Elevation of Serum Cystatin C Levels as a Predictor of Cardiovascular Risk in Type 2 Diabetes Mellitus Patients: A Case-control Study
NS Sumantara1, MR Anusuya2
1 Assistant Professor, Department of Biochemistry, Rajarajeswari Medical College and Hospital, Bangalore, Karnataka, India.
2 Professor, Department of Biochemistry, Kempegowda Institute of Medical Sciences, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. NS Sumantara, Rajarajeswari Medical College and Hospital, #202, Kambipura, Mysore Road, Bangalore-560074, Karnataka, India.
E-mail: sumantara90@gmail.com
Introduction
Patients with type 2 Diabetes Mellitus (DM) exhibit atherogenic lipid profile, increasing the risk for atherosclerosis, compared to people without diabetes. Cystatin C, a naturally occurring protease inhibitor has a key role in pathogenesis of atherosclerosis in type 2 DM patients by inhibiting the elastolytic activity of arterial extracellular matrix by cysteine protease cathepsins. Increased concentration of cystatin C in serum reflects a counterbalance of the damaging elastolytic activity which is involved in the pathogenesis of atherosclerosis in type 2 DM patients.
Aim
To determine the serum levels of cystatin C and lipid profile in type 2 DM patients with good and poor glycaemic control and to find out the correlation between serum cystatin C with HbA1c levels and cardiovascular risk markers (non-High-Density Lipoprotein Cholesterol (HDLc), Total Cholesterol (TC)/HDLc, Low-Density Liporotein (LDLc)/HDLc).
Materials and Methods
The present case-control study included 60 diabetic patients of 35-75 years of age including both the genders. They were divided into Group A (n=30) with HbA1c ≤6.5% and Group B (n=30) with HbA1c >6.5%. Blood samples were collected in fasting state and analysed for Fasting Blood Sugar (FBS), TC, HDLc, LDLc. FBS was analysed by Hexokinase method, HbA1c by turbidimetric inhibition immunoassay and cystatin C by Immunoturbidimetric method. Other parameters like Non-HDLc and cardiovascular risk ratios TC/HDLc and LDLc/HDLc were calculated. Statistical analysis was done by student’s t-test and statistical significance was established at p-value <0.0001. Pearson’s correlation coefficient was used to examine various parameters.
Results
In the present study, it was found that diabetic patients with HbA1c >6.5% showed increased levels of serum cystatin C (1.20±0.73 mg/L), TC (182±46.48 mg/dL), LDLc (137±13.86 mg/dL) and low levels of HDLc (34.7±12.43 mg/dL) compared to diabetic patients with HbA1c ≤6.5%. Increase in serum cystatin C levels correlated well with the increased levels of HbA1c (r=0.92), non-HDLc (r=0.87) and cardiovascular risk ratios like TC/HDLc (r=0.95) and LDLc/HDLc (r=0.97).
Conclusion
The elevated serum levels of cystatin C levels correlated well with increased HbA1c and lipid profile indicating the dyslipidemia and proatherogenic status in type 2 diabetic patients with poor glycaemic control. Thus, cystatin C can be considered as the predictive marker for cardiovascular disease in type 2 diabetic patients.
Atherosclerosis, Cathepsins, Dyslipidemia, Glycaemic control, Hyperglycaemia
Introduction
Hyperglycaemia in diabetic individuals induces a large number of alterations at cellular levels of vascular system [1]. Studies have reported that long term hyperglycaemia also results in dyslipidemia in diabetic patients [2-4]. Diabetic people associated with dyslipidemia are at increased risk for cardiovascular disease [5,6].
Studies have reported that high cystatin C concentration is directly related to inflammation and atherosclerosis [7-9]. Cystatin C is a nonglycosylated 13kDa basic protein belonging to the cystatin superfamily of cytokine protease inhibitors [10,11]. Cysteine protease-cathepsins are a group of proteolytic enzymes which includes cathepsins like B, H, S, L and C that are involved in pathological mechanisms like inflammation, tumour invasion, breakdown of collagen and bone resorption [5,7]. Cystatin C is a naturally occurring protease inhibitor [12]. Cathepsin S has elastolytic and collagenolytic properties and plays a role in extracellular matrix remodeling by the degradation of matrix proteins. Mechanism of atherosclerosis is the local imbalance between elastolytic activity of cathepsins and their inhibitor cystatin C promotes neovascularisation leading to micro vessel formation and recruitment of inflammatory cells with accumulation of plasma lipids, thus it has a clear effect on cardiovascular system [7,8,11].
Increased serum cystatin C may be a part of regulatory mechanisms engaged to control the proatherogenic capacity of specific cathepsins such as cathepsin S. Studies have reported that patients with higher circulating cystatin C concentration have an increased cardiovascular risk profile [7,12,13]. Cystatin C levels are prognostic markers that can be useful as risk assessment tool in cardiovascular diseases [14-16]. The impact of increased levels of cystatin C has a profound impact on the risk of fatal cardiovascular disease [17-20]. Since, cystatin C correlated well with cardiovascular risk factors in patients with poor glycaemic control, this study was undertaken to verify and confirm the available data and to substantiate that cystatin C is a biomarker of cardiovascular risk in patients of type 2 DM.
Materials and Methods
A case-control study was carried out on 60 diabetic subjects, from outpatient and inpatient wards, Department of Medicine of Kempegowda Institute of Medical Sciences and Hospital, Bengaluru, Karnataka, India. The study subjects were divided into cases and controls of 30 each and informed consent was obtained from the patients. The Ethical clearance was obtained from the Institutional Ethical committee (Ref No.: KIMS/IEC/A31-2016). The study period was from October 2016-January 2017.
Inclusion criteria: Type 2 DM established according to the criteria of American Diabetes Association, patients of age group 35-75 years with duration of history of DM between 1-5 years and on treatment with oral hypoglycaemic drugs/insulin/both were recruited [21].
Exclusion criteria: Patients with type 1 DM, cardiac diseases, renal diseases and patients on hypolipidemic drugs were excluded from the study.
The study population was grouped into:
Group A as controls which included 30 Type 2 DM patients with HbA1c ≤6.5% (good glycaemic control).
Group B as cases which included 30 Type 2 DM patients with HbA1c >6.5% (poor glycaemic control).
Laboratory Analysis
Under aseptic precautions, 5 mL of blood sample was drawn after 10 hours of overnight fasting. This was followed by centrifugation and then the sample was processed immediately.
The serum samples were analysed in Cobas 6000 autoanalyser for FBS by Hexokinase method. Serum cystatin C by immunoturbidimetric method and lipid profile by enzymatic colorimetric method. The third Adult Treatment Panel III (ATP III) of the National Cholesterol Education Program (NCEP) guidelines was referred [22]. According to NCEP, TC >200 mg/dL, LDL >130 mg/dL and HDL <40 mg/dL is considered as risk for Cardiovascular Heart Disease (CHD). Dyslipidemia was defined if there is presence of one or more than one abnormal serum lipid concentration. HbA1c was measured by turbidimetric inhibition immunoassay in whole blood. HbA1c was expressed as percentage (%) according to National Glycohaemoglobin Standardisation Program (NGSP). Values of all the other parameters were given in mg/dL. Non-HDLc and cardiovascular risk ratios TC/HDLc and LDLc/HDLc were calculated.
Statistical Analysis
Statistical analysis was done by student’s t-test and results were expressed as mean±standard deviation (SD). The data was evaluated by GraphPad software version Prism 7.0. Statistical significance was established at p-value <0.0001. Pearson’s correlation coefficient was used to examine various parameters. The results were considered statistically not significant when p-value was >0.05. Graphical data was presented in scatter plot.
Results
The mean age of the group A was (53.43±12.21) years and group B was (49.23±7.98) years. The demographic parameters did not show statistically significant results as shown in [Table/Fig-1].
Demographic parameters of the study subjects.
| Variables | Group A (n=30) | Group B (n=30) | p-value |
|---|
| Gender (M/F) | 9/21 | 13/17 | ------ |
| Age (years) | 53.43±12.21 | 49.23±7.98 | 0.12 |
In [Table/Fig-2], Group B patients showed statistically highly significant values for serum cystatin C levels, HbA1c, non HDLc, TC/HDLc and LDLc/HDLc with p value <0.0001. Among the circulating lipids, LDLc and non-HDLc were significantly higher in group B patients compared to group A patients.
Mean and Standard deviation of study parameters in Group A and Group B.
| Parameters | Group A (Mean±SD) | Group B (Mean±SD) | t-value | p-value |
|---|
| FBS (mg/dL) | 91±15.15 | 191±60.27 | 8.81 | <0.0001 |
| HbA1c (%) | 5.23±0.84 | 10.19±2.13 | 11.86 | <0.0001 |
| Total cholesterol (mg/dL) | 160±44.03 | 182±46.48 | 1.88 | 0.064 |
| HDL cholesterol (mg/dL) | 56.66±9.1 | 34.7±12.43 | 7.80 | <0.0001 |
| LDL cholesterol (mg/dL) | 102.9±39.10 | 137±13.86 | 4.50 | <0.0001 |
| Non-HDL cholesterol (mg/dL) | 125±35 | 175.9±33.6 | 5.74 | <0.0001 |
| TC/HDLc | 2.9±0.96 | 5.95±2.33 | 6.62 | <0.0001 |
| LDLc/HDLc | 1.88±2.02 | 4.39±2.57 | 4.20 | <0.0001 |
| Cystatin C (mg/L) | 0.55±0.26 | 1.20±0.73 | 4.59 | <0.0001 |
p-value <0.0001 was considered statistically significant
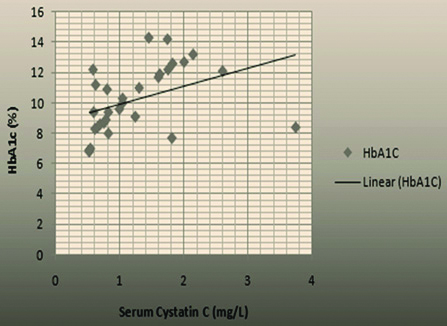
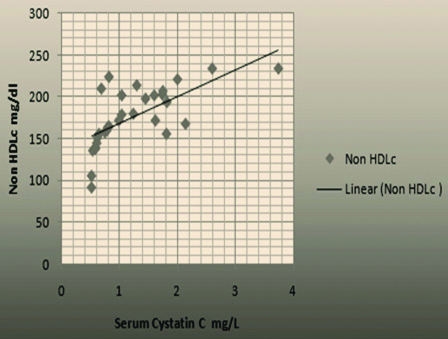
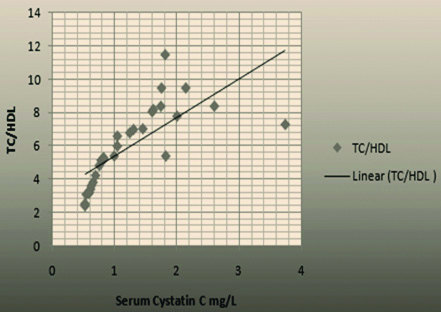
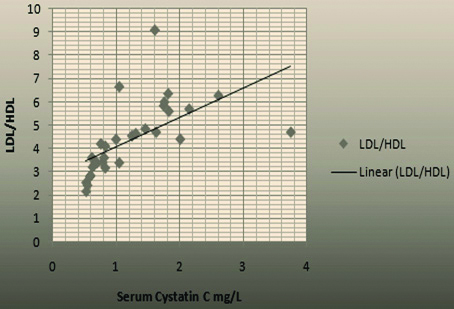
The [Table/Fig-3] showed positive Pearson’s correlation coefficient between serum cystatin C levels with study parameters like HbA1c with r-value 0.92, Non-HDLc with r-value 0.87 and cardiovascular risk ratios like TC/HDLc with r-value 0.95 and LDLc/HDLc with r-value 0.97 and results were considered significant when p-value <0.0001.
Pearson’s correlation coefficient of serum cystatin C levels with study parameters.
| Parameters | p-value | r-value |
|---|
| Serum cystatin C with HbA1c | <0.0001 | 0.92 |
| Serum cystatin C with Non-HDLc | <0.0001 | 0.87 |
| Serum cystatin C with TC/HDLc | <0.0001 | 0.95 |
| Serum cystatin C with LDLc/HDLc | <0.0001 | 0.97 |
p-value <0.0001 was considered statistically significant
The [Table/Fig-4,5,6, and 7] showed the scatter plots drawn for the parameters HbA1c, Non HDLc, TC/HDLc and LDLc/HDLc showing significant positive correlation with serum cystatin C.
Graph showing pearson’s correlation between serum cystatin C and HbA1c of the subjects.
Graph showing pearson’s correlation between serum cystatin C and Non-HDLc of the subjects.
Graph showing pearson’s correlation between Serum cystatin C and TC/HDLc of the subjects.
Graph showing pearson’s correlation between Serum cystatin C and LDLc/HDLc of the subjects.
Discussion
In the present study, serum cystatin C was found to be increased in type 2 DM with poor glycaemic status and it correlated well with the increased levels of HbA1c (r=0.92), suggesting that elevated cystatin C concentration is directly related to the increased elastolytic activity of cysteine proteases and progression in the pathogenesis of atherosclerosis which is in accordance with the study done by Senghor A et al., [5].
Mahato RV et al., also showed that diabetic patients with poor glycaemic control exhibited significant increase in TC, LDLc, Non-HDLc and risk ratios when compared with patients of good glycaemic control [6]. In the present study, it was showed that the severity of cardiovascular risk associated with dyslipidemia increases with elevated HbA1c levels, which is in accordance with few other studies too [23-26]. Non-HDLc was significantly correlated with cystatin C levels (r=0.87). Lu W et al., also showed that non-HDLc as a strong predictor of cardiovascular disease in diabetic patients [27]. Since, non-HDLc can be measured in a non-fasting state, it has great value in determining dyslipidemia in diabetic patients. According to NCEP Adult Treatment Panel III, Non-HDLc is recommended to assess the cardiovascular risk in diabetic patients [22,27].
The risk ratios like TC/HDLc and LDLc/HDLc showed good positive correlation with cystatin C in the present study, which was in accordance to studies done by Triki S et al., Angelidis C et al., and Mohamed WM et al., [28-30]. Gimeno-Orna JA et al., showed TC/HDLc ratio as predictor of cardiovascular events and concluded that TC/HDLc ratio can be used as a treatment guide for diabetic dyslipidemia [2]. Khan HA et al., have found that LDLc/HDLc has strong relation with the cardiovascular disease [23].
Hence, based on the results derived from the present study, it can be concluded that an increase in serum cystatin C will help in the assessment of proatherogenic status in diabetic patients with poor glycaemic control. Thus, cystatin C can be considered as the predictor for cardiovascular risk in type 2 diabetic patients.
Limitation(s)
Due to time constraints a convenient sample size of 60 was selected for the study. It was found that, the lipid parameters were also significantly elevated along with the cystatin C levels in diabetic patients with poor glycaemic control. So, further studies are needed with large sample size to evaluate the role of cystatin C in development of atherosclerosis.
Conclusion(s)
In the study, higher serum cystatin C levels correlated well with increased HbA1c and lipid profile indicating the dyslipidemia and proatherogenic status in type 2 DM patients. Hence, cystatin C behaves as a predictor of cardiovascular risk in type 2 DM patients helping physicians to take appropriate measures to prevent the occurrence of cardiovascular disease in diabetic patients. Further studies on a larger sample size are required for the detailed evaluation of possible role of serum cystatin C levels as predictor of cardiovascular risk in type 2 DM patients.
p-value <0.0001 was considered statistically significant
p-value <0.0001 was considered statistically significant
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 21, 2020
Manual Googling: Mar 19, 2021
iThenticate Software: Apr 24, 2021 (19%)
[1]. Aronson D, Rayfield EJ, How hyperglycemia promotes atherosclerosis: Molecular mechanismsCardiovasc Diabetol 2002 1(1):110.1186/1475-2840-1-112119059 [Google Scholar] [CrossRef] [PubMed]
[2]. Gimeno-Orna JA, Faure-Nogueras E, Sancho-Serrano MA, Usefulness of total cholesterol/HDL-cholesterol ratio in the management of diabetic dyslipidaemiaDiabet Med 2005 22(1):26-31.10.1111/j.1464-5491.2004.01341.x15606687 [Google Scholar] [CrossRef] [PubMed]
[3]. Das B, Evaluation of Cystatin C as a predictor of Coronary artery disease in type 2 DiabetesIOSR-JDMS 2013 11(1):53-60.10.9790/0853-1115360 [Google Scholar] [CrossRef]
[4]. Grubb A, Diagnostic value of analysis of cystatin C and protein HC in biological fluidsClin Nephrol 1992 38(Suppl 1):S20-27. [Google Scholar]
[5]. Senghor A, William E, Naveen C, Krishnan MS, Correlation of Cystatin C and Cardiovascular risk makers in uncontrolled type 2 DMIJPCR 2013 5(2):79-82. [Google Scholar]
[6]. Mahato RV, Prajwal G, Pramod R, Prashant R, Khelanand S, Dipendra RP, Association between glycaemic control and serum lipid profile in type 2 diabetic patients: Glycated haemoglobin as a dual biomarkerBiomedical Research 2011 22:375-80. [Google Scholar]
[7]. Taglieri N, Koenig W, Kaski JC, Cystain C and cardiovascular riskClin Chem 2009 55:1932-43.10.1373/clinchem.2009.12839719713275 [Google Scholar] [CrossRef] [PubMed]
[8]. Selvin E, Marinopoulos S, Berkenblit G, Rami T, Brancati FL, Powe NR, Meta-analysis: Glycosylated hemoglobin and cardiovascular disease in diabetes mellitusAnn Intern Med 2004 141(6):421-31.10.7326/0003-4819-141-6-200409210-0000715381515 [Google Scholar] [CrossRef] [PubMed]
[9]. Yamashita H, Nishino T, Obata Y, Nakazato M, Inoue K, Furusu A, Association between cystatin C and arteriosclerosis in the absence of chronic kidney diseaseJ Atheroscler Thromb 2013 20(6):548-56.10.5551/jat.1319323574755 [Google Scholar] [CrossRef] [PubMed]
[10]. Shlipak MG, Sarnak MJ, Katz R, Fried LF, Seliger SL, Newman AB, Cystatin C and the risk of death and cardiovascular events among elderly personsN Engl J Med 2005 352(20):2049-60.10.1056/NEJMoa04316115901858 [Google Scholar] [CrossRef] [PubMed]
[11]. Bhat K, Lal AK, Ahmad S, Kakkar M, Cystatin C: An early marker of cardiac complications in diabeticsActa Med Int 2015 2(1):84-86.10.5530/ami.2015.1.13 [Google Scholar] [CrossRef]
[12]. Chung YK, Lee YJ, Kim KW, Cho RK, Chung SM, Moon JS, Serum cystatin C is associated with subclinical atherosclerosis in patients with type 2 diabetes: A retrospective studyDiab Vasc Dis Res 2018 15(1):24-30.10.1177/147916411773815629090609 [Google Scholar] [CrossRef] [PubMed]
[13]. Sukhova GK, Shi GP, Simon DI, Chapman HA, Libby P, Expression of the elastolytic cathepsin S and K in human atheroma and regulation of their production in smooth muscle cellsJ Clin Invest 1998 102(3):576-83.10.1172/JCI1819691094 [Google Scholar] [CrossRef] [PubMed]
[14]. Lee SH, Lee KW, Kim ES, Park YR, Kim HS, Shin AP, Cystatin C is a valuable marker for predicting future cardiovascular disease in type 2 diabetic patientsKorean Diabetes J 2008 32(6):488-97.10.4093/kdj.2008.32.6.488 [Google Scholar] [CrossRef]
[15]. Chen S, Tang Y, Zhou X, Cystatin C for predicting all-cause mortality and rehospitalization in patients with heart failure: A meta-analysisBiosci Rep 2019 39(2):BSR2018176110.1042/BSR2018176130643006 [Google Scholar] [CrossRef] [PubMed]
[16]. Einwoegerer CF, Domingueti CP, Association between increased levels of Cystatin C and the development of cardiovascular events or mortality: A systematic review and meta-analysisArq Bras Cardiol 2018 111(6):796-807.10.5935/abc.2018017130281693 [Google Scholar] [CrossRef] [PubMed]
[17]. Meng L, Yang Y, Qi LT, Wang XJ, Xu GB, Zhang BW, Elevated serum cystatin C is an independent predictor of cardiovascular events in people with relatively normal renal functionJ Nephrol 2012 25(3):426-30.10.5301/jn.500002021928225 [Google Scholar] [CrossRef] [PubMed]
[18]. Zhao M, Che Q, Zhang Y, Qian X, Huang T, Expression and clinical significance of serum cystatin C in patients with hypertension and coronary heart diseaseMedicine (Baltimore) 2020 99(22):e2002910.1097/MD.000000000002002932481372 [Google Scholar] [CrossRef] [PubMed]
[19]. Yang X, Lin Q, Li X, Wu L, Xu W, Zhu Y, Cystatin C is an important biomarker for cardiovascular autonomic dysfunction in Chinese type 2 diabetic patientsJ Diabetes Res 2019 2019:170696410.1155/2019/170696431011584 [Google Scholar] [CrossRef] [PubMed]
[20]. Cepeda J, Tranche-Iparraguirre S, Marín-Iranzo R, Fernández-Rodríguez E, Riesgo-García A, García-Casas J, Cystatin C and cardiovascular risk in the general populationRev Esp Cardiol 2010 63(4):415-22.10.1016/S0300-8932(10)70062-2 [Google Scholar] [CrossRef]
[21]. American Diabetes AssociationDiagnosis and classification of Diabetes MellitusDiabetes Care 2019 33:62-69.10.2337/dc10-S06220042775 [Google Scholar] [CrossRef] [PubMed]
[22]. Lipsy RJ, The National Cholesterol Education Program Adult Treatment Panel III guidelinesJ Manag Care Pharm 2003 9(1 Suppl):02-05. [Google Scholar]
[23]. Khan HA, Sobki SH, Khan SA, Association between glycaemic control and serum lipids profile in type 2 diabetic patients: HbA1c predicts dyslipidaemiaClin Exp Med 2007 7(1):24-29.10.1007/s10238-007-0121-317380302 [Google Scholar] [CrossRef] [PubMed]
[24]. Lee M, Saver JL, Huang WH, Chow J, Chang KH, Ovbiagele B, Impact of elevated cystatin C level on cardiovascular disease risk in predominantly high cardiovascular risk populations: A meta-analysisCirc Cardiovasc Qual Outcomes 2010 3(6):675-83.10.1161/CIRCOUTCOMES.110.95769620923994 [Google Scholar] [CrossRef] [PubMed]
[25]. Nosaka K, Nakamura K, Kusano K, Toh N, Tada T, Miyoshi T, Serum cystatin C as a biomarker of cardiac diastolic dysfunction in patients with cardiac disease and preserved ejection fractionCongest Heart Fail 2013 19(4):35-39.10.1111/chf.1203923910705 [Google Scholar] [CrossRef] [PubMed]
[26]. Kobayashi T, Yokokawa H, Fujibayashi K, Haniu T, Hisaoka T, Fukuda H, Association between high cystatin C levels and carotid atherosclerosisWorld J Cardiol 2017 9(2):174-81.10.4330/wjc.v9.i2.17428289532 [Google Scholar] [CrossRef] [PubMed]
[27]. Lu W, Resnick HE, Jablonski KA, Jones KL, Jain AK, Howard WJ, Non-HDL cholesterol as a predictor of cardiovascular disease in type 2 diabetes: The strong heart studyDiabetes Care 2003 26(1):16-23.10.2337/diacare.26.1.1612502653 [Google Scholar] [CrossRef] [PubMed]
[28]. Triki S, Fekih O, Hellara I, Neffati F, Douki W, Ben Hamda K, Association between serum cystatin C levels and cardiovascular disease in type 2 diabetic patientsAnn Biol Clin 2013 71(4):438-42.10.1684/abc.2013.085723906571 [Google Scholar] [CrossRef] [PubMed]
[29]. Angelidis C, Deftereos S, Giannopoulos G, Anatoliotakis N, Bouras G, Hatzis G, Cystatin C: An emerging biomarker in cardiovascular diseaseCurr Top Med Chem 2013 13(2):164-79.10.2174/156802661131302000623470076 [Google Scholar] [CrossRef] [PubMed]
[30]. Mohamed WM, Waleed AI, Said SM, Cystatin C in patients with coronary artery diseaseInterv Cardiol J 2019 7(3):96 [Google Scholar]