 17 (48.6%) |
| Socio-economic status | Upper | | | 0.696 |
| Upper middle | 1 (2.8%) | 2 (5.7%) |
| Lower middle | 9 (25.7%) | 11 (31.4%) |
| Upper lower | 25 (71.5%) | 22 (62.9%) |
| Lower | | |
| Education | Illiterate | 4 (11.4%) | 4 (11.4%) | 0.888 |
| Schooling | 19 (54.4%) | 22 (63.0%) |
| Graduate | 11 (31.4%) | 8 (22.8%) |
| Post graduate | 1 (2.8%) | 1 (2.8%) |
| Occupation | Home maker | 33 (94.3%) | 33 (94.3%) | 1.000 |
| Working | 2 (5.7%) | 2 (5.7%) |
p-value (qualitative parameters by chi-square test and quantitative parameters by t-test)
The mean estimated intraoperative blood loss from incision till creation of flaps was 21.33±74 mL in group I and 49.67±17 mL in group II respectively. It was observed that the blood loss in saline group was more than double when compared to vasopressin group and this difference was statistically significant (p=0.001). In both the groups, 4 out of 35 (11.4%) patients required blood transfusion (p=1.000). In group I, overall ease of dissection was seen in 21 out of 35 (60%) patients and out of these, good ease of dissection was noted in 4/35 (11.4%) patients; as the flaps were easily created postinfiltration. In group II, 30 out of 35 (85.7%) patients were found to have ease of dissection and good ease of dissection was seen in 12/35 (34.2%) patients. Overall, saline infiltration group had much better ease of dissection as compared to vasopressin group (p=0.016). In group I, use of electro cautery was noted in 17/35 (48.6%) patients and out of these, usage was more than three times in 2/35 (5.8%). Whereas in group II, there was use of electro cautery in 23/35 (65.8%) patients and out of these, 3/35 (8.7%) had it more than three times. Hence, saline group needed electro cautery more frequently during surgery as compared to vasopressin group (p=0.381) [Table/Fig-3]. The duration of surgery from incision till creation of flaps in vasopressin group was 19.00±4.18 minutes, and in saline group it was 20.63±5.37 minutes; this time difference was statistically insignificant (p=0.162). The total duration of surgery in vasopressin group was 133.57±10.259 minutes and in saline group it was 128.57±9.438 minutes. Although this time difference was not much, but it was statistically significant (p=0.037).
Comparison of intraoperative parameters in both the groups.
| Parameter | Group I (n=35) | Group II (n=35) | p-value |
|---|
| Intraoperative blood loss from incision till creation of flaps (mL) | 21.33±74 | 49.67±17 | 0.001* |
| Need of blood transfusion | 4 (11.4%) | 4 (11.4%) | 1.000 |
| Ease of dissection | No | 14 (40%) | 5 (14.3%) | 0.016* |
| Yes | 21 (60%) | 30 (85.4%) |
| Use of electro cautery (no. of times) | 0 | 18 (51.4%) | 12 (34.2%) | 0.381 |
| ≤3 | 15 (42.8%) | 20 (57.1%) |
| >3 | 2 (5.8%) | 3 (8.7%) |
| Duration of surgery (minutes) | From incision till flaps creation | 19.00±4.18 | 20.63±5.375 | 0.162 |
| Total duration of surgery | 133.57±10.25 | 128.57±9.438 | 0.037* |
p-value (qualitative parameters by chi-square test and quantitative parameters by t-test); *-Statistically significant
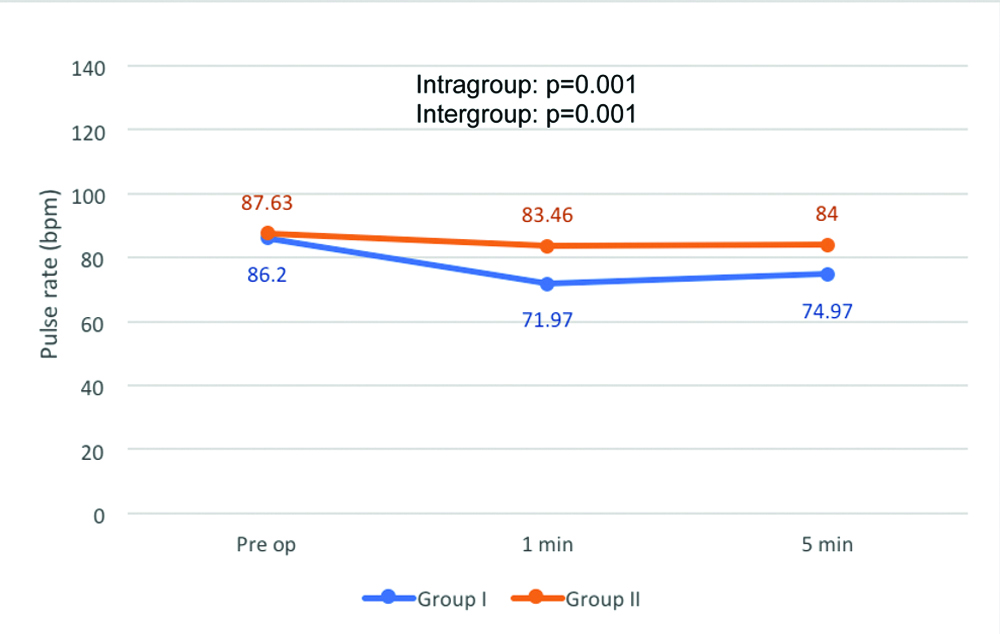
The mean pre-operative pulse rate in group I was 86.20 bpm and at 1-minute vasopressin infiltration, it dropped to 71.97 bpm and this was statistically significant (p<0.001) [Table/Fig-4]. At 5 minutes, it became 74.97 bpm, and significantly different (p<0.001). In group II also there was significant fall in pulse rate at one minute (p<0.001) but not as much as in group I. However, there was a rise at 5 minutes postinfiltration but still it remained significantly below from baseline (p<0.001).
Comparison of intraoperative pulse rate within and between the groups.
p-value (F test Repetitive Measure ANOVA); bpm: beats per minute
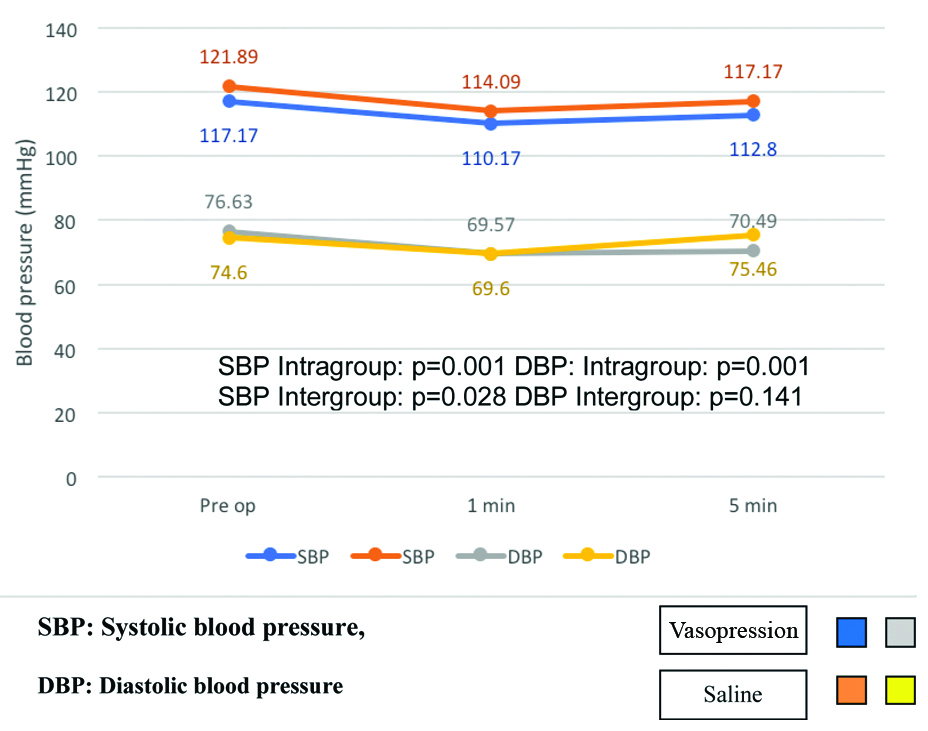
The mean systolic blood pressure in group I dropped at one minute and this difference was statistically significant (p<0.001) [Table/Fig-5]. At 5 minutes it picked up however was still significantly lower when compared to baseline (p<0.001). In group II, the systolic blood pressure was decreased at one minute and this fall was statistically significant (p<0.001). The SBP increased at five minutes to but the difference from baseline was still significant (p<0.001). On intragroup comparison, there was significant postinfiltration fall of systolic blood pressure at one and five minutes in both groups (p<0.001). On intergroup comparison, the difference in systolic blood pressure was found to be statistically significant between groups (p=0.028). The diastolic blood pressure in group I fell one minute postinfiltration and at five minutes it rose slightly. A significant difference at one minute and at five minutes when compared with preoperative diastolic pressure was seen (p<0.001). Also In group II the preoperative diastolic blood pressure fell one minute and this was statistically significant (p<0.001). Diastolic blood pressure rose again at five minutes and was slightly higher than baseline (p<0.001). For group I and group II intragroup changes in diastolic blood pressure were significant at one and five minutes when compared to baseline (p=0.001). However, on intergroup comparison there was no statistical difference in DBP (p=0.141).
Comparison of Systolic and Diastolic BP within the group and between the groups.
p-value (F test repetitive measure ANOVA)
In group I, 4 out of 35 (11.4%) patients had some postoperative complications as compared to 5/35 (14.3%) in group II. Vaginal discharge was seen in 2/35 (5.7%) patients in vasopressin group and 3/35 (8.7%) in saline group. Febrile illness was seen in 2/35 (5.7%) patients in vasopressin group and 1/35 (2.8%) in saline group. No case of vaginal bleeding was noted in vasopressin group while in saline group vaginal bleeding was seen in one patient (p=0.916). The mean duration of hospital stay in group I was 3.74±0.61 days while in group II it was 4.46±0.61 days, which was statistically significant (p=0.001).
Discussion
Traditionally, VH is being performed with saline injection intracervically to create mechanical tamponade and to create easier plane of dissection. Use of hydro dissection with different types of vasoconstrictor agents is expanding [8]. The use of vasopressin as a medical mean to decrease the blood loss has been studied in few studies. In this study, women receiving vasopressin had almost half blood loss comparing to the women receiving saline.
When compared with other studies it was found that in a study by Jullian TM et al., they observed less blood loss in vasopressin group compared to saline group 296±37 mL vs 435±55 mL (p<0.02) during VH [12]. Ascher-Walsh CJ et al., did a study where they used vasopressin and found less blood loss 145.3 mL vs 226.4 mL (p=0.022) [13]. An RCT by Frederick J et al., also showed significant decrease in blood loss with vasopressin used during myomectomy [14].
It was observed that ease of dissection felt during separation of planes was more in saline group as compared to vasopressin group. Saline use for hydrodissection causes mechanical tamponade of cervico-vaginal vessels and separates planes of tissue prior to the incision being made [8,15]. However, the use of electrocautery was more in saline group as compared to vasopressin group. No other study has compared these parameters.
The clinical response of vasopressin injection is fall in pulse rate and rise in blood pressure [16]. In this study both the groups had fall in pulse rate but not below 60 bpm. Okin CR et al., [2] noticed in their study the fall in pulse rate by 15 beats/min in 22.2% patients in vasopressin group. Henn EW et al., also reported the fall in mean pulse rate in ornipressin group and slight fall in saline group [10].
In this study, mean systolic BP at one minute fell and then picked up at five minutes in vasopressin group (p=0.001). In saline group also falling trend was noted. Also, in DBP there was initial fall in BP and then it rose (p=0.001). There was no increase in BP in our study probably due to low dose and intracervical infiltration which had only local action. The fall in blood pressure was likely due to neuroaxial anaesthesia. In the study by Singh P et al., after 8 U of vasopressin infiltration, there was rise in mean blood pressure [15]. This rise was likely due to higher dose of vasopressin infiltrated. Jullian TM et al., did a study in which 10 units of vasopressin was used and observed that vasopressin elevated mean systolic and diastolic pressure [12]. Kammerer-Doak DN et al., reported that the mean change in blood pressure were not significant between the groups; the dose of vasopressin used was 4 units in 18cc of saline [17]. None of the studies have reported any major cardiovascular complications. However further studies on larger sample size are recommended to gather more evidence in this regard. Vasopressin is short acting with half-life of 10-20 minutes. Research using long acting vasopressin analog i.e., Terlipressin which is effective for 4-6 hours and which may reduce total surgical blood loss is also recommended.
Limitation(s)
Small sample size and no blinding were the limitation of the study.
Conclusion(s)
No surgical procedure is more gratifying than the one done with minimal blood loss. Here, we found that at an infiltration dose of four units, vasopressin appears to be safe and effective in VH. No major adverse reaction was noted with vasopressin infiltration.
p-value (qualitative parameters by chi-square test and quantitative parameters by t-test)
p-value (qualitative parameters by chi-square test and quantitative parameters by t-test); *-Statistically significant