Poncet’s Disease Revisited
Mini Bhatnagar1, Bimal K Agrawal2, C Srivatsa3, Dil Preet Reehal4, Jaskaran Bazad5
1 Professor, Department of General Medicine, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India.
2 Professor and Principal, Department of General Medicine, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India.
3 Postgraduate Student, Department of General Medicine, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India.
4 Intern, Department of General Medicine, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India.
5 Postgraduate Student, Department of General Medicine, Maharishi Markandeshwar Institute of Medical Sciences and Research, Mullana, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mini Bhatnagar, #930, Sector 40 A, Chandigarh, India.
E-mail: drshyamini@yahoo.com
Tuberculosis (TB) is one of the most dreaded diseases prevalent in developing countries. Though primarily affecting the lungs, TB can affect almost any part of the body. The musculoskeletal system is the fourth most common extra-pulmonary target, after pleural, lymphatic and genitourinary system. Poncet’s Disease aka Tuberculous Rheumatism is a rare rheumatologic association of active Extra Pulmonary TB (EPTB) which may be easily missed/misdiagnosed even though TB is frequently encountered in medical practice. The authors present the case of an adolescent 18-year-old male who presented with subacute symmetrical inflammatory arthritis of lower extremities. Investigations ruled out other rheumatological conditions. He recovered completely after receiving Antitubercular Treatment (ATT) for abdominal TB, which was diagnosed during workup.
Arthritis, Reactive, Tuberculosis, Tuberculous rheumatism
Case Report
An 18-year-old male visited the Medicine Department with complaints of generalised weakness since two months. The weakness was accompanied by decreased appetite, significant weight loss, fever and constipation. In addition, patient had difficulty in walking due to bilateral ankle, feet pain and swelling in ankle joints. The swelling which started six weeks ago progressed over time and was aggravated by physical activity. He had received Nonsteroidal Anti-Inflammatory Drugs (NSAIDS) for about one month with no relief in symptoms. He denied any respiratory symptoms or history of trauma. He did not have any past history of diabetes, TB, or asthma. According to his father, the patient’s childhood immunisations including Bacillus the Calmette-Guérin (BCG) vaccine at birth were complete. Furthermore, there was no family history of TB, rheumatologic or autoimmune diseases. However, one person in the neighborhood had received ATT in recent past.
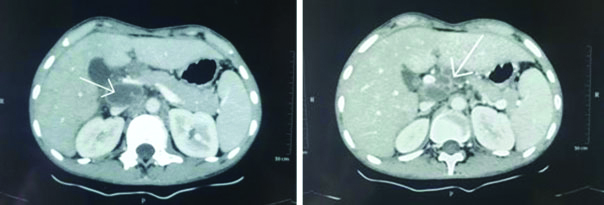
The patient’s pulse and blood pressure were within normal limits. He was febrile (101°F) and weighed 34 kg. On further examination, mild pallor. Bilateral inguinal lymphadenopathy was present lymph nodes measuring 1.5×1 cm. Both ankle joints, metatarsophalangeal and intertarsal joints were swollen and tender. Bilateral joints showed restricted painful movement. There was painful swelling extending from the lateral malleoli to distal part of the ankle joints. Rest of the physical examination was unremarkable. Laboratory investigations revealed an elevated Erythrocyte Sedimentation Rate (ESR) (90 mm/hour), alkaline phosphatase (377 IU/L), and aspartate aminotransferase (AST) (87 U/L). His hemoglobin was 10.6 mg/dL with peripheral blood film displaying microcytic hypochromic anaemia. A Purified Protein Derivative (PPD) skin test resulted in induration of 18 mm at 48 hours. Ultrasound of whole abdomen [Table/Fig-1] was suggestive of abdominal lymphadenopathy. Subsequently, Contrast-Enhanced Computed Tomography (CECT) [Table/Fig-2] showed extensive necrotic abdominopelvic lymphadenopathy with peritoneal and omental thickening along with thickening of terminal ileum causing luminal narrowing with mild upstream bowel dilation (partial stricture formation); findings were suggestive of tubercular aetiology. Electrocardiogram and chest X-ray (Posteroanterior view) was normal. X-ray of the ankle joint and feet revealed no abnormalities. Rheumatoid Factor (RF), Anti Cyclic Citrullinated Peptide (CCP), Antinuclear Antibody (ANA) and Human Leukocyte Antigen (HLA B-27) were negative. An attempt was made to induce sputum sample with the aid of saline nebulisation and resulting sputum sample was negative for Acid-Fast Bacillus (AFB) and Cartridge Based Nucleic Acid Amplification Test (CBNAAT) was also negative.
Ultrasound abdomen showing anechoic lesion with acoustic enhancement suggestive of lymphadenopathy in portocaval region.

CECT Abdomen showing lymphadenopathy with compression of portal vein
The patient was diagnosed as a case of abdominal TB on the basis of clinical and radiological criteria as per Revised National Tuberculosis Control Programme (RNTPC) guidelines with suspicion of Poncet’s disease. He was started on ATT (Isoniazid, Rifampicin, Ethambutol, and Pyrazinamide) with pyridoxine supplementation. The patient was discharged after 27 days and after taking ATT for 17 days. On follow-up after one month, there was improvement of abdominal and joint related symptoms. He was able to walk on his own with no complaints of pain, tenderness or swelling. Joints were normal on examination with full range of movement. Appetite and strength were slowly regained over the next few months. There was no recurrence of joint related complaints on the last follow-up at the completion of six months of ATT.
Discussion
Poncet's Disease (PD) is a sterile, non-erosive, reactive symmetrical inflammation of large joints of lower limbs seen in association with EPTB. Four different categories of joint-related manifestations have been recognised in association with TB: Direct musculoskeletal involvement of Mycobacterium Tuberculosis (M.TB) (TB septic arthritis aka tubercular arthritis), Mycobacterium Tuberculosis (M.TB) infection in patients of rheumatologic diseases who are on anti-TNF alpha DMARDS, ATT induced rheumatologic syndromes (tendinitis, lupus); reactive immunologic phenomena caused by TB (reactive arthritis, Erythema Nodosum) [1]. Poncet’s disease is a rare form of acute reactive, aseptic polyarthritis associated with active EPTB. It commonly starts insidiously, affecting multiple large weight bearing joints symmetrically causing crippling pain and limitation of range of movements. The joint inflammation is sterile and is associated with a distant focus of tubercular infection, usually enteric, urogenital or upper respiratory tract, and predominantly affects young adults. It responds well to ATT and is not associated with residual joint damage [2,3]. Poncet’s disease was first described in 1887 by Antoine Poncet as a polyarthritis that accompanies active TB at a distant focus which resolves with ATT without residual joint damage [4]. A significant number of cases have been reported in literature [5-9] describing a non-deforming polyarthritis of lower extremities seen in association with EPTB.
Diagnostic criteria of PD were described by Juan R et al., as: a) presence of extra-articular TB; b) involvement of more than one joint including knees and ankles); c) no axial, vertebral, sacroiliac involvement); d) nonspecific laboratory results); e) no chronic joint involvement; f) exclusion of other rheumatologic diseases [5].
Diagnosis of PD is often difficult as it develops insidiously and progresses slowly within a few weeks from TB infection [6], and clinically resembles other inflammatory arthritis. Moreover, it has been reported that serological tests such as Rheumatoid Factor (RF) and may be positive in patients with TB without documented clinical evidence of Rheumatoid Arthritis (RA). In patients with TB, positive Anti-CCP is reported in up to 37% and positive IgM RF in up to 62% even in absence of RA [10,11]. HLA B-27 is also known to be strongly associated with reactive arthritis and RA [12]. Poncet’s Disease is thus a diagnostic conundrum and patient may even receive long term unnecessary and potentially harmful DMARDS under suspicion of RA or Systemic lupus erythematosus (SLE) [13]. It has been suggested that T cell mediated cross reactivity between mycobacterial proteins and host cartilage in genetically inclined individuals contributes to the reactive arthritic process in Poncet’s Disease [14]. A similar pathogenesis has been suggested for erythema nodosum which has been reported in association with Poncet’s Disease producing suspicion of Lofgren’s Syndrome. This usually presents with bilateral ankle arthritis, Erythema Nodosum and mediastinal lymphadenopathy [7,15]. In the index patient there was no erythema nodosum. Tubercular infection of joint is usually a monoarthritis with evidence of acid fast bacilli in synovial fluid and leads to permanent joint damage if ATT is initiated late contrast Poncet’s Disease is a polyarthritis which resolves without complications rapidly with ATT. Poncet’s Disease is thus a diagnosis of exclusion and even in patients without quintessential symptoms of TB, clinicians, especially in countries of high disease burden, should be mindful of PD as one of the differential diagnoses. Fortunately, with initiation of ATT, it resolves without residual joint damage or long-term complications.
In the present patient, Poncet’s Disease was observed in association with abdominal TB. He had no evidence of pulmonary TB, X-ray chest being normal and sputum negative for AFB on microscopy and CBNAAT, although there was possibility of exposure to TB in the neighborhood. Thus, it is likely he had primary abdominal TB. Diagnostic workup for other rheumatological conditions was negative for RA factor, anti CCP, ANA Levels, HLA B-27 and complete resolution of all rheumatologic signs and symptoms was observed within a month from beginning ATT. In the two cases described by Kroots EJ one had mycobacteria grown in sputum culture while the other had histopathological findings suggestive of TB in axillary lymph node biopsy and normal X-ray chest [8]. Both patients had involvement of upper and lower limb joints and Erythema Nodosum lesions over the legs. Sharma A et al., described twenty-three cases of Poncet’s Disease in whom thirteen had oligoarthritis mostly involving ankle joint and EPTB most commonly tubercular lymphadenitis was reported [9]. In the case described abdominopelvic lymphadenopathy was associated with symmetrical ankle joint inflammatory involvement and there was no Erythema Nodosum. In this patient and all other reported case there was resolution of rheumatological manifestations with antitubercular therapy without any deformity.
Conclusion(s)
The authors describe Poncet’s Disease in a young patient suffering with abdominal TB. Active TB should be contemplated as a differential diagnosis in patients with fever and unusual presentation of joint pains, especially in endemic regions. It is important to determine the primary site of infection with adequate history, physical examination, and diagnostic imaging. This approach may prevent the initiation of immunosuppressive drugs in patients with an improper diagnosis of rheumatological disease, which would worsen the underlying TB infection. Even after ruling out rheumatoid diseases and other autoimmune diseases, the diagnosis of PD commands a high index of suspicion. Since not all clinicians are aware of PD, this condition often goes underdiagnosed.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 03, 2021
Manual Googling: May 11, 2021
iThenticate Software: May 29, 2021 (15%)
[1]. Franco-Paredes C, Díaz-Borjon A, Senger MA, Barragan L, Leonard M, The ever-expanding association between rheumatologic diseases and tuberculosisAm J Med 2006 119(6):470-77.10.1016/j.amjmed.2005.10.06316750957 [Google Scholar] [CrossRef] [PubMed]
[2]. Novaes GS, Kalil G, Borrelli FE, Criteria for diagnosis of Poncet’s diseaseRev Bras Rheumatol 1992 32:20-26. [Google Scholar]
[3]. Dall L, Long L, Stanford J, Poncet’s disease: Tuberculous rheumatismRev Infect Dis 1989 11(1):105-07.10.1093/clinids/11.1.1052644685 [Google Scholar] [CrossRef] [PubMed]
[4]. Poncet A, De la polyarthrite tuberculeuse deformante ou pseudorheumatisme chronique tuberculeuxCongres Fracaise de Chirague 1887 1:732-39. [Google Scholar]
[5]. Reuda JC, Crepy M, Mantilla RD, Clinical features of Poncet’s Disease: From the description of 198 cases found in literatureClin Rheumatol 2013 32(7):929-35.10.1007/s10067-013-2270-y23624588 [Google Scholar] [CrossRef] [PubMed]
[6]. Chakraborty PP, Ray S, Mandal SK, Poncet’s Disease: An unusual presentation of tuberculosis in a diabetic ladyWorld J Clin Cases 2015 3(4):385-88.10.12998/wjcc.v3.i4.38525879013 [Google Scholar] [CrossRef] [PubMed]
[7]. Gupta N, Bhatnagar AK, Musculoskeletal manifestations of tuberculosis: An observational studyJ Fam Med Prim Care 2018 7(3):538-41.10.4103/jfmpc.jfmpc_7_1730112304 [Google Scholar] [CrossRef] [PubMed]
[8]. Kroot EJ, Hazes JM, Colin EM, Dolhain RJ, Poncet’s disease: Reactive arthritis accompanying tuberculosis. Two case reports and a review of the literatureRheumatology (Oxford) 2007 46(3):484-89.10.1093/rheumatology/kel26816935915 [Google Scholar] [CrossRef] [PubMed]
[9]. Sharma A, Pinto B, Dogra S, Sharma K, Goyal P, Sagar V, A case series and review of Poncet’s disease, and the utility of current diagnostic criteriaInt J Rheum Dis 2016 19(10):1010-17.10.1111/1756-185X.1272626354099 [Google Scholar] [CrossRef] [PubMed]
[10]. Elkayam O, Segal R, Lidgi M, Caspi D, Positive Anti-cyclic citrullinated proteins and rheumatic factor during active tuberculosisAnn Rheum Dis 2006 65(8):1110-12.10.1136/ard.2005.04522916361276 [Google Scholar] [CrossRef] [PubMed]
[11]. Hirokazi S, Inagaki M, Shioda M, Nagasaka K, Poncet’s disease with high titres of rheumatoid factor and anti-citrullinated peptide antibodies mimicking rheumatoid arthritisJ Infect Chemother 2015 21(1):65-69.10.1016/j.jiac.2014.07.01525150438 [Google Scholar] [CrossRef] [PubMed]
[12]. Silva I, Mateus M, Branco JC, Poncet’s disease: A symmetric seronegative polyarthritis with enthesmopathy refractory to the therapyActa Rheumatol Port 2013 38(3):192-95. [Google Scholar]
[13]. Nyo MTL, Ally MMTM, Durren EMV, Ardense R, Poncet’s disease in the Preclinical phase of Rheumatoid ArthritisCase Reports in Rheumatol 2018 2018:357124710.1155/2018/357124729854537 [Google Scholar] [CrossRef] [PubMed]
[14]. Akturk H, Soydemir D, Abali S, Somer A, Yekeler E, Koksalan K, Poncet’s disease: Reactive arthritis due to tuberculosisJ Paediatr Inf 2016 10:72-75.10.5152/ced.2015.1789 [Google Scholar] [CrossRef]
[15]. Rizwi Z, Iqbal T, Javed A, Rizvi A, Erythema Nodosum: A consequence of tuberculosisCureus 2019 11(5):e274810.7759/cureus.4724 [Google Scholar] [CrossRef]