Radicular Dens Invaginatus (RDI) represent a rare form of dens invaginatus which develops in the root of the tooth after the crown development is completed that can sometimes cause complex pathological conditions that are difficult to diagnose. This case report describes a case of a RDI associated with an inflammatory periapical cyst. A 17-year-old female complained of mobility in tooth 22. The tooth showed gyroversion and colour change and no evidence of caries or root fracture. Axial slices and tridimensional reconstruction of the cone-beam computed tomography revealed the presence of a RDI on the distal surface of the root that extended from cervical to the apical third. The diagnostic hypothesis was symptomatic infectious apical periodontitis, and conventional root canal treatment was performed. Subsequently, it was opted for a complementary surgical approach, which involved an aspiration puncture bulletin with a collection of yellow-citrus liquid, periapical curettage, apicectomy, retro-preparation and retrofilling with Mineral Trioxide Aggregate (MTA). Histopathological examination revealed inflammatory periapical cyst. After 3-years, repair of the area was evident. Surgical management of this rare condition can be favourable for resolving endodontic infection related to this dental anomoly.
Cone-beam computed tomography, Dens in dente, Palatogingival groove, Radicular cyst, Root canal treatment
Case Report
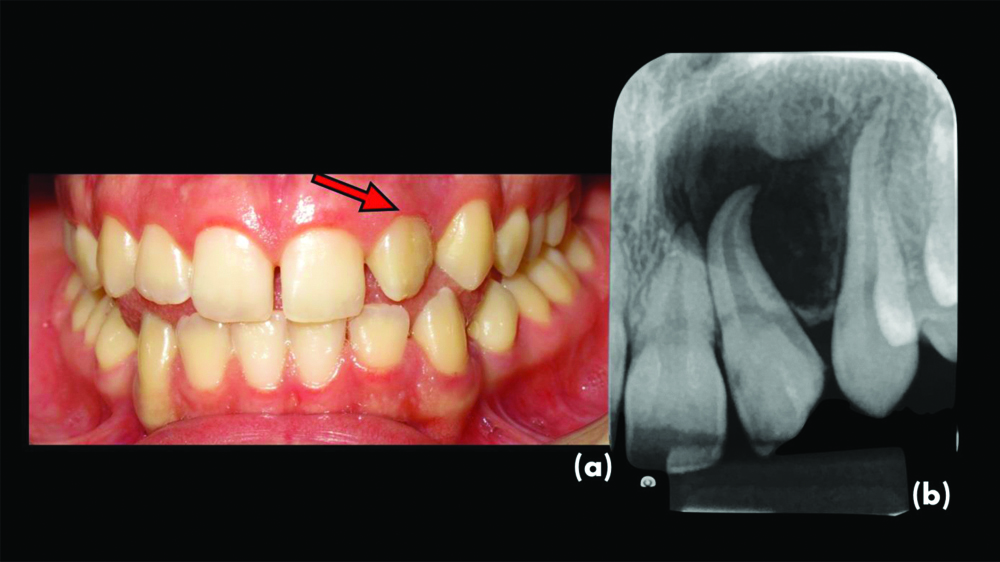
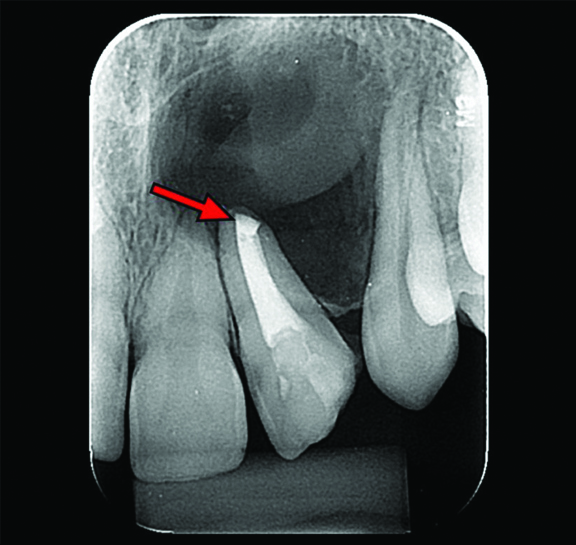
A 17-year-old female was referred to the Department of Endodontics for evaluation of a defined radiolucent lesion in the region of the upper incisors. The patient complained of slight mobility and moderate pain for the past two months that intensified during chewing in the tooth 22 but did not report any previous history of dental trauma. It was observed that tooth presented with gyroversion, and conoid shape with change at the inciso-distal angle, however, there was no evident edema or swelling in the region. The probing depth of the buccal gingival sulcus was within normal limits. A periapical radiograph revealed a well-defined radiolucent area associated with the root of tooth 22, involving root of tooth 21 and 23 (extending to the bone crest) and promoting a root divergence from adjacent teeth [Table/Fig-1a,b]. Cold test was performed using a cold spray (Endo-Frost; Roeko, Langeman, Germany). The result of the test was negative.
a) Initial clinical aspect of tooth #22 showing gyroversion, colour change, and shape change at the inciso-distal angle; b) Periapical radiography shows a wide radiolucency at #22 and extending to teeth #21 and #23.
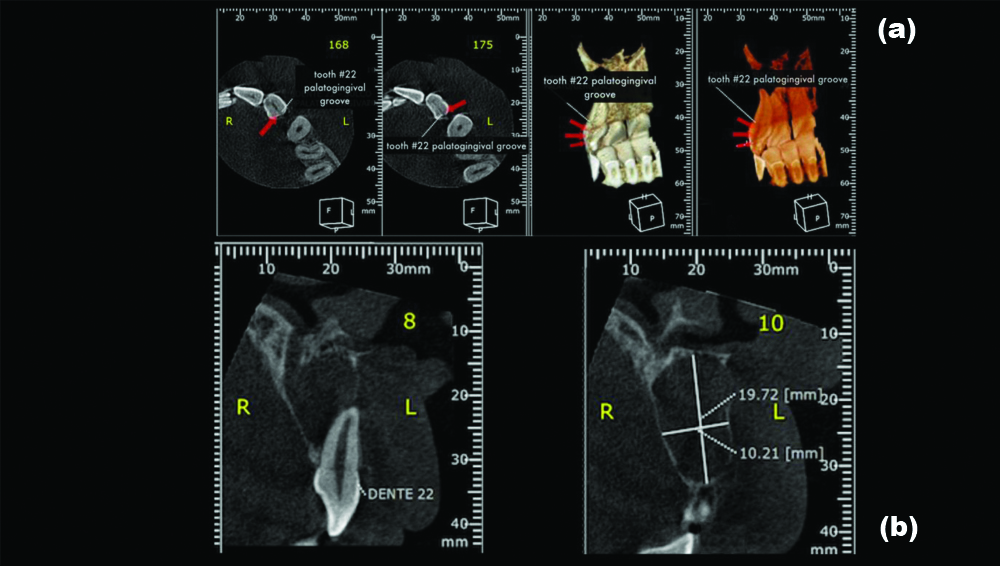
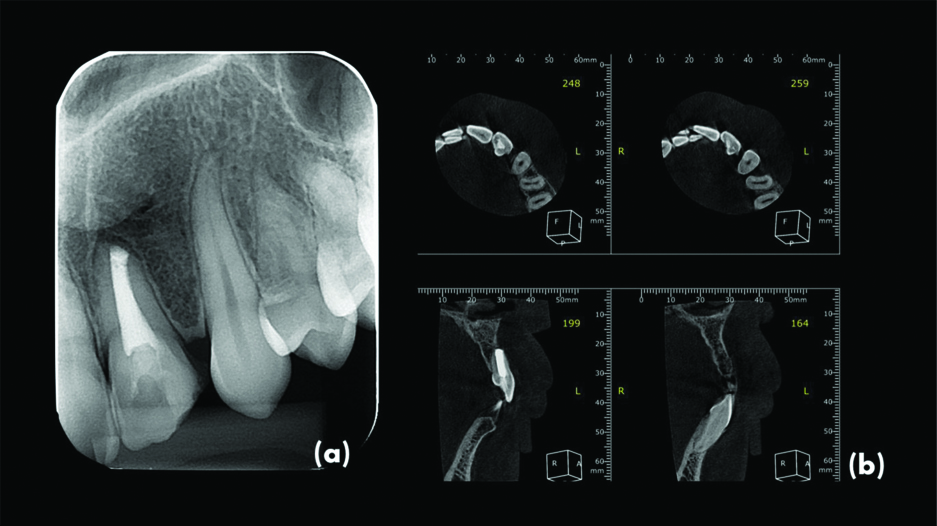
Cone-Beam Computed Tomography images showed a RDI on the distal surface of the root that extended from cervical to apical third. Transverse sections showed a wide area of periapical bone rarefaction with disruption of the vestibular cortex [Table/Fig-2a,b]. The provisional diagnosis of RDI with pulp necrosis and symptomatic apical periodontitis was established, and root canal treatment was planned.
a) CBCT preoperative images. Axial sections and 3D reconstruction showing a RDI on the distal surface of the root; b) Transverse sections showed a wide area of periapical bone rarefaction with disruption of the vestibular cortex.
The tooth was accessed using round diamond burs (#1011 and #1012) and isolated with a rubber dam, and the root canal was explored and pulp was extirpated using #10 and #15K-files (Dentsply Maillefer). Cervical preparation of the root canal was performed with Gates-Glidden® #1 and 2 and Largo® #1 drills. The working length was established based on the radiograph and K-file instrument. The apical third was prepared until the #80 K-file. During root canal preparation, the canal was irrigated with 2.5% sodium hypochlorite (NaOCl, Fitofarma, Brazil). After instrumentation, the canal was dried with an absorbent paper cone (Dentsply Maillefer) and then irrigated with 5 mL of 17% EDTA solution (Biodinâmica, Brazil) that remained in the root canal for 3 minutes to remove the smear layer. Calcium hydroxide (Biodinâmica, Brazil) was inserted and remained for 14 days. The access cavity was closed was restored with glass ionomer cement (Riva, SDI Brazil). Two other exchanges of intracanal medication were performed, interspersed for the same period, and after the improvement in clinical signs and symptoms was verified, and the root canal was filled with gutta-percha and Seal apex sealer (Sybron Endo, USA) using the lateral compaction technique. The cavity was permanently restored with composite resin (Z350, 3M ESPE, USA). Due to the extensive bone destruction seen in tomography images and the presence of a RDI as a potential niche for retaining bacterial biofilm, it was opted for the surgical approach as additional therapy.
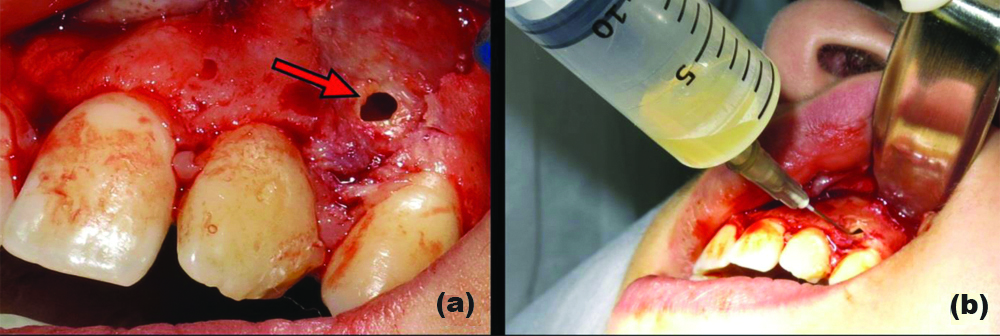
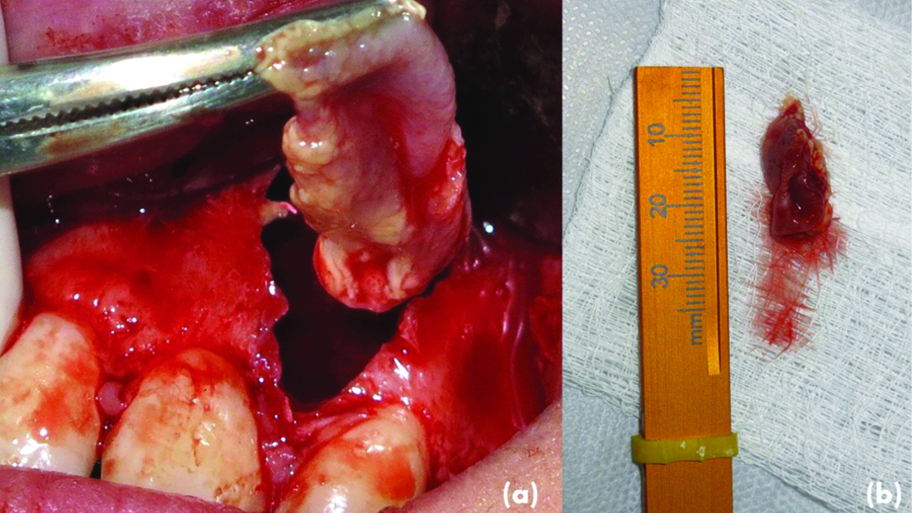
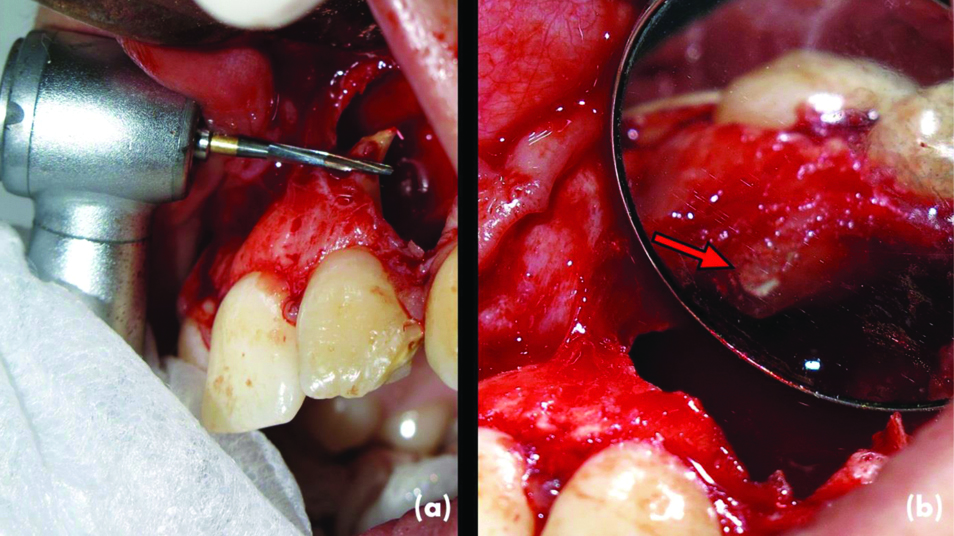
The surgical procedure started with a modified Neumann incision and periosteal mucus flap, detached and folded, which enabled the visualisation of an already fenestrated area in the apical region of tooth 22, with a rupture of the vestibular bone cortex. An aspiration puncture was performed in the fenestrated site in which yellow-citrus liquid, characteristic of cystic lesions, was observed [Table/Fig-3a,b]. Spherical carbide drills #2 and 3 were used for osteotomy. Periapical curettage was performed with the removal of soft tissue, of fusiform and cystic shape, which was placed in a frame with 10% formaldehyde solution [Table/Fig-4a,b]. Apicectomy was performed with a 28 mm Zecrya® drill, 3 mm from the root apex. The retrocavity was made with the aid of a PM1 ultrasonic tip (Helse Ultrasonic, Brazil) coupled with the EMS PM 200 ultrasonic unit (EMS, Switzerland) and adjusted to 30% power, and filled with white MTA (Angelus, Brazil) [Table/Fig-5a,b].
a) The area already fenestrated in the apical region of tooth #22, with disruption of the vestibular bone cortex; b) Aspiration puncture at the fenestrated site, from which a liquid yellow-citrus content was observed.
(a) Periapical curettage performed (b) Lesion removed with dimensions 25×10×5 mm.
a) Apicectomy was performed with the Zecrya® drill. b) Back cavity filled with white MTA.
The histopathological analysis revealed the presence of stratified parakeratinised squamous epithelium, covering a cystic cavity, and, just below this epithelium, the presence of fibrous connective tissue, with moderate mononuclear inflammatory infiltrate, hyperemic blood vessels and full of red blood cells in its interior, confirming the diagnosis of inflammatory periapical cyst. A week later, no clinical and radiographic complications were observed [Table/Fig-6]. The images revealed new bone formation and repair of apical periodontitis after three years [Table/Fig-7].
Radiographic evaluation 14 days after surgery; biomaterial (MTA) presence in the surgical store (arrow).
Radiographic (a) and tomographic (b) follow-up after three years demonstrated bone formation and repair of apical periodontitis
Discussion
The RDI represented a rare form of dens invaginatus which develops in the root of the tooth after the crown development is completed that can sometimes cause complex pathological conditions that are difficult to diagnose. This anomaly is considered rare, its prevalence varying from approximately 2.8% to 8.5%, being more commonly found in the maxillary incisors, predominantly the lateral incisors (93.8%) [1,2].
Several pathologies can be associated with RDI, including endodontic or periodontal disease, or both combined, with or without symptoms [1-3]. The initial periodontal evaluation showed that the probing depth of the gingival sulcus was within usual standards, which corroborates the thesis that the large area of bone destruction with disruption of the vestibular cortex detected by the CBCT images could be of endodontic origin, a fact that signaled the need for immediate endodontic intervention [Table/Fig-2a,b]. The objective was to promote the sanitisation of root canal systems.
The diagnosis of RDI is quite complicated and challenging because, in many cases, they can be confused with vertical root fractures [4,5]. Thus, the association of RDI and the possible endo-periodontal injury caused by this developmental anomaly may not be conclusive due to the absence of signs and symptoms. The CBCT becomes essential to determine the groove’s location and the size of the bone lesion involved [5,6]. The CBCT images in the case provided more accurate information regarding the extent of the lesion and the degree of bone destruction and enabled the definition of strategies for the surgical treatment of the lesion in tooth 22 affected by RDI.
A root groove should be considered only an area of periodontal risk that does not necessarily lead to periodontal disease onset [2]. Simon JHS et al., reported three cases of teeth affected by primary endodontic lesions associated with RDI. They suggested that the lesion formed might be due to bacteria that extended beyond the canal roots to the groove’s invaginated areas, which favours colonisation and growth and hinders the host’s defense mechanisms in these areas [4]. The complementary surgical approach was necessary because the finding of RDI in tooth 22 could be a factor of persistence of the periapical lesion due to the possible remaining microbial focus that could contribute to a self-sustaining infection.
The complex pathological conditions that could involve RDI as detected in several treatment modalities have been proposed [6-9], among which is the curettage of granulation tissue close to the invaginated areas of the groove, which was initially proposed for the surgical treatment of the case. The apical region’s initial exposure was necessary, which allowed access to the apical portion of the root and the defect assessment. After performing an aspiration puncture at the fenestrated site, where a yellow-citrus liquid content was observed, a cystic lesion associated with RDI was suspected, and the histopathological finding later confirmed it. The authors opted for the apicectomy of the 3 mm apical root because, this resection can promote the removal of approximately 98% of the apical ramifications and 95% of the lateral channels [9]. The presence of bacteria in these areas and the possible association with the groove found in this study could have caused the wide periapical lesion.
The invasion of microorganisms in the periapex region combined with inflammatory mediators involved in the pathogenesis of apical periodontitis can destroy periapical tissues with the consequent development of granulomas, abscesses, and periapical cysts [10,11]. A study that analysed 256 human periapical lesions, observed that approximately 52% of apical periodontitis cases had some odontogenic epithelium with proliferative capacity. However, only 15% were periapical cysts. It has been advocated that the cause of periapical cysts is a result of a chronic inflammatory process due to an apical periodontitis, from which the epithelial remnants of odontogenesis proliferate from stimuli of inflammatory cytokines and growth factors, forming a cavity lined by this epithelium [12]. Such a fact could justify the lesion’s development later diagnosed as an inflammatory periapical cyst in the histopathological examination [13]. The retrograde cavity preparation followed by retro-obturation was essential to promote airtight sealing of the root canal system.
Conclusion(s)
The survival and maintenance of the tooth in function should, whenever possible, be the ultimate goal of treatment. Despite the complexity and rarity of the clinical case involving a tooth affected by RDI associated with an inflammatory periapical cyst, which could have a very doubtful prognosis, the clinical and surgical management was favourable and feasible for resolving the endodontic infection associated with this dental anomaly.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 09, 2021
Manual Googling: Apr 29, 2021
iThenticate Software: May 24, 2021 (7%)
[1]. Cecilia MS, Lara VS, Moraes IG, The palato-gingival groove- A cause of failure in root canal treatmentOral Surg Oral Med Oral Pathol Oral Radiol 1998 85:94-98.10.1016/S1079-2104(98)90405-X [Google Scholar] [CrossRef]
[2]. Everett FG, Kramer GM, The disto-lingual groove in the maxillary lateral incisor; a periodontal hazardJ Periodontol 1972 43:352-61.10.1902/jop.1972.43.6.3524504186 [Google Scholar] [CrossRef] [PubMed]
[3]. Kim HJ, Choi Y, Yu MK, Lee KW, Min KS, Recognition and management of palatogingival groove for tooth survival: A literature reviewRestor Dent Endod 2017 42(2):77-86.10.5395/rde.2017.42.2.7728503472 [Google Scholar] [CrossRef] [PubMed]
[4]. Simon JHS, Dogan H, Ceresa LM, Silver GK, The radicular groove: Its potencial clinical significanceJ Endod 2000 26(5):295-98.10.1097/00004770-200005000-0001211199740 [Google Scholar] [CrossRef] [PubMed]
[5]. Giner-Lluesma T, Micó-Muñoz P, Prada I, Micó-Martínez P, Collado-Castellanos N, Manzano-Saiz A, Role of cone-beam computed tomography (CBCT) in diagnosis and treatment planning of two-rooted maxillary lateral incisor with palatogingival groove. Case reportJ Clin Exp Dent 2020 2(7):704-07.10.4317/jced.5709232905137 [Google Scholar] [CrossRef] [PubMed]
[6]. Garrido I, Abella F, Ordinola-Zapata R, Duran-Sindreu F, Roig M, Combined endodontic therapy and intentional replantation for the treatment of palatogingival grooveJ Endod 2016 42:324-28.10.1016/j.joen.2015.10.00926608020 [Google Scholar] [CrossRef] [PubMed]
[7]. Chung SH, Hwang YJ, You SY, Hwang YH, Oh S, A case report of multiple bilateral dens invaginatus in maxillary anteriorsRestor Dent Endod 2019 44(4):3910.5395/rde.2019.44.e3931799167 [Google Scholar] [CrossRef] [PubMed]
[8]. Forero-López J, Gamboa-Martinez L, Pico-Porras L, Niño-Barrera JL, Surgical management with intentional replantation on a tooth with palato-radicular grooveRestor Dent Endod 2015 40:166-71.10.5395/rde.2015.40.2.16625984480 [Google Scholar] [CrossRef] [PubMed]
[9]. Kim S, Kratchman S, Modern endodontic surgery concepts and practice: A reviewJ Endod 2006 32:601-23.10.1016/j.joen.2005.12.01016793466 [Google Scholar] [CrossRef] [PubMed]
[10]. Estrela C, Carmo Souza PO, Barbosa MG, Aburad de Carvalhosa A, Batista AC, Pinto Júnior DDS, Mesenchymal stem cell marker expression in periapical abscessJ Endod 2019 45(6):716-23.10.1016/j.joen.2019.03.00931060815 [Google Scholar] [CrossRef] [PubMed]
[11]. Lin LM, Huang GT, Rosenberg PA, Proliferation of epithelial cell rests, formation of apical cyst, and regression of apical wound healingJ Endod 2007 33:908-16.10.1016/j.joen.2007.02.00617878074 [Google Scholar] [CrossRef] [PubMed]
[12]. Ramachandran Nair PN, Pajarola G, Schroeder HE, Types and incidence of human periapical lesions obtained with extracted teethOral Surg Oral Med Oral Pathol Oral Radiol Endod 1996 81(1):93-102.10.1016/S1079-2104(96)80156-9 [Google Scholar] [CrossRef]
[13]. Zhu J, Wang X, Fang Y, Von den Hoff JW, Meng L, An update on the diagnosis and treatment of dens invaginatusAust Dent J 2017 62(3):261-75.10.1111/adj.1251328306163 [Google Scholar] [CrossRef] [PubMed]