Spinal Tuberculosis (TB) is the most common destructive form of extrapulmonary TB. The diagnosis of spinal TB is challenging involving combined approach of clinical diagnosis, imaging techniques, detection of Acid-Fast Bacilli (AFB) in microscopy, histopathology, and culture. This case series reports four patients of spinal TB diagnosed clinically, radiologically and microbiologically that were treated appropriately with standard anti-TB treatment according to Category I daily regimen.
Introduction
Spinal TB also known as Pott’s disease accounts for 1-2% of cases among 15-20% of extrapulmonary TB and almost half the cases of musculoskeletal TB [1,2]. It is more common in children and young adults. The incidence of spinal TB is increasing in developed countries [3]. To prevent and minimise the neurological morbidity associated with spinal TB, it is necessary to diagnose and treat it at the earliest [4]. Spinal involvement usually is a result of the haematogenous spread of Mycobacterium tuberculosis into the dense vasculature of cancellous bone of the vertebral bodies, although it is a fact that the primary infection site is usually either a pulmonary lesion or any infection of the genitourinary system [5,6].
Spinal TB is usually difficult to diagnose initially and may mimic pyogenic or malignancy in the initial stages. Most of the time, the patient presents at late stages where neurological involvement is prominent and would have crippled the patient, thus posing a challenge to the clinician despite all the technological advances which may eventually lead to severe skeletal deformities and irreversible neurological complications [7,8]. To overcome the challenge and/or the delay in the start of appropriate treatment the following case series highlights the need for the combination of clinical diagnosis, imaging techniques, and detection of acid-fast bacilli in microscopy, histopathology, and culture. Among the imaging techniques, Magnetic Resonance Imaging (MRI) is a more sensitive imaging technique than X-ray and more specific than Computed Tomography (CT). Above all, evidence also indicates that identification of AFB is very difficult in extrapulmonary TB due to its paucibacillary nature.
Case Series
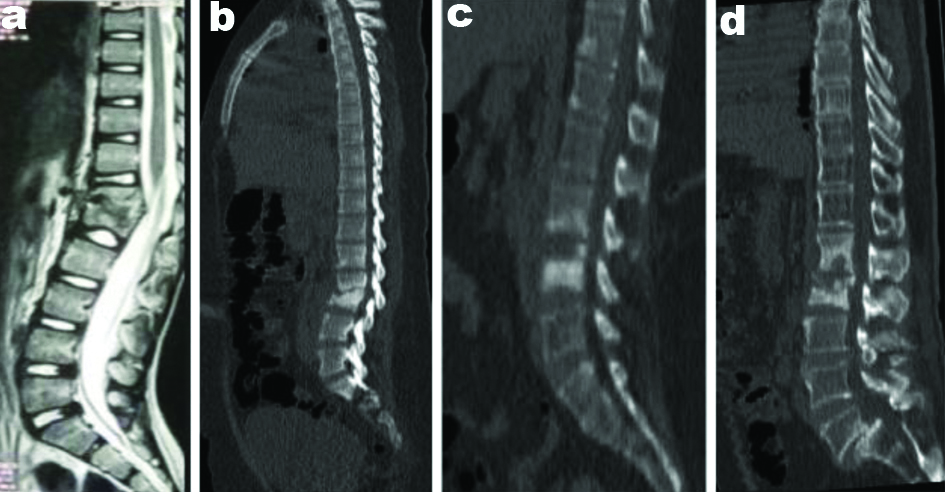
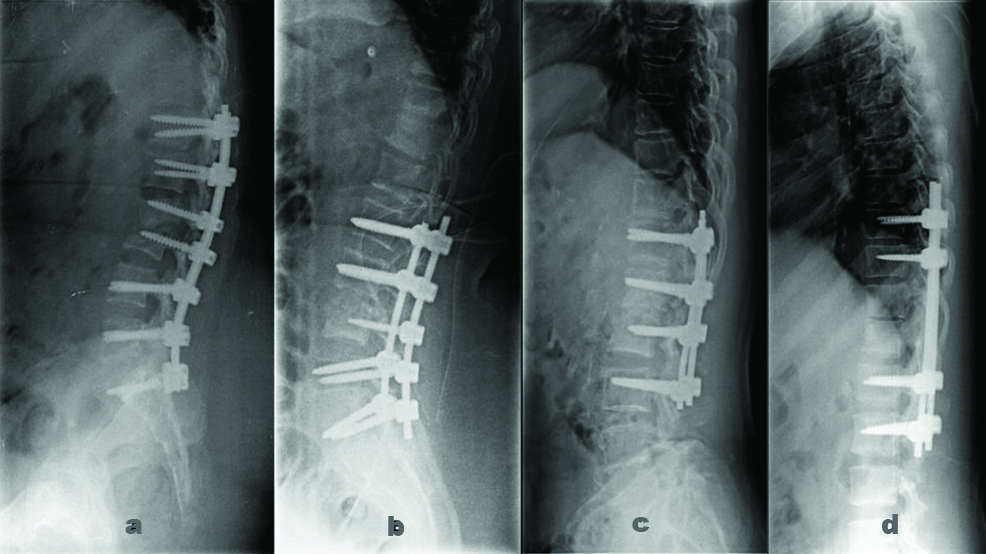
The preoperative images of the spine of all the four cases has been represented in [Table/Fig-1(a-d)]. And postoperative images of radiographic of all cases are shown in [Table/Fig-2(a-d)].
Mid sagittal of whole spine.
a. Case 1: T2 weighted MRI image showing D11-D12 vertebral body destruction.
b. Case 2: CT scan showing destruction of L2-L3 with local kyphosis.
c. CT scan showing spondylodiscitis of L3-L4.
d. Case 4: CT scan showing L1-L2 spondylodiscitis
Postoperative radiographs.
a. Case 1: Lumbosacral fixation- D9-D10 to L1-L2 with pedicle screws
b. Case 2: D12-S1 fixation with pedicle screws
c. Case 3: Posterior instrumentation with pedicle screws from L1-L5
d. Case 4: Thoracolumbar fixation with pedicle screws
Case 1
A 30-year-old female presented with a history of low backache for the past six months with fever headache and since one month was admitted to the hospital. There was no history of blurring of vision, limb weakness, tingling numbness, or seizures, no history of diabetes mellitus or hypertension.
Routine diagnostic parameters were within normal limits except Erythrocyte Sedimentation Rate (ESR) which was 96 mm/hour. MRI brain image showed multiple nodular lesions in the supra and infratentorial brain and brainstem. Likewise, the MRI of the spine revealed D11-D12 vertebral body destruction with anterior vertebral body collection [Table/Fig-1a]. The tentative clinical diagnosis recorded was TB granuloma of the brain lesions and TB abscess of spine lesions.
The patient underwent D9-D10 to L1-L2 fusion with wound debridement and posterior stabilisation [Table/Fig-2a]. The postoperative exudate was sent for routine bacteriology culture as well as Mycobacterium culture. Ziehl Neelsen (ZN) stain showed scanty AFB. The culture was positive for the Mycobacterium tuberculosis complex.
Case 2
A 28-year-old female with a history of low backache for nine months, which was insidious in onset and gradually progressive and was unable to walk. History revealed that the patient was diagnosed with TB spine nine months back elsewhere for which she had taken Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol for two months (intensive phase) followed by Isoniazid, Rifampicin for four months (continuation phase), and then the patient stopped treatment. The patient was feeling well during Anti TB Treatment (ATT) and after one month she developed increasing pain in the back associated with difficulty in walking after discontinuation of treatment. There was no history of diabetes mellitus or hypertension.
On examination, central tenderness over the lumbar spine extending from L1-L4 was present associated with an increase in paraspinal muscle tone. No sinus or scar was seen. Routine diagnostic parameters were within normal limits except ESR was 44 mm/hour. Mantoux test showed 18 mm induration after 48 hours. CT scan showed destruction of L2 and L3 vertebral bodies [Table/Fig-1b] with bilateral psoas abscess.
The patient was provisionally diagnosed as TB spine involving L2, L3, L4 with bilateral psoas abscess under the epidural collection. The patient was subjected to D12-S1 posterior instrumentation stabilisation with laminectomy [Table/Fig-2b]. Exudate and biopsy samples were sent for routine laboratory investigations. The culture was positive for the Mycobacterium tuberculosis complex. L2-L3 intervertebral disc biopsy was sent for histopathology examination which showed focal chronic inflammatory infiltrate with no evidence of TB.
Case 3
A 60-year-old female, with diabetes mellitus, presented with low backache for the past two months which was insidious on onset, gradually progressing with a history of radiating pain to the right lower limb with difficulty walking for the past one month. No history of trauma or history of TB or hypertension was revealed by the patient.
On examination, tenderness was present at L2-L3 vertebrae with a spasm of paraspinal muscles. Routine diagnostic parameters were within normal limits except ESR was 90 mm/hour. Mantoux test showed 21 mm induration after 48 hours. CT scan showed lumbar spondylosis with spondylodiscitis of L3-L4 [Table/Fig-1c].
The patient was subjected to L1-L5 posterior instrumentation and stabilisation with discectomy and fusion [Table/Fig-2c]. The tissue was sent for routine laboratory investigations. AFB culture was positive for Mycobacterium tuberculosis complex and also was confirmed by Cartridge Based Nucleic Acid Amplification Test (CBNAAT) which was sensitive to rifampicin. Histopathological Examination (HPE) of the biopsy sample from the disc showed features of acute on chronic non-specific inflammation.
Case 4
A 62-year-old male, with diabetes mellitus and Ischaemic Heart Disease (IHD), presented with low backache for three months, insidious on onset, progressive and radiating to both the lower limbs for the last 10-12 days. The patient had undergone radical subtotal gastrectomy and jejunostomy in 2017 and underwent chemotherapy and radiotherapy following surgery. The patient was admitted on and off with a history of low back pain. Relevant investigations were done and were within normal limits except ESR was 140 mm/hour. On examination, tenderness present over L1–S1 vertebrae with paraspinal tenderness. CT scan showed features suggestive of spondylodiscitis at L1-L2 [Table/Fig-1d] with postoperative status with grade 2 spondylolisthesis of L5 over S1 with L5 bilateral spondylolysis.
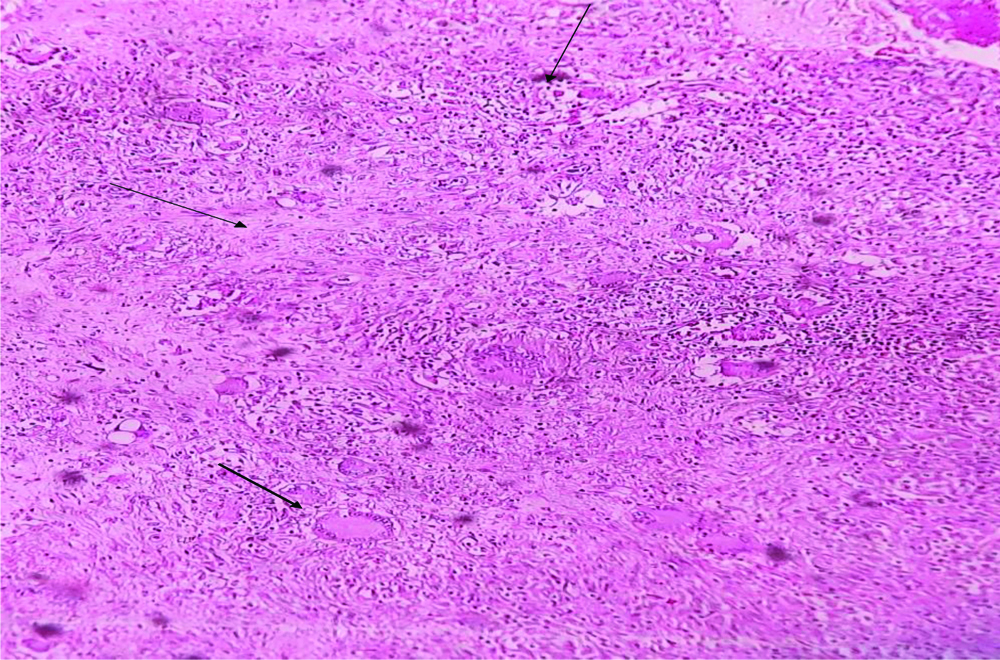
The patient was clinically diagnosed with L1-L2 spondylodiscitis, Koch’s/metastasis with L5-S1 spondylolisthesis with bilateral radiculopathy. He underwent D10-S1 posterior instrumentation with stabilisation with discectomy [Table/Fig-2d]. Biopsy and exudate sample sent for routine laboratory investigations. AFB culture were positive for Mycobacterium tuberculosis complex and also were confirmed by CBNAAT which was sensitive to rifampicin. Histopathological Examination (HPE) of L3-L4 spine tissue showed caseating TB [Table/Fig-3].
Histopathological Examination (HPE) of spine tissue showing granulomas with areas of caseation necrosis, epithelioid cells, Langahan’s, and foreign body giant cells H&E,10X.
ATT: Anti TB Treatment
Treatment: All the patients were treated based on category I daily regimen. The following anti-tubercular drugs were given- INH: Isoniazid (300 mg), R: Rifampicin (450 mg), Z: Pyrazinamide (1500 mg), E: Ethambutol (800 mg) [9]. The patients were treated with (HRZE) for four months followed by eight months of (HRE). The summary of all cases is listed in [Table/Fig-4].
Summary of the four cases.
| Case No. | Age/Sex | Clinical features | ESR/Other significant investigations | Microbiological and Pathological investigations | Radiological investigations | Site of involvement | Clinical diagnosis | Management |
|---|
| Case 1 | 30/Female | Low back pain.Fever and headache | 96 mm /hour.HIV, HBsAg, HCV: Non-reactive | AFB smear: positiveCulture: Positive | MRI Brain: Multiple nodular lesions in supra and infratentorial brain and brainstem.MRI Spine: D11-D12 vertebral body destruction with anterior body collection | Dorsal | TB granuloma of brain stem with TB abscess of spinal lesion | D9-D10 to L1-L2 fusion with wound debridement and posterior stabilisation.Category 1 ATT |
| Case 2 | 28/Female | Low back pain.Difficulty to walk | 44 mm/hour.HIV, HBsAg, HCV: Non-reactive | AFB smear: NegativeCulture: PositiveHPE: Chronic inflammation | CT scan: Destruction of L2-L3 vertebral bodies with bilateral psoas abscess | Lumbar with psoas abscess | TB spine involving L2, L3, L4 with bilateral psoas abscess under epidural collection | D12-S1 posterior instrumentation stabilisation with laminectomy. Category 1 ATT |
| Case 3 | 60/Female | Low back pain Difficulty in walking | 90 mm/hourMantoux: 21 mm induration after 48 hours.HIV, HBsAg, HCV: Non-reactive | Culture: PositiveCBNAAT: Mycobacterium tuberculosis detected and sensitive to RifampicinHPE: acute on chronic non-specific inflammation. | CT scan: lumbar spondylosis with spondylodiscitis of L3-L4. | Lumbar | L3-L4 Spondylodiscitis | L1-L5 posterior instrumentation and stabilisation with discectomy and fusion.Category 1 ATT |
| Case 4 | 62/Male | Low backache | 140 mm/hourHIV, HBsAg, HCV: Non-Reactive | AFB smear: NegativeCulture: PositiveCBNAAT: Mycobacterium tuberculosis detected and sensitive to Rifampicin.HPE: Caseating necrosis | CT scan: Features suggestive of spondylodiscitis at L1-L2 with postoperative status with grade 2 spondylolisthesis of L5 over S1 with L5 bilateral spondylolysis | Lumbar | L1-L2 spondylodiscitis, Koch’s/metastasis with L5-S1 spondylolisthesis with bilateral radiculopathy. | D10- S1 posterior instrumentation with stabilisation with discectomy.Category 1 ATT |
AFB (Acid-fast bacilli) smear=Ziehl Neelsen staining
Follow-up: The patients were followed-up monthly during treatment and again at the end of one and half year. Significant clinical improvement was seen in all cases. No relapse/no neurological deficit was revealed at the end of one and half years.
Discussion
The case series reveals that the progression of clinical features of spinal TB to be usually slow and insidious on onset as well as the duration of the illness varies from few months to years. It also reveals back pain to be the most frequent symptom of spinal TB associated with fever. The age range of patients with TB spondylitis was observed to be 28-60 years. All the cases were retrovirus negative which indicate adequate immunocompetency.
Spinal TB is a destructive form of TB that commonly affects thoracic and thoracolumbar segments with the initial destruction of vertebral bodies, with the occurrence of the paraspinal abscess also [3]. The chest X-ray was normal in all the above cases however, ESR was raised in all the above cases. Mantoux test was positive in two cases. In this series, diagnostic suspicion of TB spine could be confirmed with radiological features and laboratory investigations.
Computed tomography showed a degenerative process with spondylosis and spondylodiscitis, thus suggesting the need for CT to define the extent of the disease as it is supposed to be the best method to detect calcified foci [10]. Early surgery is indicated to ascertain the diagnosis of TB spine and also to confirm the aetiological agent by histopathology and microbiology. Debridement also reduces the bacterial load of the infected tissue [4]. Potential benefit of early surgery is a decline in neurological deficit. The degree of the fixation depends on the degree of destruction of bones (<50%), number of the levels involved and signs of instability [11]. Debridement of the infected tissue and stabilisation of the spine (spinal reconstruction) is a more extensive procedure and the reconstructions are performed with bone grafts or by using artificial materials like steel, carbon fiber, or titanium [12].
In this series, after obtaining informed and written consent debridement with posterior instrumentation with stabilisation by using titanium material was performed on the patients. Microbiological investigations of spinal TB were made with tissue/exudate conventional TB culture and CBNAAT [13]. One of the cases of HPE revealed caseating TB inflammation. Spinal TB once diagnosed by clinical and radiological ATT should be empirically started as early as possible before the aetiological diagnosis is confirmed. Duration of treatment remains controversial due to difficulty in assessing the response and risk of relapse, so most experts recommend 9-12 months of treatment [8]. In these cases, as there was no neurological deficit/impairment ATT was given for 12 months.
According to a study done by Patankar AP, it was shown that TB spine if treated timely and adequately the outcome comes relatively good. Decompression and fixation give a good result concerning neurological function [14]. One of the studies done by Alam MS et al., concluded that patients with spinal TB anterior debridement, auto graft bone fusion, anterior or posterior fixation appears to be effective in arresting the disease [15].
Conclusion(s)
The foregoing implies that the goal of TB spine should not only aim at eradicating the infection, but also in treating and preventing neurological complications. A high degree of a clinical index of suspicion is necessary for the diagnosis of spinal TB. Hence, tissue/exudate from the biopsy should always be subjected to staining, culture, HPE, and CBNAAT.
[1]. Patel R, Gannamani V, Shay E, Alcid D, Spinal tuberculosis and cold abscess without known primary disease: Case report and review of the literatureCase Rep Infect Dis 2016 2016:178015310.1155/2016/178015328070429 [Google Scholar] [CrossRef] [PubMed]
[2]. Garg RK, Malhotra HS, Kumar N, Spinal tuberculosis: Still a great mimicNeurol India 2019 67:1402-04.10.4103/0028-3886.27361831857523 [Google Scholar] [CrossRef] [PubMed]
[3]. Garg RK, Somvanshi DS, Spinal tuberculosis: A reviewJ Spinal Cord Med 2011 34(5):440-54.10.1179/2045772311Y.000000002322118251 [Google Scholar] [CrossRef] [PubMed]
[4]. Jain AK, Tuberculosis of the spine: A fresh look at an old diseaseJ Bone Joint Surg Br 2010 92(7):905-13.10.1302/0301-620X.92B7.2466820595106 [Google Scholar] [CrossRef] [PubMed]
[5]. Tuli SM, Tuberculosis of the shoulderTuberculosis of the skeletal system 1993 1st edNew DelhiJaypee Brothers Medical Publishers(P) Ltd [Google Scholar]
[6]. Boachie-Adjei O, Squillante RG, Tuberculosis of the spineOrthop Clin North Am 1996 27(1):95-103.10.1016/S0030-5898(20)32054-X8539058 [Google Scholar] [CrossRef] [PubMed]
[7]. Pellisé F, Tuberculosis and Pott’s disease, still very relevant health problemsEur Spine J 2013 22(Suppl 4):527-28.10.1007/s00586-012-2531-523053763 [Google Scholar] [CrossRef] [PubMed]
[8]. Lacerda C, Linhas R, Duarte R, Tuberculous spondylitis: A report of different clinical scenarios and literature updateCase Rep Med 2017 2017:416530110.1155/2017/416530129391868 [Google Scholar] [CrossRef] [PubMed]
[9]. Banga RK, Singh J, Dahuja A, Garg RS, Spinal tuberculosis- directly observed treatment and short course or daily anti tubercular therapy- are we over treating?Open Orthop J 2018 12:380-88.10.2174/187432500181201038030369990 [Google Scholar] [CrossRef] [PubMed]
[10]. Rivas-Garcia A, Sarria-Estrada S, Torrents-Odin C, Casas-Gomila L, Franquet E, Imaging findings of Pott’s diseaseEur Spine J 2013 22(Suppl 4):567-78.10.1007/s00586-012-2333-922684257 [Google Scholar] [CrossRef] [PubMed]
[11]. Phalak M, Kale SS, Tuberculosis of the thoracic spine- when and how to operateNeurol India 2019 5(1):01-14. [Google Scholar]
[12]. Jutte PC, van Loenhout-Rooyackers JH, Routine surgery in addition to chemotherapy for treating spinal tuberculosisCochrane Database Syst Rev 2006 (1):CD00453210.1002/14651858.CD004532.pub26532687 [Google Scholar] [CrossRef] [PubMed]
[13]. Parikh F, Basha J, Shah S, Bapat M, Diagnostic challenges in spinal tuberculosis and role of genexpert MTB/RIF Assay (Cartridge Based Nucleic Acid Amplification Test [CBNAAT])Open Forum Infectious Diseases 2015 2(1):58610.1093/ofid/ofv133.460 [Google Scholar] [CrossRef]
[14]. Patankar AP, Tuberculosis of spine: An experience of 30 cases over two yearsAsian J Neurosurg 2016 11(3):226-31.10.4103/1793-5482.14508527366249 [Google Scholar] [CrossRef] [PubMed]
[15]. Alam MS, Phan K, Karim R, Jonayed SA, Munir HK, Chakraborty S, Alam T, Surgery for spinal tuberculosis: A multi-center experience of 582 casesJ Spine Surg 2015 1(1):65-71.10.1055/s-0036-1582791 [Google Scholar] [CrossRef]