Giant Malignant Phyllodes Tumour of Breast- A Clinical Dilemma and Surgical Challenge
Raghav Yelamanchi1, Nikhil Gupta2, Dhruv Gupta3, CK Durga4
1 Resident, Department of Surgery, Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
2 Professor, Department of Surgery, Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
3 Resident, Department of Surgery, Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
4 Professor, Department of Surgery, Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Raghav Yelamanchi, Sard 17, Old Building, Dr. Ram Manohar Lohia Hospital, New Delhi, India.
E-mail: raghavyelamanchi@gmail.com
Phyllodes tumour is an uncommon tumour of the breast. It is fibroepithelial in origin and mostly benign. Giant phyllodes tumours are described as tumours with size more than 10 cm and are extremely rare. Differentiating malignant and benign tumours pathologically is difficult and needs clinical judgement and high index of suspicion. A 50-year-old female presented with complaint of swelling in the left breast. On further evaluation, it was diagnosed as phyllodes tumour on biopsy. She underwent left mastectomy and excision of pectoralis major muscle due to clinical and radiological suspicion of malignancy. Postoperative histopathology report revealed malignant phyllodes tumour. Cases of giant phyllodes tumour should undergo adequate imaging and image guided biopsy with high index for suspicion for malignancy. They should be operated as per the principles of oncosurgery as there is a high probability of such huge tumours harboring malignancy.
Cystosarcoma phyllodes, Fibroepithelial tumour, Lattismus dorsi flap, Reconstruction
Case Report
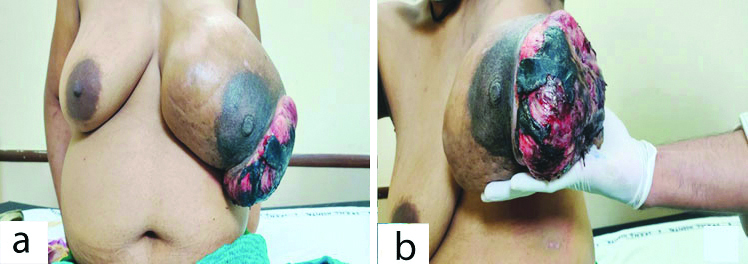
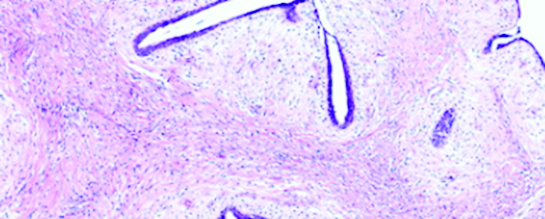
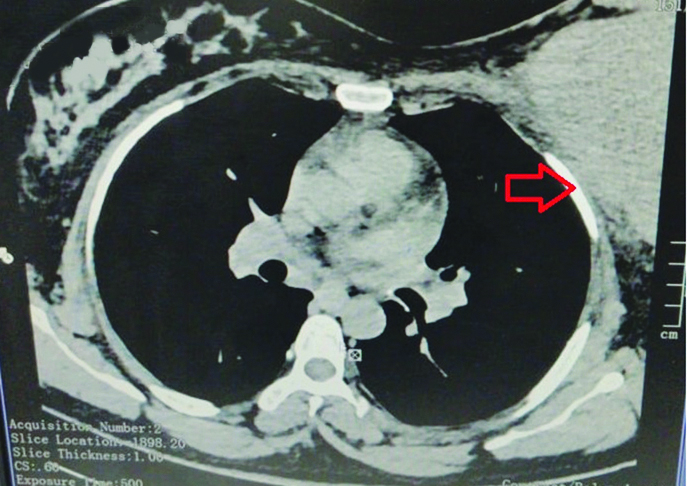
A 50-year-old female presented to the Surgery Department with complaints of swelling in the left breast for the last two years. The swelling was initially small but there was a rapid increase in the size of the swelling along with development of ulceration of overlying skin since last six months. There was no significant past history. On examination, there was a huge swelling of size 25×15×15 cm occupying the entire left breast with an ulcerofungating growth of size 13×10 cm over the skin [Table/Fig-1a and b]. On palpation, consistency of the swelling was variegated and the swelling was fixed to the underlying muscle. A single anterior axillary lymph node was palpable of size 2×1 cm. Mammography of the left breast was suggestive of Breast Imaging, Reporting and Data System (BIRADS) category 3. Biopsy from the lesion showed leaf like epithelial pattern with stromal hypercellularity conclusive of benign phyllodes tumour [Table/Fig-2]. No immunohistochemistry markers were tested. Fine Needle Aspiration Cytology (FNAC) of axillary lymph node suggested inflammatory lymphoid hyperplasia. Computerised tomography of chest showed the tumour invading the pectoralis major [Table/Fig-3].
Pre-operative images of the breast swelling with ulcerofungating growth.
Histopathological image of the biopsy specimen of the tumour 100X (H&E staining) showing leaf like epithelial pattern.
Computerised tomography of the chest. Arrow showing the invasion of the pectoral muscles by the tumour.
There was a clinical dilemma because of discordant results between clinical and pathological diagnosis. Even though the biopsy report suggested benign phyllodes tumour authors had a strong suspicion of malignancy due to clinical features such as rapid growth of the tumour as well as fixity to the underlying pectoralis muscle. The differential diagnoses of malignant phyllodes tumour or co-existing invasive carcinoma along with phyllodes tumour was made.
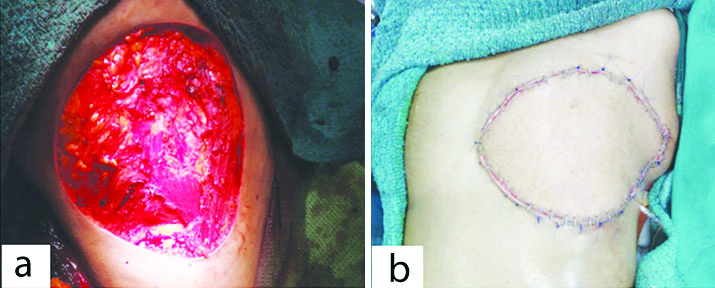
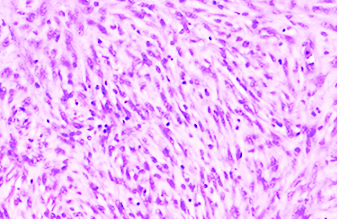
The patient was operated as per oncological principles as there was a suspicion for malignancy. Patient underwent left mastectomy along with removal of underlying pectoralis major muscle. The soft tissue defect was large and was closed by harvesting lattismus dorsi myocutaneous flap from the trunk [Table/Fig-4]. The harvest site was closed primarily. The patient had an uneventful postoperative recovery. Postoperative histopathology report showed hypercellular stromal tissue with nuclear atypia pointing towards malignant phyllodes with pectoralis major invasion [Table/Fig-5]. All the margins were negative for tumour. The patient is presently undergoing radiotherapy and regular clinical examination of bilateral breasts during follow-up visits.
Soft tissue defect which was closed with lattismus dorsi myocutaneous flap.
Histopathological image 200x (H&E staining) showing the hypercellularity and nuclear atypia.
Discussion
Phyllodes tumours accounts for <1% of breast tumours and consists of epithelial and stromal components [1]. These tumours are described as cystosarcoma phyllodes by Johannes Muller in 1838 [2]. They are classified into benign, borderline or malignant as per the World Health Organisation (WHO) criteria 2013 which is based on stromal hypercellularity, mitotic figures, cytologic atypia, stromal overgrowth, and the nature of the tumour border [3]. However, the distinction between benign and malignant phyllodes tumour is difficult and does not always coincide with the clinical behavior [4]. Most of the tumours have a median size of 4 cm at presentation. Tumours of size more than 10 cm are referred as giant phyllodes tumour [5].
Surgery is the mainstay of treatment for phyllodes tumour. A wide local excision with 1 cm margin is usually recommended. The overall survival even for malignant tumours at five years is 82% [6]. Phyllodes tumours are known for local recurrence as high as 15%. Recurrences tend to have more aggressive growth and cellular atypia. This rare case of giant malignant phyllodes tumour which was a diagnostic challenge due to discordant clinical and biopsy findings and which had also tested our expertise to reconstruct the large defect left over after mastectomy.
Although most of the phyllodes tumours can be diagnosed by biopsy, there are limitations in accurately differentiating benign from malignant tumours [1]. The entire tumour may not harbor the malignancy. This is especially true in tumours with variegated consistency. There are also many case reports of malignant transformations in a benign phyllodes tumour [7]. Malignant transformation of a previously benign tumour progresses initially from a state of increased stromal cellularity to atypia to malignancy. On molecular analysis, malignant phyllodes tumours have decreased expression of Bcl-2, oestrogen receptor and beta-catenein. They have increased expression of p53, CD34, epidermal growth factor receptor, c-kit and high Ki-67 index [8]. There are also many reported cases of co-existing invasive carcinoma along with phyllodes tumour [9]. Large tumours of breast with ulcerofungating growth are rare and should be differentiated from other conditions of breast presenting with swelling and ulceration [Table/Fig-6].
Differential diagnosis of breast swelling with overlying skin ulceration.
| S. No. | Differential diagnosis | Characteristics |
|---|
| 1. | T4 breast carcinoma | Usually tumours are hard in consistency and accompanied by lymph node and systemic metastasis |
| 2. | Phyllodes tumour | Ulceration occurs due to rapid growth of tumour rather than true skin involvement |
| 3. | Soft tissue sarcoma | History of radiation exposure would be suggestive. Lymph node metastasis is very rare. Systemic metastasis is more common |
| 4. | Tubercular and fungal mastitis | Presents as swelling with ulceration and multiple discharging fistulae. Clinical and radiological similarities with T4 carcinoma |
| 5. | Granulomatous lesions of breast | Chronic granulomatous mastitis, Sarcoidosis, Wegeners granulomatosis, etc |
In various case series, the incidence of lympadenopathy in phyllodes tumours was 10-15%, although malignancy was detected in less than 1% of the nodes [10]. Hence, routine lymphadenectomy is not recommended unless they are pathologically proven lymph node deposits. The role of radiotherapy has been established in malignant phyllodes tumour with respect to local tumour control [11].
Conclusion(s)
All cases of giant phyllodes tumour should undergo adequate imaging and image guided biopsy with high index for suspicion for malignancy. Even if the biopsy is not suggestive of any malignancy they should be operated as per the principles of oncosurgery as there is a high probability of these tumours harboring malignant components in final histopathology. Also, if there are discordant finding on investigations, immunohistochemistry can be sought for better diagnosis as per literature which was not done for the above case.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 25, 2021
Manual Googling: Mar 06, 2021
iThenticate Software: May 04, 2021 (14%)
[1]. Mishra SP, Tiwary SK, Mishra M, Khanna AK, Phyllodes tumour of breast: A review articleISRN Surg 2013 2013:36146910.1155/2013/36146923577269 [Google Scholar] [CrossRef] [PubMed]
[2]. Fiks A, Cystosarcoma phyllodes of the mammary gland-Müller’s tumour. For the 180th birthday of Johannes MüllerVirchows Arch A Pathol Anat Histol 1981 392(1):01-06.10.1007/BF004305436269275 [Google Scholar] [CrossRef] [PubMed]
[3]. Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver WHO Classification of Tumours of the Breast. Chapter 11Fibroepithelial tumours 2012 4th edLyonIARC Press:143 [Google Scholar]
[4]. Sotheran W, Domjan J, Jeffrey M, Wise MH, Perry PM, Phyllodes tumours of the breast- A retrospective study from 1982-2000 of 50 cases in PortsmouthAnn R Coll Surg Engl 2005 87(5):339-44.10.1308/003588405X5112816176692 [Google Scholar] [CrossRef] [PubMed]
[5]. Liang MI, Ramaswamy B, Patterson CC, McKelvey MT, Gordillo G, Nuovo GJ, Giant breast tumours: Surgical management of phyllodes tumours, potential for reconstructive surgery and a review of literatureWorld J Surg Oncol 2008 6:11710.1186/1477-7819-6-11719014438 [Google Scholar] [CrossRef] [PubMed]
[6]. Chaney AW, Pollack A, McNeese MD, Zagars GK, Pisters PW, Pollock RE, Primary treatment of cystosarcoma phyllodes of the breastCancer 2000 89(7):1502-11.10.1002/1097-0142(20001001)89:7<1502::AID-CNCR13>3.0.CO;2-P [Google Scholar] [CrossRef]
[7]. Abdul Aziz M, Sullivan F, Kerin MJ, Callagy G, Malignant phyllodes tumour with liposarcomatous differentiation, invasive tubular carcinoma, and ductal and lobular carcinoma in situ: Case report and review of the literaturePatholog Res Int 2010 2010:50127410.4061/2010/50127421151726 [Google Scholar] [CrossRef] [PubMed]
[8]. Pornchai S, Chirappapha P, Pipatsakulroj W, Lertsithichai P, Vassanasiri W, Sitathanee C, Malignant transformation of phyllodes tumour: A case report and review of literatureClin Case Rep 2018 6(4):678-85.10.1002/ccr3.142829636939 [Google Scholar] [CrossRef] [PubMed]
[9]. Panko N, Jebran AA, Gomberawalla A, Connolly M, Invasive ductal carcinoma within a benign phyllodes tumourAm J Case Rep 2017 18:813-16.10.12659/AJCR.90377428724885 [Google Scholar] [CrossRef] [PubMed]
[10]. Islam S, Shah J, Harnarayan P, Naraynsingh V, The largest and neglected giant phyllodes tumour of the breast-A case report and literature reviewInt J Surg Case Rep 2016 26:96-100.10.1016/j.ijscr.2016.07.02227475116 [Google Scholar] [CrossRef] [PubMed]
[11]. Varghese SS, Sasidharan B, Manipadam MT, Paul MJ, Backianathan S, Radiotherapy in phyllodes tumourJ Clin Diagn Res 2017 11(1):XC01-03.10.7860/JCDR/2017/24591.916728274029 [Google Scholar] [CrossRef] [PubMed]