Anaesthetic Management of Non Traumatic Diaphragmatic Hernia as a Co-existing Disease: Combined Spinal Epidural to Rescue
Divya Gahlot1, Kirti Nath Saxena2, Bharti Wadhwa3
1 Senior Resident, Department of Anaesthiology, Maulana Azad Medical College and Lok Nayak Hospital, Delhi, India.
2 Director Professor, Department of Anaesthiology, Maulana Azad Medical College and Lok Nayak Hospital, Delhi, India.
3 Professor, Department of Anaesthiology, Maulana Azad Medical College and Lok Nayak Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Divya Gahlot, D-55, Arya Nagar Apartments, IP Extension, Patpar Ganj, Delhi-110092, India.
E-mail: gahlotdivya63@gmail.com
Diaphragmatic hernia is a congenital or acquired defect in diaphragm, resulting in herniation of abdominal viscera into thoracic cavity. Acquired diaphragmatic hernia are seen mostly in patients with blunt or penetrating abdominal injuries. Non traumatic acquired diaphragmatic hernias have been reported in literature but are extremely rare. Anaesthetic management of a patient presenting with Non traumatic diaphragmatic hernia as a co-existing disease offer unique challenges and considerations. This report was about the successful anaesthetic management of a 66-year-old male having Osteoarthritis (OA) of left knee with long standing massive right diaphragmatic hernia as a co-existing disease. The patient was scheduled for left Total Knee Replacement (TKR). Combined Spinal Epidural (CSE) with low dose Subarachnoid Block (SAB) was the anaesthetic technique of choice. Femoral sciatic block is an alternate technique of anaesthesia for such patients.
Anaesthetic technique, Osteoarthritis, Subarachnoid block, Total knee replacement
Case Report
A 66-year-old male, scheduled for left TKR in view of OA of left knee, presented to preanaesthetic clinic. He was a known case of hypertension for the past 10 years, controlled on oral drugs. There was no history of dyspnea, orthopnea, chest pain, paroxysmal nocturnal dyspnea.
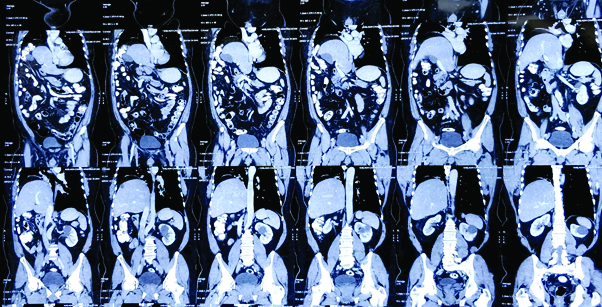
The functional capacity of the patient was difficult to assess, as the patient had difficulty in walking due to OA of knee. Breath holding time was 18 seconds; on auscultation breath sounds were reduced on right side. Chest X-ray showed homogenous radio opacity seen obscuring right mid and lower zone likely to be either consolidation or collapse or effusion [Table/Fig-1]. Contrast-Enhanced Computed Tomography (CECT) thorax and abdomen reported right diaphragmatic hernia with herniation of liver, omental fat and hepatic flexure into right thoracic cavity [Table/Fig-2] causing compression and displacement of heart and mediastinum towards left side with compression of right and left atria and splaying of right pulmonary vessels with basal atelectasis of the right lung. Pulmonary Function Test (PFT) showed mild restrictive pattern with Forced Vital Capacity (FVC) 77%, Forced Expiratory Volume 86%, FEV1/FVC of 105%.
Chest X-ray showing homogenous opacity on right-side of lung with blunting of Costophrenic angles.

Serial images of CECT abdomen and thorax showing right diaphragmatic hernia with herniation of liver, omentum and hepatic flexure of colon.
Rest of the medical and surgical history, preanaesthetic examination and biochemical investigations were normal. As the patient was asymptomatic and PFTs showed mild restrictive pattern, no surgical intervention was advised. Patient was planned for left TKR under CSE anaesthesia.
Epidural catheter was inserted at L3-L4 intervertebral space catheter was fixed at 10 cm. The SAB was performed at L4-L5 intervertebral space and 2.2 mL of 0.5% bupivacaine heavy was administered. Level of motor block achieved was T10-T12. The surgical procedure lasted for 2 hours and intraoperative and postoperative period was uneventful. A 6 mL of 0.125% bupivacaine was administered postoperatively through epidural catheter as per patient’s requirement. Rescue analgesia was managed with systemic analgesics (intravenous paracetamol 1 gm and diclofenac 75 mg). Routine monitoring with SpO2 and vital charting was done postoperatively.
Discussion
Diaphragm is the largest respiratory muscle separating thorax from the abdominal cavity [1]. Diaphragmatic hernia is defect in the diaphragm which may be congenital or acquired causing abdominal organs to herniate into the thoracic cavity. While congenital diaphragmatic hernias are due to defect that progresses in the embryologic period, acquired defects occur because of trauma in 75% of cases [2]. Only few reported cases are non traumatic in origin [3,4]. The patient reported here had no history of trauma and had no specific symptoms such as dyspnea, tachypnea, cough, chest or abdominal pain. Diaphragmatic hernia was an incidental finding preoperatively in the present case.
Owing to its rarity, anaesthetic management of patients with diaphragmatic hernia as a co-existing disease is not adequately described in literature. A prior diagnosis helped anaesthesia team to prepare for possible difficulties and complications that were expected in this condition. Since the surgery could be done under central neuraxial block, CSE was anaesthesia of choice in the present case. However, respiratory compromise can occur in these patients with high level of block in regional anaesthesia because of blockade of the muscles of respiration and reduction in inspiratory capacity and expiratory reserve volume [5]. Thus, a careful titration of local anaesthetics should be done to prevent high level of block. The SAB with lower drug volume, in order to avoid high level of block, was administered and an epidural catheter was inserted to both supplement low level of block and maintain optimal level of block in case of recession of block. It permitted the advantage of early onset of effect, flexibility of using graduated doses of drug through epidural catheter for a better haemodynamic stability as well as avoidance of conversion to general anaesthesia. Faheem M and Fayad A, have reported spontaneous diaphragmatic rupture in a patient with diaphragmatic eventration after lower limb surgery under epidural anaesthesia, the probable mechanism of which was explained to be an increase workload of the diaphragm due to high regional block [5].
Another concern is the positioning of the patient, supine positioning during the procedure causes reduction in Functional Residual Capacity (FRC) and may increase the herniation of abdominal viscera into thoracic cavity increasing the respiratory compromise in these patients [6]. Specific positions such as Trendelenburg and lithotomy which further causes FRC reduction should be used cautiously in these patients.
Although, general anaesthesia was not the anaesthesia of choice in the present case, it is important to understand the difficulties in its administration. Administration of general anaesthesia offers greater difficulties and needs higher vigilance in these patients as compared to regional technique. In patients with abdominal viscera occupying a large portion of the thoracic cavity, a higher risk of regurgitation, aspiration, hypoxemia, and haemodynamic compromise should be considered [7]. Tracheal intubation difficulties may also be encountered because of mediastinal shift and deviation of the trachea in these patients. Direct compression of mediastinum and great vessels caused by mass effect impairs venous return to the heart and decreases cardiac output [8]. Administration of positive pressure ventilation further compromises the venous return and poses a higher risk of intraoperative haemodynamic instability in these patients [6]. Use of nitrous oxide should be avoided, as its use causes expansion of intra-abdominal viscera, increases the herniation and mediastinal shifting causing further respiratory and circulatory impairment [8]. Increase in intra-abdominal pressure such as coughing, bucking and lighter planes of anaesthesia further should be avoided as it can further increase herniation of contents into thorax causing increase in respiratory and circulatory compromise [5,7].
Peripheral nerve block such as femoral sciatic nerve block is a known approach and a good alternative anaesthetic approach in these patients. Compared with neuraxial anaesthesia it minimises hypotension, ensures better haemodynamic stability and less respiratory compromise. However, increased induction time and requirement of expertise may be the limiting factor of using this approach [9].
Conclusion(s)
Non traumatic diaphragmatic hernias are a rare entity in adult patients, which require meticulous and appropriate anaesthetic management. A thorough evaluation of patient in the preoperative period can help identify these rare disorders and thus give us the opportunity to prepare ourselves for the possible difficulties and complications during the surgery. Central neuraxial block is advantageous as compared to general anaesthesia in these patients owing to its greater haemodynamic stability, lesser respiratory compromise and better postoperative outcome. However, caution should be maintained to prevent higher level of blocks in these patients. Graded epidural with low dose SAB appears to be safest option for lower abdominal and lower limb surgeries. Peripheral nerve blocks with appropriate respiratory monitoring are preferable option for upper limb surgeries. Therefore, a thorough preoperative assessment with knowledge of the associated anaesthetic considerations can help anaesthesiologists to avoid unnecessary complication and have a best possible patient outcome.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 31, 2020
Manual Googling: Jan 21, 2021
iThenticate Software: Apr 21, 2021 (11%)
[1]. Pataka A, Paspala A, Sourla E, Bagalas V, Argyropoulou P, Non traumatic liver herniation due to persistent cough mimicking a pulmonary massHippokratia 2013 17(4):376-77. [Google Scholar]
[2]. Bianchi E, Mancini P, Vito SD, Pompili E, Congenital asymptomatic diaphragmatic hernias in adults: A case seriesJ Med Case Rep 2013 7:12510.1186/1752-1947-7-12523668793 [Google Scholar] [CrossRef] [PubMed]
[3]. Mar Fan MJ, Coulson ML, Siu SK, Adult incarcerated right sided Bochdalek herniaAust N Z J Surg 1999 69:239-41.10.1046/j.1440-1622.1999.01538.x10075372 [Google Scholar] [CrossRef] [PubMed]
[4]. Arsalane A, Herman D, Bazelly B, Left strangulated diaphragmatic hernia: An unusual complication of gastric bypassRev Pneumol Clin 2005 61:374-77.10.1016/S0761-8417(05)84867-9 [Google Scholar] [CrossRef]
[5]. Faheem M, Fayad A, Diaphragmatic rupture after epidural anaesthesia in a patient with diaphragmatic eventrationEur J Anaesthesiol 1999 16:574-76.10.1097/00003643-199908000-0001610500951 [Google Scholar] [CrossRef] [PubMed]
[6]. Miller RD, Cohen NH, Ericksson Fleisher LA, Weiner-Kronish JP, Young WL, Miller’s Anaesthesia 2015 8th editionPhiladelphia, PA 19103-2899Elsevier:1448-49. [Google Scholar]
[7]. Katz RI, Belenker SL, Poppers PJ, Intraoperative management of a patient with a chronic, previously undiagnosed traumatic diaphragmatic herniaJ Clin Anaesth 1998 10:506-09.10.1016/S0952-8180(98)00065-8 [Google Scholar] [CrossRef]
[8]. William DJ, Sandby-Thomas MGF, Anaesthetic management of acute gastric volvulus in an adultBritish Journal of Anaesthesia 2003 90:96-98.10.1093/bja/aeg007 [Google Scholar] [CrossRef]
[9]. Jeon YT, Peripheral nerve block for anaesthesia in patients having knee arthroplastyKorean J Anaesthesiol 2012 62(5):403-04.10.4097/kjae.2012.62.5.40322679534 [Google Scholar] [CrossRef] [PubMed]