A Rare Case of Giant Dacryocystomucopyocele
Pooja R Jain1, Rohit P Tiwari2, Rakesh K Barot3, Arun Mane4, Vaidehi D Bhatt5
1 Lecturer, Department of Ophthalmology, Rajiv Gandhi Medical College and CSMH, Kalwa, Thane, Maharashtra, India.
2 Lecturer, Department of Ophthalmology, Rajiv Gandhi Medical College and CSMH, Kalwa, Thane, Maharashtra, India.
3 Professor, Department of Ophthalmology, Rajiv Gandhi Medical College and CSMH, Kalwa, Thane, Maharashtra, India.
4 Professor, Department of General Surgery, Rajiv Gandhi Medical College and CSMH, Kalwa, Thane, Maharashtra, India.
5 Junior Resident, Department of Ophthalmology, Rajiv Gandhi Medical College and CSMH, Kalwa, Thane, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rohit P Tiwari, 1703/04, Vertex Solitaire, A1, Bhiwandi-Murbad Road, Near Golden Park Apt, Kalyan (West)-421301, Maharashtra, India.
E-mail: drrohitptiwari@gmail.com
Chronic dacryocystitis is frequently caused by Nasolacrimal Duct (NLD) infection or obstruction. Mucocele is formed when chronic stagnation of tears occurs in the lacrimal sac. When mucocoele gets infected with pyogenic organisms, pyocele is formed. Proximal obstruction in mucopyocele causing encysted dacryocystomucopyocele presenting as an enormous swelling is very uncommon. Very few cases of giant encysted dacryocystomucopyocele are reported in literature. Hereby, authors report a case of 42-year-old male with an acquired, enormous dacryocystomucopyocele, which developed over only one and half years and produced upward displacement of the lower lid and mechanical obstruction for eye closure. Computed Tomography (CT) of orbit and paranasal sinuses was done to confirm the diagnosis and find out the extent of cyst. Complete surgical excision of the cyst was performed. There was no recurrence of the swelling at one year follow-up.
Chronic dacryocystitis, Lacrimal sac, Mucocele, Nasolacrimal duct, Pyocele
Case Report
A 42-year-old male, came to Out Patient Department (OPD) with complaint of progressive swelling in the right eye inner corner since one and half years. He gave history of multiple episodes of painless increase in size of the swelling followed by spontaneous rupture with drainage of pus and some reduction in size. However, it was soon followed by gradual increase to present size. Last such episode was two months before presentation. Incision and drainage of the swelling was done elsewhere, 15 months back. There was no history of watering, redness, purulent discharge from the right eye. He also complained of some restriction in right nasal field since last few days. The patient denied any history of repeated attacks of sinusitis, rhinitis or pharyngitis. Systemic history was insignificant.
On examination, an oval 5.0×4.8×4.0 cm swelling was noted in right lacrimal sac region which was firm, slightly indentable and non tender with a pus point [Table/Fig-1]. There was mild erythema and induration of overlying stretched skin. The swelling was overlying inner half of lower lid causing upward displacement of lower lid and mechanical obstruction for eye closure. The regurgitation test was negative. In both eyes unaided vision was 6/6. Rest ophthalmic examination and systemic examination was unremarkable. Anterior rhinoscopy was normal. Blood investigations including complete haemogram, blood sugar levels and seromarkers were normal.
Showing a large encysted mucopyocele with narrowing of the palpebral aperture of the right eye.

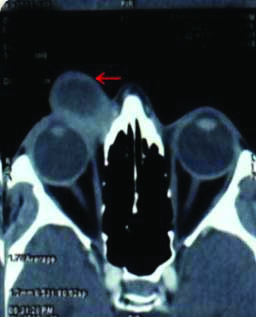
An orbital Computed Tomography (CT) scan showed a well-encapsulated, well-defined, preseptal cystic mass of size 3.4×3.3×3.0 cm in inferomedial aspect of right orbit inseparable from lacrimal sac with homogeneously enhancing wall having communication with Nasolacrimal Duct (NLD) [Table/Fig-2]. There was no radiologic evidence of invasion into adjacent sinuses, bone destruction or neoplasm. On correlation of the history, clinical features and radiological findings clinical diagnosis of a giant dacryocystomucopyocele was established.
Image of CT scan of orbit showing a well-defined, cystic lesion in inferomedial aspect of right orbit with homogenously enhancing wall (as shown by red arrow).
Patient underwent cyst excision under local anaesthesia with short sedation. Surgical steps included an elliptical 7 cm incision on right nasojugal fold followed by blunt dissection around the cyst to free it from orbicularis muscle. Midway during surgery the cyst ruptured followed by drainage of pus which was sent for microbiology assessment. The collapsed cyst was tagged with 4-0 vicryl suture and adequate traction was achieved for further dissection. The Bowman’s probe was introduced from lower punctum and cyst was confirmed to be continuous with common canaliculus. Cyst connections with surrounding soft tissue and NLD were severed. Excision of the mass was done en masse and sent for histopathology examination. Post excision, meticulous examination of the lacrimal fossa was done to rule out any remnants. Wound was closed in two layers after excising the stretched skin.
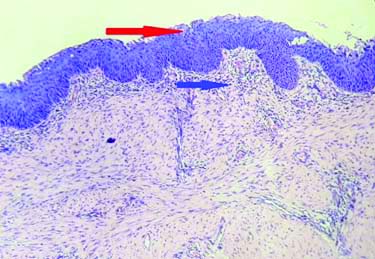
The collapsed cyst measured 2.9×2×1 cm [Table/Fig-3]. The fibrous wall was thickened and uninterrupted, measuring 1 mm in thickness. Histopathological examination revealed that the cystic cavity was lined by hyperplastic stratified squamous epithelium with focal denudation. The sub epithelium showed dense lymphoid cell infiltration with few neutrophils. There was no evidence of granuloma or malignancy [Table/Fig-4]. Gram staining of the aspirated fluid revealed occasional gram positive cocci and gram negative bacilli. Cultures demonstrated Klebsiella species. The postoperative period was uneventful. At one-year follow-up, patient was doing well without recurrence of swelling.
Specimen showing a collapsed and surgically delivered enlarged lacrimal sac (cyst).

Haematoxylin and Eosin stain with 20X magnification showing cyst wall lined by hyperplastic stratified squamous epithelium (shown by red arrow) with subepithelial lymphoid infiltration (shown by blue arrow).
Discussion
Dacryocystococeles or lacrimal mucoceles are non-neoplastic diffuse enlargements of the lacrimal sac by mucopurulent material and results from combined proximal and distal obstructions in the nasolacrimal pathway. They can be broadly categorised into congenital/infantile or acquired/adult [1]. Dacryocystoceles are cystic enlargements of the lacrimal sac filled with secretions derived from goblet cells and submucosal accessory seromucinous glands, mixed with entrapped tears [2]. In neonates, called amniotoceles, are represented by a painless swelling inferior to the medial canthal tendon generally without overlying cutaneous erythema [3].
In adults, due to NLD obstruction chronic stagnation of tears within the lacrimal sac occurs which leads to chronic dacryocystitis and formation of mucocele. When secondary blockage of canaliculi occurs, it becomes encysted. In the presence of abundant mucus in the cyst’s contents it is called as dacryocystomucocele. In protracted cases of chronic dacryocystitis when infection supervenes dacryocystomucopyocele term is more appropriate [1]. It is very uncommon to encounter large encysted dacryocystomucopyocele. Usual course of events in a case of chronic dacryocystitis are: epiphora, mucocele, recurrent acute on chronic dacryocystitis, lacrimal fistula. The present case is unusual as the patient developed a dacryocystomucopyocele of enormous size within a span of two years causing mechanical obstruction for eye closure and restriction in the nasal field of vision which is a rare presentation.
In present case, the primary acquired NLD obstruction was the cause of giant encysted dacryocystomucopyocele. NLD obstruction can be due to secondary causes like infections by low pathogenicity bacteria and fungi, dacryoliths, anatomical abnormalities such as anomalous ethmoid cells, fractures of face or complications of nasal surgeries and use of some drugs (docetaxel and fluorouracil). NLD obstruction is rarely caused by neoplasms of the NLD. In present case CT scan of orbit was of paramount importance in clinching the diagnosis, ruling out the extension into orbit and sinuses along with pre-operative planning of the surgery.
Review of literature revealed similar cases. Perry LJ et al., reported a case of a 95-year-old woman with a giant dacryocystomucopyocele of size 4×5 cm developed over 25 years and resulting in globe displacement with an associated conspicuous enlargement of the NLD [1]. Kamath SJ et al., reported another case of a 73-year-old man with encysted lacrimal mucopyocele of size 2.7×2.5×1.2 cm secondary to chronic dacryocystitis is reported. It was initially thought as malignancy as a large swelling caused distortion of surrounding structures [4]. An instance of orbital extension of encysted mucocele (3×3 cm) through a rent in the orbital septum has been reported by Krisnamurthy G et al., [5]. These cases mentioned were managed by complete cyst excision or Dacryocystectomy (DCT) as in present case. do Nascimento SB et al., reported a large lacrimal sac mucocele (1.2 cm in diameter) causing erosion of lamina papyracea and nasal septum along with compression of medial rectus and eyeball displacement was treated by surgical marsupialization [6]. Anwar MJ et al., reported a case of a 42-year-old male with idiopathic acquired encysted dacryocystocele of moderate size managed by external Dacryocystorhinostomy (DCR) with silicone tube intubation [7].
The surgical options of such swellings include external or endoscopic DCR with or without nasolacrimal stent placement or complete surgical excision of the cystic sac (DCT). Because of the infrequency of adult cases, there is no consensus as to the best surgical approach [1]. In present case complete surgical excision of the cystic sac was preferred as: (a) The cyst was very big and thick walled; (b) The histopathological examination of the cyst was important to rule out rare occurrence of malignancy; (c) DCR would have been technically more difficult with high chances of failure.
The literature search revealed that the present case is the largest dacryocystomucopyocele (5.0×4.8×4.0 cm) developed in short span of 15 months. Previously reported largest dacryocystomucopyocele (5×4 cm) developed over 25 years and was termed as ‘Giant dacryocystomucopyocele’ due to its enormous size [1].
Conclusion(s)
Appropriate clinical examination and CT orbit is of paramount importance for deciding diagnosis of dacryocystopyomucocele. Management strategy should be decided upon taking into consideration clinical presentation, extent of the cyst, need for histopathological analysis and technically feasible surgical option.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 17, 2021
Manual Googling: Feb 27, 2021
iThenticate Software: Mar 22, 2021 (15%)
[1]. Perry LJ, Jakobiec FA, Zakka FR, Rubin PA, Giant dacryocystomucopyocele in an adult: A review of lacrimal sac enlargements with clinical and histopathologic differential diagnosesSurv Ophthalmol 2012 57:474-85.10.1016/j.survophthal.2012.02.00322784678 [Google Scholar] [CrossRef] [PubMed]
[2]. Harris GJ, DiClementi D, Congenital dacryocystoceleArch Ophthalmol 1982 100:1763-65.10.1001/archopht.1982.010300407430067138344 [Google Scholar] [CrossRef] [PubMed]
[3]. Woo KI, Kim YD, Four cases of dacryocystoceleKorean J Ophthalmol 1997 11:65-69.10.3341/kjo.1997.11.1.659283156 [Google Scholar] [CrossRef] [PubMed]
[4]. Kamath SJ, Saha D, Krishna U, Kolavala B, A large encysted lacrimal sac mucocele- A typical presentationInternational Journal of Current Research 2017 9(10):59920-22. [Google Scholar]
[5]. Krisnamurthy G, Padmavar BU, Desai Y, An encysted lacrimal mucocele with orbital extensionIndian J Opthalmol 1977 25:40-41. [Google Scholar]
[6]. do Nascimento SB, Rodrigues AB, Jurity TP, de Sá JC, Castelo Branco AN, Lacrimal sac mucoceleBraz J Otorhinolaryngol 2014 80:540-41.10.1016/j.bjorl.2014.05.00125457075 [Google Scholar] [CrossRef] [PubMed]
[7]. Anwar MJ, Choudhry SA, Aadil M, Asif A, Ameer A, Idiopathic acquired dacryocystocele presenting only with epiphora: A very rare case reportCureus 2017 9(9):e165310.7759/cureus.1653 [Google Scholar] [CrossRef]