Utility of FNAC in primary diagnosis of tumours in the last few decades has been very successful. This is due to continuous, consistent and critical association between cytological assessment and histopathological diagnosis [1].
The role of FNAC is well documented in patients of salivary gland lesion for preoperative evaluation, but due to lack of uniform system for reporting, its efficacy has been limited. There were different classification and reporting formats for salivary gland lesions with varied category schemes, which makes it difficult for clinicians to interpret the report [1].
The 2017 WHO classification of salivary gland tumour lists 11 types of primary benign tumour (adenomas) and 20 types of malignant tumours (carcinoma) with subtypes in some. Also, there are non epithelial tumours, malignant lymphomas and secondary tumours [2]. Similarly, different classifications give long and varied list of lesions.
The MSRSGC was proposed by an international panel of experienced cytopathologists in 2015 at the European congress of cytology held in Milan, Italy. It is a uniform and evidence based reporting system for salivary gland FNACs consisting of six diagnostic categories. There was participation of 40 experts from 14 different countries [3,4]. This system is based upon the literature as well as upon the experience of experts from a multidisciplinary group involved in the field of salivary gland cytopathology [3].
The aim of the MSRSGC was to provide enhanced communication between pathologist and clinician and improved patient care as already established in the Bethesda system for reporting cervical (The Bethesda System for Reporting Cervical Cytopathology and thyroid (The Bethesda System for Reporting Thyroid Cytopathology [5-6]. It provides a standardised terminology and ROM for each category and therefore minimises the ambiguity seen in interpretation of FNAC reports. There is a need to clearly understand the merits and demerits of reporting salivary gland cytopathology and histopathology which helps in management of ROM in salivary gland lesions. Hence the study was designed to categorise ROM in patients with salivary gland lesions.
Materials and Methods
The present study was a cross-section (retrospective) conducted for three year a tertiary care hospital conducted in a tertiary care hospital in the Department of Pathology, Chirayu Medical College and Hospital Bhopal, Madhya Pradesh, India. The study was conducted from 1st September to 31st October 2020.
Inclusion criteria: All the cases of salivary gland swelling that were registered in the Department of Pathology between January 2017 to December 2019 were included in the study.
Exclusion criteria: Salivary gland like tumours in organs other than salivary gland were excluded from the study.
Study Procedure
Relevant clinical details, fine needle aspiration smears, histopathological slides, blocks and final reports were retrieved from the departmental archives.
Fine needle aspiration cytology was performed by percutaneous or intraoral aspiration using 22-24 gauge needles after taking informed consent. A minimum of two passes were performed. In the case of large swellings, aspiration was done from different areas to minimise sampling error. Cystic lesion was aspirated till complete evacuation and again FNAC was done from residual solid area. Aspirated fluid was subjected to centrifugation and smears were prepared from the sediment.
Air dried-smears were routinely fixed, processed and stained using Geimsa stain. 1-3 slides per case were fixed in 95% alcohol and were stained by Papanicolaou’s method.
The results obtained on FNAC were divided into six categories as per Milan system [4]: (1) non diagnostic; (2) non-neoplastic; (3) Atypia of Undetermined Significant (AUS); (4) Neoplasm (a- Benign; b- Salivary gland neoplasm of uncertain malignant potential SUMP); (5) Suspicious for malignancy (SM); (6) Malignancy. For histopathology examination authors used 10% neutral buffer formalin for fixation, processed the specimen and stained with Haematoxylin and Eosin (H&E) stain. Results of cytology and histopathology were compared and ROM was calculated by dividing the number of cases that came out to be malignant in each category by the total number of cases in that category on histopathology.
Statistical Analysis
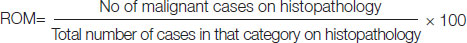
For statistical analysis the cases from the collected data were distributed according to age, sex and site. Total 63 cases were categorised into six Milan categories on cytology. Histological follow-up was done. Histopathological diagnosis was considered as the gold standard. ROM was calculated as follows in the form of percentage.
Results
Out of total 63 cases of salivary gland swelling FNAC histopathological association was found in 45 of cases. The most common site was parotid with 34 (53.9%) cases followed by submandibular 26 (41.2%) and minor salivary gland 2 (3.1%). Single case of sublingual salivary gland was observed in the study. Common age group was found to be 5th decade with 16 cases (25.3%) followed by 10 cases each in 4th and 6th decade. A male preponderance with Male: Female ratio 1.42:1 was observed [Table/Fig-1].
Age, gender and site distribution.
| Clinical features | No. of cases (N) | (%) |
|---|
| Age distribution (years) |
| 11-20 | 5 | 7.9 |
| 21-30 | 9 | 14.2 |
| 31-40 | 10 | 15.8 |
| 41-50 | 16 | 25.3 |
| 51-60 | 10 | 15.8 |
| 61-70 | 8 | 12.6 |
| 71-80 | 5 | 7.9 |
| Gender distribution |
| Males | 37 | 58.7 |
| Females | 26 | 41.2 |
| Site distribution |
| Parotid gland | 34 | 53.9 |
| Submandibular gland | 26 | 41.2 |
| Sublingual gland | 1 | 1.5 |
| Minor salivary gland | 2 | 3.1 |
Categorisation of cases according to Milan system has been depicted in [Table/Fig-2]. Maximum number of cases were seen in category IV- neoplasm. There are 27 (42.8%) cases out of total 63 cases in this category. Out of these 27 cases 24 were placed in benign IV a and three cases in category IV b. A 22 of these benign cases were diagnosed as pleomorphic adenoma. From the other two cases one case was diagnosed as basal cell adenoma and the other was given a diagnosis of benign salivary gland tumour without further sub classification. Basal cell adenoma which was on cytopathology was found to be adenoid cystic carcinoma on histopathology.
Spectrum of total salivary gland lesions as per Milan system (Number of cases-63).
| S. No. | Diagnostic category | No. of cases (N) |
|---|
| 1 | Category I- Non diagnostic | 6 (9.5%) |
| 2 | Category II- Non-neoplastic | 11 (17.4%) |
| Chronic sialadenitis | 4 |
| Acute sialadenitis | 2 |
| Benign cystic lesion | 2 |
| Chronic non-specific inflammation | 2 |
| Granulomatous sialadenitis | 1 |
| 3. | Category III- AUS | 2 (3.17%) |
| 4 | Category IV- Neoplasm | 27 (42.8%) |
| a. Benign | 24 |
| Pleomorphic adenoma | 22 |
| Benign salivary gland tumour | 1 |
| Basal cell adenoma | 1 |
| b. SUMP | 3 |
| 5 | Category V- Suspicious for Malignancy (SM) | 3 (4.7%) |
| 6 | Category VI- Malignant | 14 (22.2%) |
| High grade salivary gland tumour | 5 |
| Mucoepidermoid carcinoma | 3 |
| Adenoid cystic carcinoma | 2 |
| NHL | 1 |
| Acinic cell carcinoma | 1 |
| Poorly differentiated carcinoma? metastasis | 1 |
| Carcinoma ex. Pleomorphic adenoma | 1 |
Next common diagnosis was category VI- malignant with 14 cases. It includes a spectrum of cases like Mucoepidermoid carcinoma (three cases), adenoid cystic carcinoma (two cases), an acinic cell carcinoma (one case), five cases were diagnosed as high-grade salivary gland malignant tumour (without specific diagnosis) one of which turned out to be non malignant on histopathology.
Eleven cases were seen in category II- Non-Neoplastic with most common diagnosis of chronic sialadenitis four cases out of 11. One case of chronic nonspecific inflammatory lesion on cytopathology was diagnosed to be Warthin’s tumour on histopathological examination.
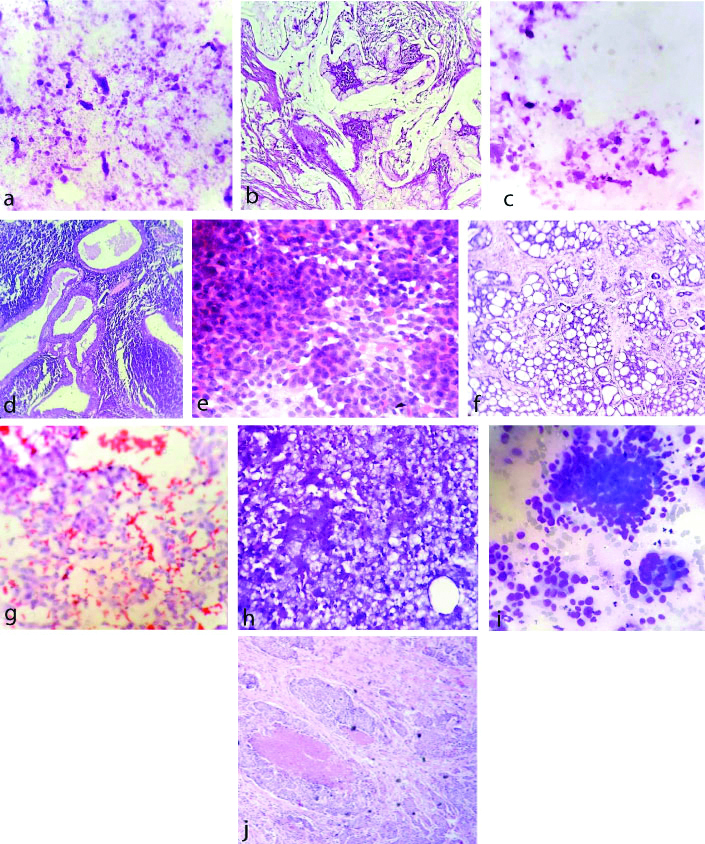
There were six cases which yielded scanty or no salivary gland tissue on more than one aspiration, these were placed in category II Non diagnostic. Category III AUS and category V suspicious for malignancy included two (3.1%) and three (4.7%) cases, respectively. Number of cases with histopathological association and the calculated ROM is shown in [Table/Fig-3]. Microscopic pictures of different Milan categories is shown in [Table/Fig-4a-j].
Histological follow-up of Milan system diagnostic categories and ROM.
| S. No. | Diagnostic category | No. of cases | No. cases with histopathological follow-up | No. of malignant cases | ROM (Risk of malignancy) |
|---|
| 1 | Category I- Non diagnostic | 6 (9.5%) | 4 | 1/4 | 25% |
| 2 | Category II- Non-neoplastic | 11 (17.4%) | 5 | 0/5 | 00% |
| 3 | Category III- AUS | 02 (3.1%) | 2 | 1/2 | 50% |
| 4 | Category IV | 27 (42.8%) | 21 | - | - |
| Benign | 24 (38%) | 20 | 1/20 | 5.0% |
| SUMP | 03 (4.7%) | 1 | 1/1 | 100% |
| 5 | Category V- Suspicious | 03 (4.7%) | 3 | 3/3 | 100% |
| 6 | Category VI- Malignant | 14 (22.2%) | 10 | 9/10 | 90% |
(a-b)-Acellular aspirate from a non diagnostic FNAC (MGG 10X), Mucoepidermoid carcinoma on histopathology (H&E 10X), (c-d)- Chronic nonspecific inflammation from parotid gland (MGG 10X), Warthin’s Tumour on histopathology (H&E10X), (e-f)-Basal cell adenoma from a case of parotid swelling (MGG 40X), Adenoid cystic carcinoma on histopathology (H&E 10X), (g-h)-SUMP epithelial cell with vacuolated cytoplasm (MGG 10X), Acinic cell carcinoma on histopathology (H&E 10X), (i-j)-High grade salivary gland tumour possibly SDC (MGG 10X), Salivary duct carcinoma on histopathology (H&E 10X).
Risk of malignancy in present study is compared with the proposed ROM in MSRSGC [4] [Table/Fig-5].
Comparison of ROM in present study with MSRSGC.
| S. No. | Diagnostic category | ROM in present study (%) | Proposed ROM (%) in MSRSGC, Esther D et al., [4] |
|---|
| 1 | Category I- Non diagnostic | 25 | 25 |
| 2 | Category II- Non-neoplastic | 00 | 10 |
| 3 | Category III- AUS | 50 | 20 |
| 4 | Category IV | - | - |
| Benign | 5 | <5 |
| SUMP | 100 | 35 |
| 5 | Category V- Suspicious for malignancy | 100 | 60 |
| 6 | Category VI- Malignant | 90 | 90 |
Discussion
The FNAC is safe cost-effective and quite accurate method for evaluation of salivary gland swellings. Salivary gland swellings are easily accessible for FNAC and also the risk of fistula formation and capsule disruption with seeding of tumour cells is very low compared to surgical biopsy. The choice between surgical or conservative treatment often depends on FNAC diagnosis. Although, cytological criteria are well defined and the diagnosis is relatively easy for the common salivary gland tumours, still the diagnostic difficulties arise due to heterogeneity of many tumours and the cytomorphological overlap, which also limits the accuracy of subtyping [1]. The Milan system is a risk stratification system having a great potential of improving clinical communication and guide treatment. There are very few studies to confirm competence of Milan system [7-9]. Present study though having some limitations will aid in confirming its competence.
In the present study, distribution of cases according to site are similar to finding observed in other studies [3,10]. The proportion of cases in different categories are quite similar to one study in which the percentage were 6.1%, 38.2%, 33.4%, 2.4% and 15%, respectively [11]. ROM in present study is quite similar to ROM in other studies [2,11-13].
Category I: Non diagnostic are aspirates having insufficient diagnostic material for an informative interpretation, which is due to scant cellularity or preservation artifacts.
Adequate cellularity from a target lesion is must for an accurate diagnosis. Guidelines for adequacy are presented in MSRSGC which suggest a minimum of 60 lesion cells as adequacy criteria [14]. Exceptions to these non diagnostic cytologic criteria include mucinous cyst contents, scanty aspirates with cellular atypia and aspirates containing abundant acellular matrix material or abundant inflammatory cells [14]. In the present study, out of total 63 cases six cases were placed in non diagnostic category I. All of these were haemorrhagic smears or smears with cystic fluid only. Histopathological association was available in four cases. One of these cases was diagnosed as Mucoepidermoid carcinoma on histological findings. This discrepancy may be due to the acellular aspirate from cystic area. ROM came out to be 25%.
Category II: Non-neoplastic lesions of salivary gland are common and they can be misdiagnosed clinically as neoplasm because of the mass lesion. In MSRSGC, this category includes benign conditions like reactive metaplastic and inflammatory process. Acute and chronic sialadenitis and reactive lymph nodes are included in this category. The ROM for aspirates of non-neoplastic salivary gland tumour is expected to be less than 10% [14-21]. In the present study, 11 cases were categorised in this category of non-neoplastic lesions. Most of these cases were inflammatory lesions, with most common diagnosis of chronic sialadenitis. Other cases were acute sialadenitis, chronic granulomatous sialadenitis, benign cystic lesions and chronic nonspecific inflammatory lesion. Histopathological association was available in five cases. A case which was given a diagnosis of chronic nonspecific inflammation, was diagnosed to be Warthin’s tumour on histopathology [Table/Fig-4c,d]. Presence of numerous chronic inflammatory cells and scant glandular cellularity on cytology might be the possible reason for wrong interpretation.
Category III: The AUS is a heterogeneous category showing morphological overlap between non-neoplastic and neoplastic processes. The ROM of this category is approx 20%. This category is formed with the intention to reduce the number of false positive diagnosis in neoplasm category and also the false negative cases in non-neoplastic category [14]. In this study, out of total 63 cases, two were classified as AUS. Histopathology was done for both of these, one of which was diagnosed as Mucoepidermoid carcinoma. Cells showing bland nuclei with prominent nucleoli might be the reason for categorisation into AUS. In present study, ROM was 50% in category III due to low sampling.
Category IV: Salivary gland neoplasms although uncommon constitute 6% of all tumour of head and neck region and 0.35% of all malignancies [14]. The neoplasm category of MSRGC is reserved for aspirates that have features diagnostic of neoplasm. It is divided into two subcategories: (a) benign and (b) salivary gland neoplasm of uncertain malignant potential. The sub category IV a Neoplasm- benign includes cases in which diagnosis of a specific benign neoplasm can be made on the basis of cytomorphological features. The ROM for neoplasm benign category IV a is low (<5%) [14]. In this study, Benign category IV a had 24 cases. Pleomorphic adenoma constituted highest number with 22 cases followed by basal cell adenoma and benign salivary gland neoplasm one case each. This category IV a had histological follow-up of 20 cases out of total 24 cases in cytology which revealed only one case to be discordant i.e., case of basal cell adenoma on FNAC was diagnosed to be adenoid cystic carcinoma on histopathology. Hyaline stromal globules surrounded by small epithelial cells could be the reason for misdiagnosis on cytopathology.
The neoplasm subcategory of SUMP IV b is reserved for salivary gland FNACs in which the morphological features are diagnostic of a neoplastic process but a specific diagnosis cannot be given. A differential diagnosis of benign and malignant entities is given. In the present study, out of three cases diagnosed as SUMP, 1 case for which histopathological association was available was reclassified as acinic cell carcinoma [Table/Fig-4g,h]. Presence of epithelial fragments of cells with abundant vacuolated cytoplasm resembling normal acinar cells resulted in a dubious interpretation. ROM in IV b was found to be 100% and this is because of low sample size (only one case).
Category V: The suspicious for malignancy category represent an indeterminate diagnostic category in the MSRSGC. The cytomorphological features of SM are highly suggestive of malignancy but are not definitive. Samples with limited cellularity containing few markedly atypical cells or sample suggestive of lymphoma but without adequate material for immunophenotyping are the examples where SM diagnosis is given [14]. The SM category along with AUS and SUMP are indeterminate diagnostic categories in MSRSGC.
In this study, three cases out of 63 were given a diagnosis suspicious for malignancy. All the three cases (100%) were confirmed to be malignant on histopathology. So ROM was 100%. This high ROM may be due to small sample size in this category. The ROM according to MSRSGC is 60% in this category.
Category VI: The category VI is for the aspirates that are diagnostic for a malignant lesion. It includes wide range of different malignant neoplasm from the major and minor salivary glands. Most of the neoplasms in this category are carcinomas, but it also includes, lymphomas, sarcomas and metastatic carcinomas to the salivary gland lymph nodes [14]. A specific classification based on WHO classification of head and neck tumour 2017 edition [2] should be made and also tumour be graded as low grade malignant tumour or high grade malignant tumour [14].
In this study, out of 63 cases 14 were diagnosed as malignant on cytology (22.2%, second most common category) which included spectrum of cases as shown in [Table/Fig-2]. This correlates well with the other studies [3,22-24]. Histopathological follow-up was available in 10 cases, out of which nine cases were confirmed to be malignant on histopathology. One case which was previously diagnosed at other institute on cytopathology as high grade malignant salivary gland tumour of parotid came to the authors department post radiation therapy with a swelling on the same site clinically suspicious of recurrence. At the authors department FNAC was performed and on cytology a diagnosis of recurrence of malignant salivary gland tumour was given, however on histopathology there was no evidence of malignancy. This misinterpretation of malignancy on cytology could be due to reactive atypia secondary to radiation therapy.
Limitation(s)
There were certain limitations in this study. One being histopathological association could not be obtained in all cases. The other limitation is comparatively smaller sample size. The present study along with other studies demonstrates that FNAC is reliable diagnostic tool for preoperative evaluation and management of salivary gland tumour. The current Milan system for reporting salivary gland cytopathology can provide better communication with clinicians and improved patient care by assessing the ROM in each category.
Conclusion(s)
The MSRSGC is a standardised reporting system for salivary gland FNAC. It is evidence based, effective and uniform system for salivary gland FNAC and it provides better communication with clinicians and helps in improving patient care. It also gives risk stratification by providing ROM in different categories. In this study, ROM was found correlating with the proposed ROM in Milan system in most categories except in AUS, SUMP and suspicious for malignancy. This was inferred to be because of the small sample size.