Central Serous Chorioretinopathy (CSCR) is the detachment of the neurosensory retina and/or Retinal Pigment Epithelium (RPE) due to accumulation of fluid in the subretinal space, mostly confined to the macula. Hereby, presenting a rare case of a 32-year-old patient with defective vision in both eyes, she was a known case of Chronic Kidney Disease (CKD) on haemodialysis. On examination best corrected visual acuity was 6/9 on dilated fundus examination with ring reflex in both eyes, Optical Coherence Tomography (OCT) macula showed detachment of the neurosensory retina from RPE with the subretinal fluid. This case is considered to be rare due to the unusual association noted between CSCR and End Stage Renal Disease (ESRD), in a female patient with no history of usage of corticosteroids or known identifiable risk factors. Hence, it is essential to screen patients with ESRD for CSCR to prevent vision threatening complications.
Case Report
A 32-year-old female patient came to the Out Patient Department (OPD) with complaints of defective vision in both eyes for two months. The patient was a known case of stage 5 CKD [1] secondary to focal segmental glomerulosclerosis, patient has been on haemodialysis since two months. Her developmental, prenatal, perinatal, postnatal, menstrual and family history were all uneventful. There was no history of steroid intake, systemic illness, any history of surgery. There was no history of metamorphopsia, delayed dark adaptation, floaters, flashes of light, photophobia. On examination, intelligence, speech, general physical examination and systemic examination were normal.
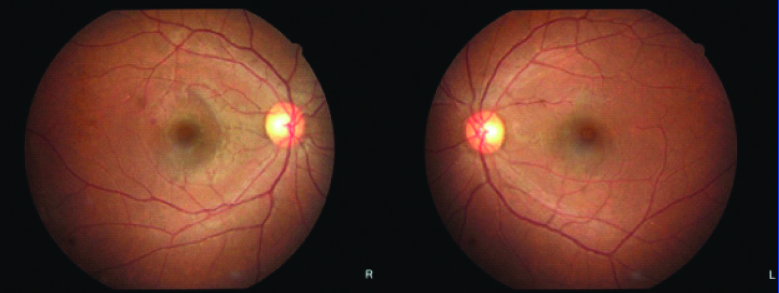
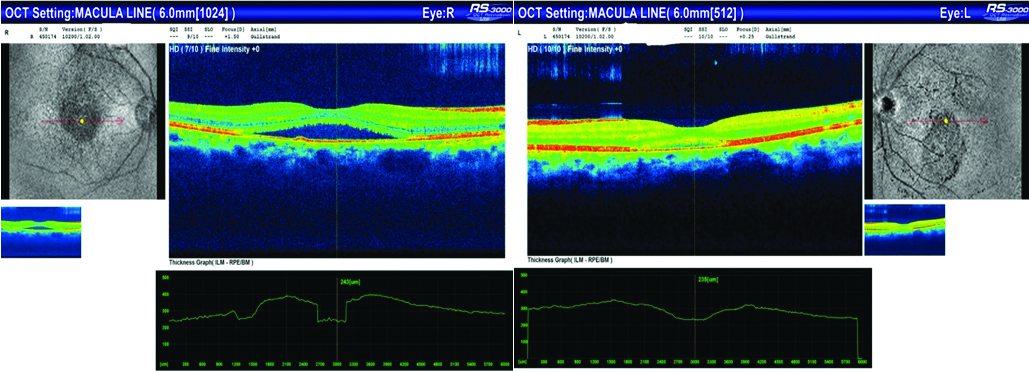
On ocular examination, best corrected visual acuity in both eyes was 6/9, anterior segment was normal, intraocular pressure was normal, distortion was seen on amslers test. On dilated fundus examination, disc and vessels were normal, macula showed ring reflex in both eyes [Table/Fig-1], a small haemorrhage temporal to macula was seen in the right eye [Table/Fig-1]. OCT macula showed detachment of the neurosensory retina from the RPE with subretinal fluid suggestive of CSCR [Table/Fig-2]. Patient has been managed conservatively with nepafenac eye drops, three times a day for one month and life style modifications. Patient was asked to review after one month, and was on monthly follow-up for three months.
Fundus photo showing a small haemorrhage temporal to macula along with ring reflex in right eye, ring reflex in left eye.
OCT macula showed detachment of neurosensory retina from the retinal pigment epithelium with subretinal fluid in both eyes.
Discussion
The CSCR is an idiopathic disorder characterised by a localised serous detachment of the sensory retina at the macula secondary to leakage from the choriocapillaris through one or more hyper permeable RPE sites [2]. It occurs more commonly in males 8:1 than females 10:1, usually between the age of 20-40 years [3,4]. Numerous risk factors are known, most common being history of usage of corticosteroids, other risk factors include type A personality, elevated endogenous cortisol, hypochondria, hysteria, conventional neurosis, pregnancy, sarcoidosis, collagen vascular disorder, obstructive sleep apnoea, alcohol consumption, allergic respiratory disease, hypertension, H pylori, family history and organ transplantation [2-5]. None of the above mentioned risk factors were found in present case.
Patients usually present with complaints of painless, gradual loss of vision, micropsia, metamorphopsia, decreased colour vision, scotoma [5]. Ocular findings of CKD patients include lid oedema, xanthalasma, conjunctivitis, conjunctival pallor, episcleritis, conjunctival and corneal calcification, pinguencula, subconjunctival haemorrhage, neovascular glaucoma, rubeosis iridis and the cataract were seen in the patient [5]. The patient presented only with complaints of defective vision with no history of metamorphopsia, micropsia, defective colour vision or scotomas which only on further evaluation was diagnosed as CSCR.
The CSCR is associated with activation of mineralocorticoid receptor due to corticosteroids and hormones, Progression of kidney damage to ESRD associated with vascular injury due to increase in blood pressure, renal fibrosis and proteinuria [6]. These further cause activation of mineralocorticoid receptor related to aldosterone. The genetic component has also been noted such as complement H may also play an important role in pathogenesis of CSCR [7-11]. Hyperpermeability of the choroid can be due to stasis, inflammation and ischemia, which may be due to steroids, catecholamines or sympathomimetic agents [2].
The hypercytokinemia in ESRD may be associated with uremia and dialysis. Due to the uremic toxin, volume overload and oxidative stress, there is increased generation and decreased elimination of proinflammatory cytokines, which leads to systemic inflammation and endothelial dysfunction [7]. Increased oxidative stress due to inflammation can lead to pathogenesis of CSCR, which is also a common mechanism between CSCR and ESRD [12]. It is essential to rule out other causes of subretinal fluid such as optic nerve pit, polypoidal choroidal vasculopathy, intraocular tumours, uveitis [13].
Investigations include OCT, Fundus Fluorescence Angiography (FFA) and Indocyanin Green Angiography (ICGA) [5]. On fluorescence angiography dot of hyper fluorescence showing a small focal leak from choroid into RPE is seen, showing an “ink blot” and “smoke stack pattern” [5,13]. OCT helps in measuring the subretinal fluid which also helps in follow-up, RPE appears as a red band due to its high reflectivity, sensory retina appears blue and both are separated by a clear space [13]. In ICGA, inner choroidal staining can be seen in mid phase and fades in late phase [5]. FAF patterns are seen as increased auto fluorescence at the site of leakage [5].
In patients with long standing subretinal fluid which cannot be efficiently re-absorbed due to extensive dysfunction and loss of RPE and choroidal disease. This chronic fluid leads to death of photoreceptors and permanent visual loss. It can also be complicated by (choroidal neovascularisation) CNV which can cause severe visual loss [2].
In acute cases, the visual prognosis is usually good and resolves in three to four months but can take upto one year, Recurrence is seen in 40-50% cases [4]. A case report by Chauhan A et al., “Ocular manifestation in a patient with CKD: A rare case report”, had a similar case scenario where the patient developed CSCR without the usage of corticosteroids [5]. A case report by Chatziralli I et al., “CSCR with multiple leakage points in a young female patient without detected risk factors” had no identifiable risk factors present [3]. Another case report by Farzan K et al., reported four cases, which developed CSCR after the usage of steroids [14].
A retrospective study conducted by Chang YS et al., “increased risk of CSCR following end stage renal disease” found that there was significantly elevated risk of CSCR in ESRD patients compared with normal individuals, but important confounding factors such as steroid use could not be taken into account [7].
Treatment options include argon laser photocoagulation, transpupillary thermotherapy, photo dynamic treatment with verteporfin, use of intravitreal bevacizumab, micropulse diode laser photocoagulation, use of corticosteroid antagonist and use of aspirin [5]. An association between CSCR and ESRD is a rare association and more over in our case since it has been noted in a female patient, which is uncommon and none of the known risk factors especially the usage of corticosteroids were not found.
Conclusion(s)
Though CSCR is a rare association in cases of renal failure, especially in a female patient even in the absence of corticosteroid use, it is essential to keep in mind for early detection and prevention of vision threatening complications.
[1]. Bauer C, Melamed ML, Hostetter TH, Staging of chronic kidney disease: time for a course correction: Table 1J Am Soc Nephrol [Internet] 2008 19(5):844-46.10.1681/ASN.200801011018385419 [Google Scholar] [CrossRef] [PubMed]
[2]. Nicholson B, Noble J, Forooghian F, Meyerle C, Central serous chorioretinopathy: Update on pathophysiology and treatmentSurv Ophthalmol [Internet] 2013 58(2):103-26.10.1016/j.survophthal.2012.07.00423410821 [Google Scholar] [CrossRef] [PubMed]
[3]. Chatziralli I, Kanonidoua E, Kanonidoua C, Chatzirallisa A, Papazisisa L, Central serous chorioretinopathy with multiple leakage points in a young female patient without detected risk factorsJ Med Cases 2012 3(3):201-03.10.4021/jmc580w [Google Scholar] [CrossRef]
[4]. Rezaei L, Ghanbari H, Dehghani A, Farzan K, Central serous chorioretinopathy following kidney transplantationSaudi J Kidney Dis Transplant [Internet] 2014 25(3):61510.4103/1319-2442.13220824821161 [Google Scholar] [CrossRef] [PubMed]
[5]. Chauhan A, Datt S, Ocular manifestation in a patient with chronic kidney disease: A rare case reportEur J Ther [Internet] 2017 22(4):222-24.10.5152/EurJTher.2016.08113 [Google Scholar] [CrossRef]
[6]. Bolignano D, Palmer SC, Navaneethan SD, Strippoli GF, Aldosterone antagonists for preventing the progression of chronic kidney diseaseCochrane Database Syst Rev 2014 (4):CD00700410.1002/14651858.CD007004.pub324782282 [Google Scholar] [CrossRef] [PubMed]
[7]. Chang Y-S, Weng S-F, Wang J-J, Jan R-L, Increased risk of central serous chorioretinopathy following end-stage renal diseaseMedicine (Baltimore) [Internet] 2019 98(11):e1485910.1097/MD.000000000001485930882685 [Google Scholar] [CrossRef] [PubMed]
[8]. Weenink AC, Borsje RA, Oosterhuis JA, Familial chronic central serous chorioretinopathyOphthalmologica 2001 215:183-87.10.1159/00005085511340388 [Google Scholar] [CrossRef] [PubMed]
[9]. Park DW, Schatz H, Gaffney MM, McDonald HR, Johnson RN, Schaeffer D, Central serous chorioretinopathy in two familiesEur J Ophthalmol 1998 8:42-47.10.1177/1120672198008001109590595 [Google Scholar] [CrossRef] [PubMed]
[10]. Miki A, Kondo N, Yanagisawa S, Bessho H, Honda S, Negi A, Common variants in the complement factor H gene confer genetic susceptibility to central serous chorioretinopathyOphthalmology 2014 121(5):1067-72.10.1016/j.ophtha.2013.11.02024365176 [Google Scholar] [CrossRef] [PubMed]
[11]. De Jong EK, Breukink MB, Schellevis RL, Bakker B, Mohr JK, Fauser S, Chronic central serous chorioretinopathy is associated with genetic variants implicated in age-related macular degenerationOphthalmology 2015 122(3):562-70.10.1016/j.ophtha.2014.09.02625439433 [Google Scholar] [CrossRef] [PubMed]
[12]. Yannuzzi LA, Central serous chorioretinopathy: A personal perspectiveAm J Opthalmol 2010 149:361-63.10.1016/j.ajo.2009.11.01720172062 [Google Scholar] [CrossRef] [PubMed]
[13]. Vegunta S, Hwang ES, Hartnett HME, Central Serous Chorioretinopathy- A case reportMoran Core 2015 Available from: http://morancore.utah.edu/section-12-retina-and-vitreous/central-serous-chorioretinopathy-case-report/ [Google Scholar]
[14]. Farzan K, Rezaei L, Ghanbari H, Dehghani A, Central serous chorioretinopathy following kidney transplantationSaudi J Kidney Dis Transpl 2014 25:615-20.10.4103/1319-2442.13220824821161 [Google Scholar] [CrossRef] [PubMed]