Colonoscopy is one of the ways of evaluating the colon that is used to screen patients for colon cancer [1]. The adequacy of bowel preparation is a vital factor in successful screening [2]. It has been reported that bowel preparation is directly correlated with the correct diagnosis of colonoscopy, along with time, cost, and complications of colonoscopy [3]. For instance, the diagnosis of adenoma becomes less likely with poor bowel preparation [4]. According to studies in Europe and Australia, patients with poor bowel preparation had longer, more difficult procedures, and lower diagnostic yield for polyps during colonoscopy [5,6]. In addition, bowel preparation depends on age, weight, level of education, and patient adherence to the implementation of bowel preparation guidelines [7]. Many patients find bowel preparation to be the most difficult part of the examination, so it is important to minimise this problem [8].
To date, no standard regimen for colonoscopy preparation has been developed. According to the American College of Radiology, bowel preparation for colonoscopy should combine dietary restriction for a few days before colonoscopy, hydration, and laxatives such as sodium phosphate or low-volume Polyethylene Glycol (PEG) [9,10]. However, the use of laxatives such as PEG and sodium phosphate can cause diarrhea and impose a significant burden on the patient [11]. On the other hand, patient tolerability in bowel preparation for colonoscopy is one of the important factors in colonoscopy preparation [12]. Therefore, current guidelines for bowel preparation in colonoscopy screening are very challenging [13]. Accumulating evidence have indicated that low-fibre foods affect colon cleaning and patient readiness for colonoscopy [14,15]. Using a low-fibre diet can reduce the amount of excretion, making it less difficult for the patient [16]. Meanwhile, it has been found that there is a strong correlation between low-fibre diet and cleaning the colon [3,17]. Eating a low-fibre diet the day before colonoscopy can have a better result in colonoscopy screening and can reduce hunger before colonoscopy [9].
Since patient adherence to the implementation of colonoscopy preparation standards plays a key role in the diagnosis of colonoscopy, devising an appropriate standard for bowel preparation can increase patient adherence to standard bowel preparation. This study aimed to determine whether giving a low-fibre diet the day before colonoscopy could improve patient adherence to colonoscopy screening without affecting the quality of colon cleaning.
Materials and Methods
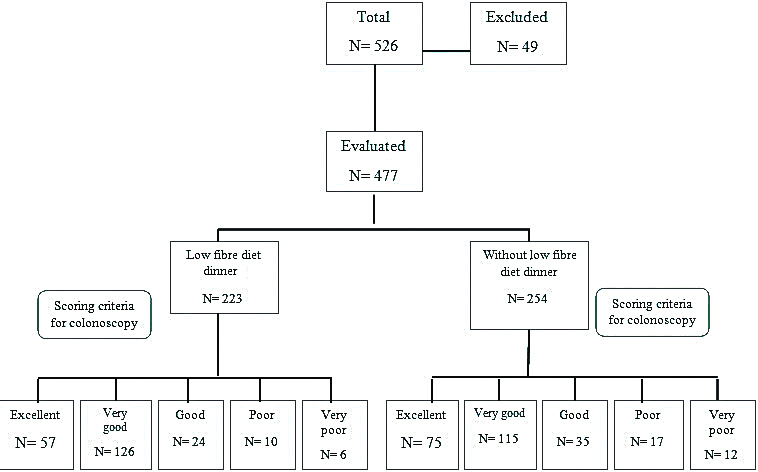
A randomised, single-blind, parallel group, non inferiority controlled trial was conducted to determine the effect of a low-fibre diet the day before colonoscopy for bowel preparation. The present study was approved by the Ethics Committee of the Health Research Board of Babol University of Medical Sciences and Clinical Trials of Iran with registration number IRCT2016011025292N2 and ethics code MUBABOL. REC.1392.1. In this study, a nurse randomly divided 526 patients from Rouhani Hospital from September 2014 to November 2015 and collected patients’ information through questionnaires [Table/Fig-1].
Inclusion criteria: All referred patients for colonoscopy except for emergency and hospitalised cases during the study period were included in the study.
Exclusion criteria: Colon resection, renal failure, heart failure, pregnancy, lactation, history of diabetes mellitus for more than two years, and a history of surgery or abdominal obstruction were excluded. Excluded from the study were 49 patients including four patients with colon resection, six patients with heart failure, 11 diabetic patients, one patient with renal failure, 26 patients due to abdominal obstruction and one pregnant patient.
All patients signed a consent form for colonoscopy. The first group received a low-fibre dinner such as white rice and yogurt a day before colonoscopy while the second group had no food for dinner (NPO). At 8 am of the colonoscopy day, colonoscopy was performed by an Olympus (series 180) machine under the supervision of a gastroenterologist and a colon specialist who were blinded to grouping.
Both groups were given a solution of 3 L of ethylene glycol and 60 mg of bisacodyl at three occasions: 3 pm and 7 pm the day before colonoscopy and 6 am on the colonoscopy day. Besides, Midazolam, propofol, and fentanyl were used as sedatives.
Scoring Criteria for Colonoscopy Preparation
Excellent (clean and free of any liquids), very good (clean with clear fluid, underlying mucus visible in clear fluid), good (clean with dirty liquid), poor (with particles including stools, but can be assessed at 80% mucus), and very poor (containing stool particles, and mucosal evaluation below 80%, colonoscopy was cancelled in this group) [9].
In this study, bubble and foam formation were also evaluated as follows: 1. Without any foam and bubbles; 2. Containing bubble and foam without dimethicone; 3. Foam and bubble and need for dimethicone.
Data Collection
Recorded data included age, sex, weight, height, level of education, number of bowel habits, bowel preparation score, colonoscopy diagnosis, and sedation dose.
Statistical Analysis
Data such as age, height, weight, BMI and sedative dose were performed by t-test and scoring of bowel preparation, sex and level of education by Chi-square were performed by SPSS software (version 26.0).
Results
Of all 526 patients participating in the study, 477 were evaluated and their cognitive information are listed in [Table/Fig-2]. The mean±SD of patients’ age in the first group is 48±14 (CI:46-50) and in the second group 49±14 (CI:47-51) (p=0.054). In the first group, 91 were male and 132 were female, and in the second group, 105 were male and 149 were female (p=0.09). The level of education did not differ significantly between the two groups (p=0.627). In the first group, 52.9% of patients were urban and 47% rural, and in the second group, 53.14% were urban and 46.85% rural (p=0.368). Postcolonoscopy diagnoses including normal, IBS, Diverticula, Haemorrhoid, Fissure, Inflammatory Bowel Disease (IBD), and others are shown in [Table/Fig-3]. It is worth mentioning that patients may have more than one diagnosis. Other diagnoses include Melanosis coli, solitary rectal ulcer, rectal prolapse, intestinal polyps, and intestinal worms. As a result, 223 patients in the first group and 254 in the second group were evaluated. As far as the relationship between patient age and the quality of bowel preparation was concerned, we found that the quality of bowel preparation decreased with age (p=0.001). However, there was no significant relationship between BMI and quality of bowel preparation (p=0.55) [Table/Fig-4]. The mean±SD sedative dose of midazolam, propofol and fentanyl in the first group were 2±0, 13±10, 41±40 while the average dose in the second group were 2±0, 9±13, 40±41, respectively (p=0.9, 0.496, 0.533). There was no significant difference between the two groups in terms of sedative doses.
Demographic data between dinner and no dinner patient at Bowel preparation.
| Variables | Low-fibre diet dinner (n=223) | Without dinner (n=254) | p-value |
|---|
| Age (years) (means±SD) | 48±14 (CI:46-50) | 49±14 (CI:47-51) | 0.054 |
| Sex M/F | 91/132 | 105/149 | 0.09 |
| Body mass index (kg/m2) | 26±4.0 (CI:25-27) | 26±4.0 (CI:25-26) | 0.551 |
| Education | None n (%) | 70 (31.39) | 76 (29.92) | 0.627 |
| School n (%) | 36 (16.14) | 55 (21.65) |
| High school n (%) | 80 (35.87) | 86 (33.85) |
| University n (%) | 37 (16.59) | 37 (14.56) |
| Bowel habit | Diarrhea n (%) | 31 (13.9) | 28 (11.02) | 0.732 |
| Constipation n (%) | 33 (14.79) | 43 (16.9) |
| Normal n (%) | 159 (71.3) | 183 (72.02) |
| Living | Urban n (%) | 118 (52.9) | 135 (53.14) | 0.368 |
| Rural n (%) | 105 (47) | 119 (46.85) |
Data are expressed as means±SD or total number (percentage). p-values characterise differences between groups “Low-fibre diet dinner” and “without dinner”
Chi-square test for education, bowel habit, living and sex independent sample t-test for age
Patient diagnosis after colonoscopy at bowel preparation with or without diet.
| Variables | Normal n (%) | IBS n (%) | Diverticula n (%) | Hemorrhoid n (%) | Fissure n (%) | IBD n (%) | Cancer n (%) | Other n (%) |
|---|
| With dinner (n=223) | 45 (16.9) | 112 (42.2) | 28 (10.5) | 23 (8.6) | 31 (11.6) | 10 (3.77) | 3 (1.1) | 13 (4.9) |
| Without dinner (n=254) | 60 (21.27) | 102 (36.1) | 23 (8.1) | 22 (7.8) | 34 (12) | 14 (4.9) | 4 (1.4) | 23 (8.1) |
Other: Melanosis coli, solitary rectal ulcer, rectal prolapse, intestinal polyps, and intestinal worms
*Patients may have more than one diagnosis
Quality of Bowel preparation in patient with and without diet according to age and Body Mass Index (BMI).
| Variables | Excellent | Very good | Good | Poor | Very poor (Cancel) | p-value |
|---|
| Low-fibre dinner (n=223) | Number n (%) | 57 (25.5) | 126 (56.5) | 24 (10.7) | 10 (4.4) | 6 (2.6) | |
| Age (years) (mean±SD) | 44±14 | 48±14 | 51±15 | 57±15 | 55±8 |
| BMI (kg/m2) (mean±SD) | 26±3 | 26±3 | 25±4 | 25±3 | 30±12 |
| Without dinner (n=254) | Number n (%) | 75 (29.6) | 115 (45.3) | 35 (13.8) | 17 (6.7) | 12 (4.7) |
| Age (years) (mean±SD) | 46±14 | 49±15 | 53±13 | 56±16 | 52±13 |
| BMI (kg/m2) (mean±SD) | 25±3 | 26±3 | 28±5 | 26±4 | 25±3 |
| Total | Number N (%) | 132 (27.7) | 241 (50.5) | 59 (12.3) | 27 (5.6) | 18 (3.6) |
| Age (years) (mean±SD) | 45±14 | 49±14 | 52±14 | 56±16 | 53±11 | 0.001 |
| BMI (kg/m2) (mean±SD) | 26±3 | 26±3 | 27±5 | 26±4 | 27±8 | 0.55 |
Data are expressed as means±SD or total number (percentage). Chi-square test
By examining the two groups in terms of foam and bubble formation, 73.9% of the patients who received a low-fibre diet the day before colonoscopy had a transparent colon without foam and bubbles, 23.8% of them had foam and bubbles in their colon and did not require dimethicone, and 2.2% of them had foam and bubbles in their colon and needed dimethicone. In the second group where patients were prepared for colonoscopy without dinner (fasting), 78.7% had a clear colon without foam and bubbles. In this group, 18.1% of the patients had foam and bubbles in their colon and did not require dimethicone while in 3.2% of them, foam and bubbles were observed in the colon and required dimethicone. (There was no significant difference between the two groups, p=0.224) [Table/Fig-5].
Comparison of two groups in terms of bubble and foam formation in colon.
| Variables | Without any foam n (%) | Foam without dimethicone n (%) | Foam and need dimethicone n (%) | Total N | p-value |
|---|
| With low-fibre dinner | 165 (73.9) | 53 (23.8) | 5 (2.2) | 223 | 0.224 |
| Without dinner | 200 (78.7) | 46 (18.1) | 8 (3.2) | 254 |
| Total | 365 | 99 | 13 | 477 |
p-values characterise difference between the formation of bubbles and foam in colon between the “with dinner” and “without dinner” groups. Chi-square test
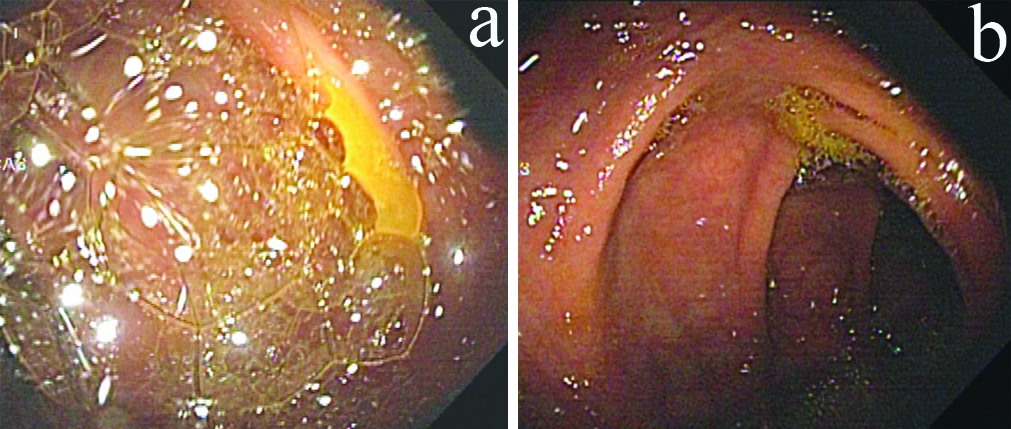
Patients were divided into normal, IBS, and other diagnoses according to colonoscopy diagnosis. In the first group, 11.1% of normal subjects, 71.4% of patients with IBS, and 15.74% of those with other diseases had foam and bubbles in their colon. In the second group, foam and bubbles were observed in 30% of normal patients, 48.1% of those with IBS, and 20.83% of patients with other diseases [Table/Fig-6]. The first group of IBS patients had a significant increase in foam and bubbles in the intestine 71.4% versus 48.1% (p=0.002) [Table/Fig-7]. As shown in [Table/Fig-8], the secretion of foam and bubbles increased in patients with IBS in the first group who had low-fibre foods to prepare the colon. The difference between the two groups in terms of the quality of colon preparation was not significant (p=0.169) [Table/Fig-9].
Comparison of foam and bubble formation in the colon of normal individuals, IBS and diagnosis of other diseases between the two groups.
| Variables | Diagnosis | Foam and bubble formation n (%) |
|---|
| With low-fibre dinner | Normal (n)=45 | 5 (11.1) |
| IBS (n)=112 | 80 (71.4) |
| Other diseases (n)=108 | 17 (15.74) |
| Without dinner | Normal (n)=60 | 18 (30) |
| IBS (n)=102 | 49 (48.1) |
| Other diseases (n)=120 | 25 (20.83) |
Other diseases: Melanosis coli, solitary rectal ulcer, rectal prolapse, intestinal polyps, and intestinal worms, Diverticula, Haemorrhoid, Fissure, IBD, Cancer
Comparison of patients with Irritable Bowel Syndrome (IBS) in two groups in terms of foam and bubble formation.
| Variables | Clear n (%) | Foam n (%) | Total n | p-value |
|---|
| With low-fibre dinner | 32 (28.6) | 80 (71.4) | 112 | 0.002 |
| Without dinner | 53 (51.9) | 49 (48.1) | 102 |
| Total | 85 | 129 | 214 |
p-values indicates the difference between patients with IBS in the two groups in terms of foam and bubble formation in the colon. Chi-square test
The presence of foam and bubbles in the colon of patients with IBS.
a: Existence of foam and bubbles in the colon of patients with IBS in the first group (With dinner)
b: Existence of foam and bubbles in the colon of patients with IBS in the second group (Without dinner)
Quality of colon preparation in patient with and without diet.
| Variables | Excellent n (%) | Very good n (%) | Good n (%) | Poor n (%) | Very poor (Cancel) n (%) | Total | p-value |
|---|
| With low-fibre dinner | 57 (25.5) | 126 (56.5) | 24 (10.7) | 10 (4.4) | 6 (2.6) | 223 | 0.169 |
| Without dinner | 75 (29.6) | 115 (45.3) | 35 (13.8) | 17 (6.7) | 12 (4.7) | 254 |
| Total | 132 | 241 | 59 | 27 | 18 | 477 |
Chi-square test
Discussion
An appropriate bowel preparation that can increase patient adherence to the procedure can be effective in screening and diagnosing colonoscopy. However, one of the important reasons that cause patients not to adhere to bowel preparations is the urge to avoid eating for a long time. Many methods have been devised to prepare the colon but these have not brought about a desirable outcome [18]. Diet is a significant factor and we frequently come across food materials such as grains and fruit seeds during colonoscopy in patients without any risk factors. At present, several guidelines (AGA, ESGE) recommend low-residue or full liquid diet on the day before colonoscopy [3,19].
Some centers for bowel preparation perform colonoscopy using PEG over a three-day or one-day period, which can reduce the duration of preparation by dividing PEG dosage to increase patient adherence to bowel preparation [20-22]. Several studies have evaluated the efficacy of diet liberalisation to Low-Residue Diet (LRD) on the bowel preparation compared to Clear Liquid Diet (CLD) [23-25]. Increasing data have proposed that having a low-fibre diet two days before colonoscopy improves the quality of bowel preparation [9,26]. Jung YS et al., showed similar rate of adequate bowel preparation between LRD and CLD (83.3% vs 83.5%) in healthy outpatients, recommending LRD avoiding fibre-rich foods as possible diet instructions prior to colonoscopy. Even though the consumption of unacceptable foods in LRD group was not evaluated in this study, compliance of diet instruction seems to be high considering high rate of adequate bowel preparation [27]. A 2009 study on 214 patients found that a LRD could be effective in bowel preparation for colonoscopy and increase patient adherence [28]. The use of low-fibre food in bowel preparation the night before colonoscopy reduces the number of patients who refuse to undergo colonoscopy due to the difficulty of bowel preparation. Our findings revealed that 82.1% of patients who consumed low-fibre diet for bowel preparation the night before colonoscopy had excellent and very good quality of bowel preparation compared with 74.8% of patients not receiving any diet. Moreover, examination of foam and bubbles in colon showed no significant difference between two groups. It was also found that the quality of bowel preparation decreased with age in both groups, suggesting an increase in the quality of bowel preparation by adding bisacodyl to PEG solution in the morning. In the present study, it was observed that people with IBS in the first group compared to those with IBS in the second group had more foam and bubbles in their colon (71.4% vs. 48.1%) (p=0.002), which can be due to the pathophysiology of IBS [29]. However, this needs further research. On the other hand, evaluating the level of education and urban/rural status of the patients showed that these were effective in implementing bowel preparation guidelines. It was previously found that a low-fibre diet tailored for diabetic patients improved colon cleaning [30]. However, in this study, diabetic patients were not identified so that they could be provided with a low-fibre diet consistent with their condition. This, of course, may create problems in the preparation of the colon. Overall, adding a low-fibre diet can increase patient adherence to bowel preparation without compromising its quality and prepare the patient for a colonoscopy without enduring hunger to our knowledge, this study was a largest clinical trial that examined a diet in bowel preparation. The study included an almost homogeneous population to use the diet to bowel preparation.
Limitation(s)
The study was not limitation-free. The selection criteria for this trial were not restrictive and the results may thus apply to any Fecal Immunochemical Test (FIT)-based screening program population. Furthermore, the present findings may not be generalisable to other clinical settings. We did not measure participant’s compliance with the proposed diet. Finally, we used a no validated questionnaire for symptoms, a common limitation in most studies on bowel preparation.
Conclusion(s)
Proper bowel preparation in colonoscopy is one of the ways to increase the patient’s commitment to colonoscopy, which leads to cost and time. The experiment showed that a low-fibre diet the day before colonoscopy increased the patient’s commitment to performing the bowel preparation process for colonoscopy. We conclude that a low-fibre diet the day before colonoscopy can be considered the most effective way to prepare the bowel for colonoscopy.
Data are expressed as means±SD or total number (percentage). p-values characterise differences between groups “Low-fibre diet dinner” and “without dinner”
Chi-square test for education, bowel habit, living and sex independent sample t-test for age
Other: Melanosis coli, solitary rectal ulcer, rectal prolapse, intestinal polyps, and intestinal worms
*Patients may have more than one diagnosis
Data are expressed as means±SD or total number (percentage). Chi-square test
p-values characterise difference between the formation of bubbles and foam in colon between the “with dinner” and “without dinner” groups. Chi-square test
Other diseases: Melanosis coli, solitary rectal ulcer, rectal prolapse, intestinal polyps, and intestinal worms, Diverticula, Haemorrhoid, Fissure, IBD, Cancer
p-values indicates the difference between patients with IBS in the two groups in terms of foam and bubble formation in the colon. Chi-square test
Chi-square test