A Case Series on Epiploic Appendagitis: An Underdog in Acute Abdomen
Tharun Ganapathy Chitrambalam1, Pradeep Joshua Christopher2, Sudha Kanthasamy3, Jeyakumar Sundaraj4
1 Associate Professor, Department of General Surgery, SRM University, Chennai, Tamil Nadu, India.
2 Postgraduate Student, Department of General Surgery, SRM University, Chennai, Tamil Nadu, India.
3 Associate Professor, Department of Anatomy, SRM University, Chennai, Tamil Nadu, India.
4 Professor and Head, Department of General Surgery, SRM University, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Tharun Ganapathy Chitrambalam, SRM Nagar, Potheri, Kattankulathur, Chennai-603203, Tamil Nadu, India.
E-mail: catchpriya.29@gmail.com
Epiploic appendagitis is an uncommon yet a significant surgical diagnosis that every surgeon should be aware. It occurs due to the torsion of the epiploic appendage which gives rise to acute abdominal pain that can mimic other common causes of acute abdominal pain like appendicitis or cholecystitis. The treatment of epiploic appendagitis depend on clinical presentation, severity and it varies from conservative management to surgical excision. This case series is about eight patients presented with complaints of lower abdominal pain. After clinical examination they were initially diagnosed to have appendicitis or diverticulitis. The Computed Tomography (CT) based diagnoses were appendicitis, omental infarct, diverticulitis or epiploic appendagitis. All of them were subjected to diagnostic laparoscopy and found to have an inflammed epiploic appendage which was excised laparoscopically.
Appendicitis, Diverticulitis, Diagnostic Laparoscopy
Introduction
Epiploic appendages, otherwise called as the appendices epiploicae, consists of about 50-100 pedunculated pouches, each between 0.5-5 cm long, arranged in two rows parallel to the taenia coli. They are more concentrated on left side when compared to the right side along the serosal surface of the colon. They are attached to the colon by a vascular pedicle which comprises of two arterioles and a venule [1,2]. Epiploic appendages may cause inflammation, torsion, intrahernial content, obstruction, intraperitoneal loose bodies and also intussusception [2]. Mean age of diagnosis of this disease is 40 years and it is about four times more frequently seen in males than females [3]. They are either primary or secondary. Primary Epiploic Appendagitis (PEA) occurs mainly due to the torsion of the appendage and common sites include sigmoid colon and caecum, typically giving the patient pain in the left or right lower quadrant [1]. Secondary epiploic appendagitis is due to involvement of nearby organs, that are getting inflamed, like appendicitis, diverticulitis or cholecystitis [4].
Epiploic appendagitis is a rare cause of acute abdominal pain which is commonly underdiagnosed. This may resemble other causes of acute abdominal pain like appendicitis, diverticulitis, and cholecystitis making it one of the significant differentials [2]. In this case series among all the eight patients, the most common factor is that all of them presented with lower abdominal pain, left or right sided, and majority of them were taken to operating room without the diagnosis of epiploic appendagitis.
Case Series
This case series consists of eight patients that presented to the tertiary care hospital over a period of two years. The patients presented with focal right or left sided lower abdominal pain. The duration of pain varied from two to fifteen days, with a mean of seven days. The mean age was 41.3 years and there were four males and four females. Clinical examination findings and symptoms were typical for diverticulitis in two patients and acute appendicitis in the other six [Table/Fig-1]. None of the patients had similar episodes of abdominal pain in past nor had any previous abdominal surgeries.
Clinical, radiological and operative data of 8 patients with epiploic appendagitis.
| Case number | Age/sex | Site of pain | Clinical diagnosis | Radiologic diagnosis | Duration of pain (Days) | Operative diagnosis | Size (cms) | Localisation | Treatment |
|---|
| 1 | 43/F | RLQ | Acute appendicitis | Omental infarct | 15 | Epiploic appendagitis | 4.5×2 | Ascending colon | Laparoscopic excision of the EA |
| 2 | 55/F | RLQ | Acute appendicitis | Epiploic appendagitis with appendicitis | 3 | Epiploic appendagitis with appendicitis | 4×4 | Ascending colon | Laparoscopic excision of EA with appendicectomy |
| 3 | 32/F | LLQ | Diverticulitis | Fat stranding in LIF likely diverticulitis | 14 | Torsion epiploic appendage with fat stranding | 5×3 | Sigmoid colon | Laparoscopic excision of EA |
| 4 | 36/M | RLQ | Appendicitis | Omental infarct | 10 | Epiploic appendagitis | 4×4 | Caecum | Laparoscopic excision of EA |
| 5 | 40/M | LLQ | Diverticulitis | Epiploic appendagitis | 5 | Epiploic appendagitis | 4×6 | Sigmoid colon | Laparoscopic excision of EA |
| 6 | 35/F | RLQ | Appendicitis | Appendicitis | 3 | Epiploic appendagitis with acute appendicitis | 3×2 | Ascending colon | Laparoscopic excision of EA with appendicectomy |
| 7 | 50/M | RLQ | Appendicitis | Appendicitis | 2 | Epiploic appendagitis with acute appendicitis | 4×3 | Caecum | Laparoscopic excision of EA with appendicectomy |
| 8 | 40/M | RLQ | Appendicitis | Caecal epiploic appendagitis | 5 | Epiploic appendagitis with acute appendicitis | 4×3 | Caecum | Laparoscopic excision of EA with appendicectomy |
RLQ: Right lower quadrant; LLQ: Left lower quadrant; EA: Epiploic appendagitis
Investigations
All patients underwent a basic blood work up which includes complete haemogram, random blood sugar level, serum electrolytes and renal function test. Total 4/8 patients had leucocytosis. In all patients a CT scan of abdomen was done in addition to Ultrasonogram (USG) of abdomen and was started on broad spectrum antibiotics. USG and CT showed possibility of omental infarct in two patients, appendicitis in two, epiploic appendagitis in two, appendicitis with epiploic appendagitis in one and diverticulitis in one patient [Table/Fig-1].
Treatment
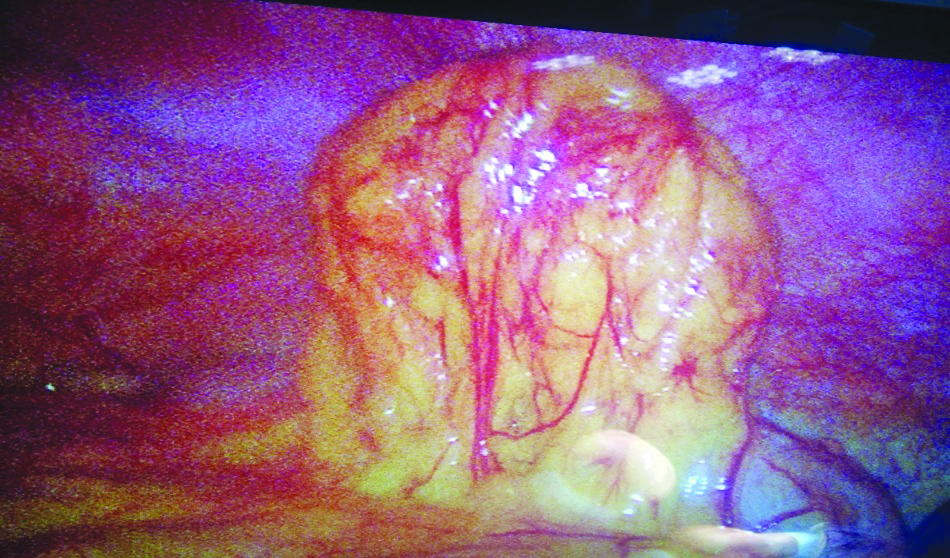
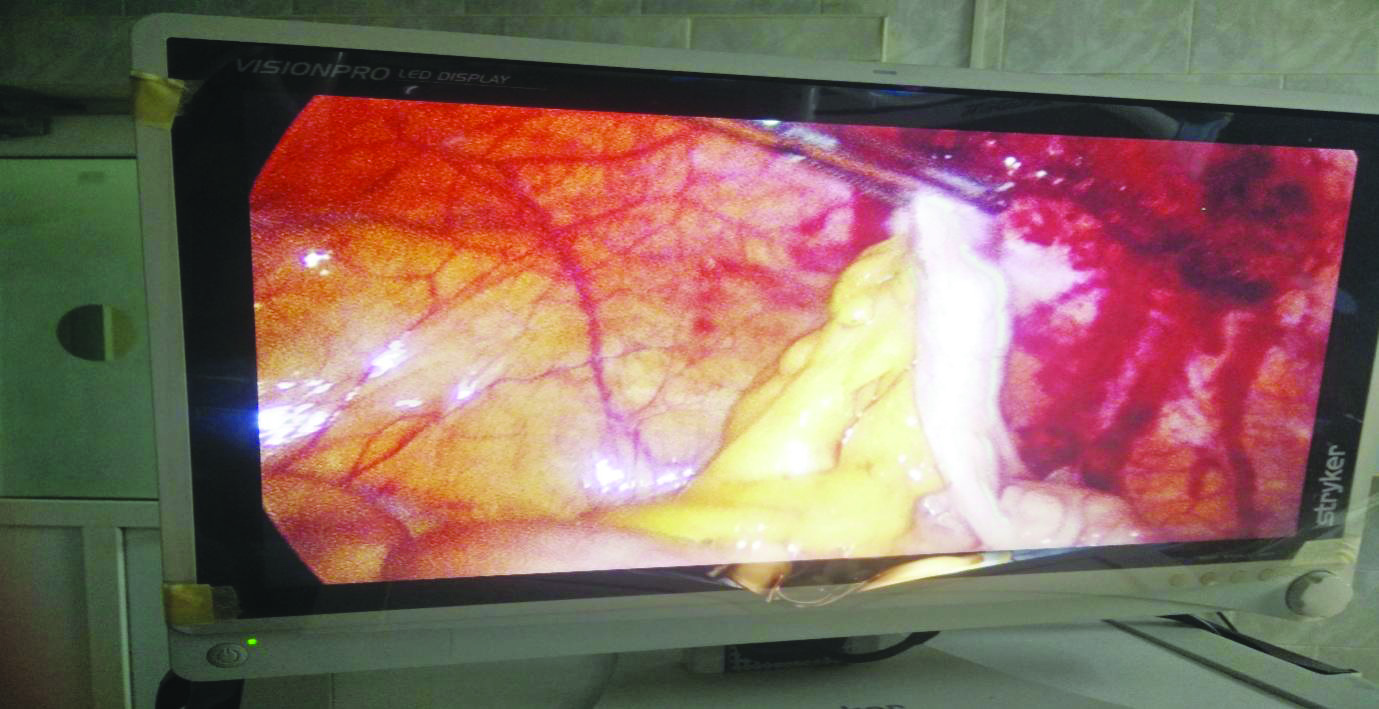
After obtaining anaesthetic assessment for surgery, all patients were subjected to a diagnostic laparoscopy, in view of confusing clinical presentation and radiological findings. On diagnostic laparoscopy, in all the patients epiploic appendagitis was noted, with origins from caecum (three patients), ascending colon (three patients) and sigmoid colon (two patients). Primary torsion of epiploic appendage was seen in 4/8 patients without any other pathology and underwent laparoscopic excision of epiploic appendagitis. Remaining four patients had evidence of acute appendicitis associated with torsion of adjacent epiploic appendage and underwent laparoscopic excision of epiploic appendagitis with appendicectomy [Table/Fig-2,3].
Inflamed epiploic appendage arising from ascending colon of patient no. 6.
Inflamed appendix in patient no. 6.
Outcome and Follow-up
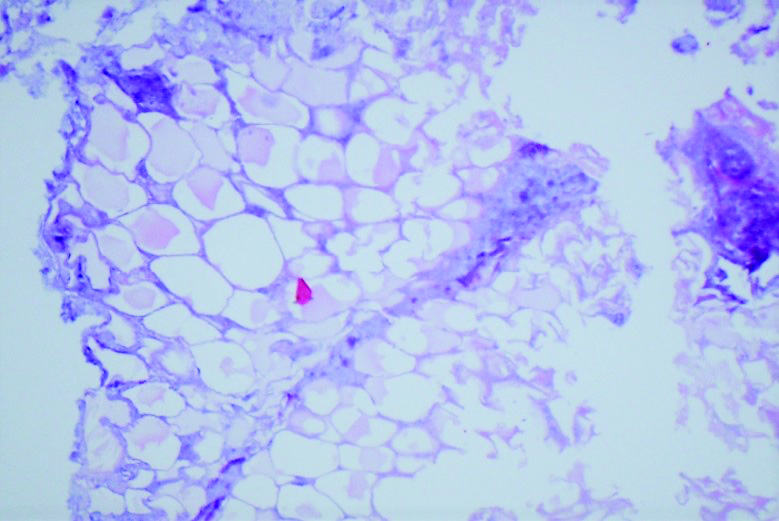
All patients recovered well postoperatively. Histopathological examination [Table/Fig-4] supported the intraoperative diagnosis in all patients as acute epiploic appendagitis and appendicitis. Patients were asymptomatic without any complaints post-surgery, on a mean follow-up period of 2 years.
Fat necrosis with fibrotic rim, consistent with infarcted epiploic appendage (Hematoxylin and Eosin stainX400) Patient no- 6.
Discussion
Epiploic appendages were first described by Vesalius in the year 1543. But it took until 1853 to get a surgical significance when Virchow suggested, their detachment can be a source of loose intraperitoneal bodies. In 1956, the term epiploic appendagitis was coined, the clinical diagnosis of which is very difficult as it lacks pathognomonic clinical features [5]. The pathophysiology behind the formation of appendagitis is the torsion of the vascular stalk of the appendage due to twisting, kinking or stretching along its long axis leading to ischaemia, venous thrombosis and necrosis [1,6]. The infarcted tissue can get calcified and appears as ‘peritoneal mice’ or ‘intraperitoneal loose bodies’, which are often an incidental finding on imaging. In rare cases, they can also get re-attached to the spleen and those are called ‘parasitised appendix epiploica’ [1].
This was initially an intraoperative finding in suspected cases of colonic diverticulitis or acute appendicitis, rather than a clinical diagnosis [7]. Due to the advent of CT, certain pathognomonic features were identified for inflamed appendage which is typically seen as a 1-4cm, oval shaped, fat density, paracolic lesion with adjacent fat stranding, bowel wall thickening and/or compression, thickened visceral and/or parietal peritoneum and central high-attenuating dot [7]. A review conducted by de Brito P et al., on an adult population presenting with abdominal pain and evaluated by CT over a three year period, showed that the frequency is about 1.3% and its incidence is 8.8/million/year [8]. If not evaluated properly and diagnosed early, the patients can end up in myriad complications like localised abscess, intussusception, obstruction and can also lead to peritonitis [6].
The management of this condition is still an unanswered question for many. Gandhi J and Gandhi N, reported that epiploic appendagitis can be managed with simple Non-Steroidal Anti-inflammatory Drugs (NSAIDs) without any surgical intervention [2]. However, conservative treatment of secondary epiploic appendagitis can be hazardous. Sand M et al., conservatively treated patients but the recurrence rate was found to be 40% [1]. Other case reports showed that the patients with primary epiploic appendagitis who were managed conservatively has no recurrences [9,10]. However, in cases of secondary epiploic appendagitis, it is ideal to atleast go ahead with a diagnostic laparoscopy, if not laparotomy to identify the pathology, as shown in this case series. The merit of minimal invasive surgery in diagnosing and treating the cases of acute abdominal pain of unclear aetiology is very well known.
All eight patients in this series underwent diagnostic laparoscopy due to the confusing clinical presentation and unmatched radiological correlation. On diagnostic laparoscopy, 4/8 patients were diagnosed as primary epiploic appendagitis and underwent laparoscopic excision of epiploic appendagitis. The remaining 4/8 patients was diagnosed as secondary epiploic appendagitis with concurrent acute appendicitis and underwent laparoscopic excision of epiploic appendagitis with appendicectomy. Laparoscopy bailed the surgeons out from missing a secondary cause of epiploic appendagitis and in confirming the same. Hence, it is recommended that laparoscopic approach be taken with clinical or radiological suspicion of epiploic appendagitis, both for diagnostic and therapeutic purpose.
Conclusion(s)
Epiploic appendagitis is an uncommon clinical condition with non specific symptoms, and diagnostic laparoscopy is helpful in both confirming the diagnosis and treating it. Although various case studies have emphasised Epiploic appendagitis as a self-limiting condition, the authors advised diagnostic laparoscopy for all suspected cases as recurrences are high and conservative treatment of secondary epiploic appendagitis can be hazardous. Laparoscopic intervention is appealing to both patient and surgeon as it offers excellent outcome and concurrent pathology if present, can be addressed in the same setting.
RLQ: Right lower quadrant; LLQ: Left lower quadrant; EA: Epiploic appendagitis
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 05, 2021
Manual Googling: Apr 14, 2021
iThenticate Software: Apr 28, 2021 (10%)
[1]. Sand M, Gelos M, Bechara FG, Sand D, Wiese TH, Steinstraesser L, Epiploic appendagitis-clinical characteristics of an uncommon surgical diagnosisBMC Surg 2007 7:1110.1186/1471-2482-7-1117603914 [Google Scholar] [CrossRef] [PubMed]
[2]. Gandhi J, Gandhi N, Epiploic appendagitisBMJ Case Reports 2009 :bcr012009141910.1136/bcr.01.2009.141921866238 [Google Scholar] [CrossRef] [PubMed]
[3]. Schnedl WJ, Krause R, Tafeit E, Tillich M, Lipp RW, Wallner-Liebmann SJ, Insights into epiploic appendagitisNat Rev Gastroenterol Hepatol 2011 8(1):45-49.10.1038/nrgastro.2010.18921102533 [Google Scholar] [CrossRef] [PubMed]
[4]. Subramaniam R, Acute appendagitis: Emergency presentation and computed tomographic appearancesEmerg Med J 2006 23(10):e5310.1136/emj.2005.03370416988291 [Google Scholar] [CrossRef] [PubMed]
[5]. Dockerty MB, Lynn TE, Waugh JM, A clinicopathologic study of the epiploic appendagesSurg Gynecol Obstet 1956 103(4):423-33. [Google Scholar]
[6]. Brady SC, Kliman MR, Torsion of the greater omentum or appendices epiploicaeCon J Surg 1979 22(1):79-82. [Google Scholar]
[7]. Rao PM, Rhea JT, Wittemberg J, Warshaw AL, Misdiagnosis of primary epiploic appendagitisAm J Surg 1998 176:81-85.10.1016/S0002-9610(98)00103-2 [Google Scholar] [CrossRef]
[8]. De Brito P, Gomez MA, Besson M, Scotto B, Huten N, Alison D, Frequency and epidemiology of primary epiploic appendagitis on CT in adults with abdominal painJournal de Radiologie 2008 89(2):23510.1016/S0221-0363(08)70399-8 [Google Scholar] [CrossRef]
[9]. Chu EA, Kaminer E, Epiploic appendagitis: A rare cause of acute abdomenRadiology Case Reports 2018 13(3):599-601.10.1016/j.radcr.2018.02.02230073043 [Google Scholar] [CrossRef] [PubMed]
[10]. Suresh Kumar VC, Mani KK, Alwakkaa H, Shina J, Epiploic appendagitis: An often misdiagnosed cause of acute abdomenCase Rep Gastroenterol 2019 13:364-68.10.1159/00050268331607837 [Google Scholar] [CrossRef] [PubMed]