The Coronavirus Disease 2019 (COVID-19) pandemic began in December 2019 in Wuhan, China. Such sudden infectious outbreaks take a toll on the psychological health of our brave frontline healthcare physicians. Frontline healthcare physicians become vulnerable to psychological problems like depression, anxiety, stress, and insomnia. Long working hours, increased patient load, and risk of spread of contagion to family members are a few of the major contributing factors. Such factors, coupled with chronic stress and emotional exhaustion predispose doctors to experience burnout which has also been reported to increase the risk of mental morbidities. Early counselling, pandemic preparedness, self-care efforts, and stress management can help to cope in these adverse times. Various online portals have also been developed as an intervention strategy in mitigating the negative impact of this pandemic. The purpose of this viewpoint is to highlight the need to address such issues in physicians, find possible root causes, and suggest relevant measures to curb the incidence of these problems.
Anxiety, Burnout, Coronavirus disease 2019, Depression, Mental health, Stress
Introduction
The COVID-19 pandemic which started in December 2019 in Wuhan, China has been declared a pandemic by the World Health Organisation (WHO) on March 11, 2020. It has spread globally in over 219 countries infecting over 111 million people. With increasing numbers of confirmed cases and deaths every day, this pandemic poses a great challenge to the healthcare sectors of every country. As the number of patients is increasing every day, healthcare professionals are pushed to the limits everyday.
In this critical and fragile situation, the frontline Healthcare Workers (HCW) directly involved in the treatment and diagnosis of patients face tremendous amounts of pressure. Literature review of previous Severe Acute Respiratory Syndrome (SARS) outbreaks also suggests that an outbreak of sudden life-threatening illness put on tremendous amounts of pressure on physicians and nurses. [1,2]. Such pandemic situations require intense and immediate response in terms of healthcare, with thousands of HCW, delivering care to patients, and fighting at the frontline to address the challenges posed to healthcare systems. Lack of specific treatment, overwhelming workload, depletion of Personal Protective Equipment (PPE), inadequate support, and fear of catching and spreading the virus to family members places the physicians in zones vulnerable to various mental problems.
The HCW are thus facing critical situations that increase their risk of suffering for the psychological impact of dealing with several unfavourable conditions, with consequences that might span from psychological distress to mental health symptoms.
Literature Search
We searched for potentially eligible articles on PubMed and Google Scholar. We used the following set of terms to search the publications: “COVID-19”, “Physician”, “Stress”, “Mental Health”, “Depression”, “Anxiety”, and “Psychological Impact”. We narrowed down the search results and included relevant studies for our purpose.
Depression
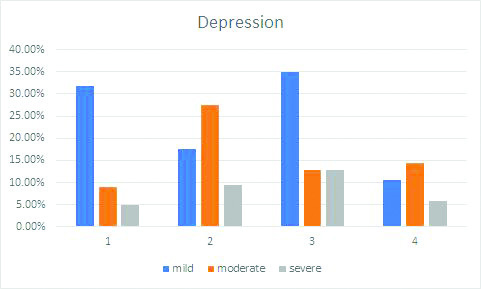
After a thorough reading of the existing literature, symptoms of depression were assessed and the prevalence of these symptoms was significant. The number of physicians exhibiting symptoms of mild depression as shown in [Table/Fig-1] ranged from 11% to 35%, moderate depression ranged from 8.9% to 27.4% and severe ranged from 4.9% to 13% [3-6]. One study also reported that 10.2% of physicians showed extremely severe depressive symptoms which were assessed using the Depression Anxiety Stress Scale-21 (DASS-21) tool. The studies used the Patient Health Questionnaire-9 (PHQ-9) and DASS-21 tools for the assessment. The PHQ-9 questionnaire scores each of the 9 Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) criteria as “0” (not at all) to “3” (nearly every day) with scores as (0-4) for normal, (5-9) for mild, (10-14) for moderate, and (15-21) for severe depression. DASS-21 is a self-report tool containing 21 items that assess three constructs: depression, anxiety, and stress. Each subscale includes 7 statements referring to the previous week. Ratings are made on a series of 4-point Likert-type scales from 0 (did not apply to me at all/never) to 3 (applied to me very much/always). Higher scores indicate more severe emotional distress [4].
Summary of the percentage of physicians working in the frontline, suffering from depression, obtained from the selected studies [3,4,5,6]. 1,2,3,4 on the x axis are representing reference studies [3,4,5,6] respectively.
Insomnia
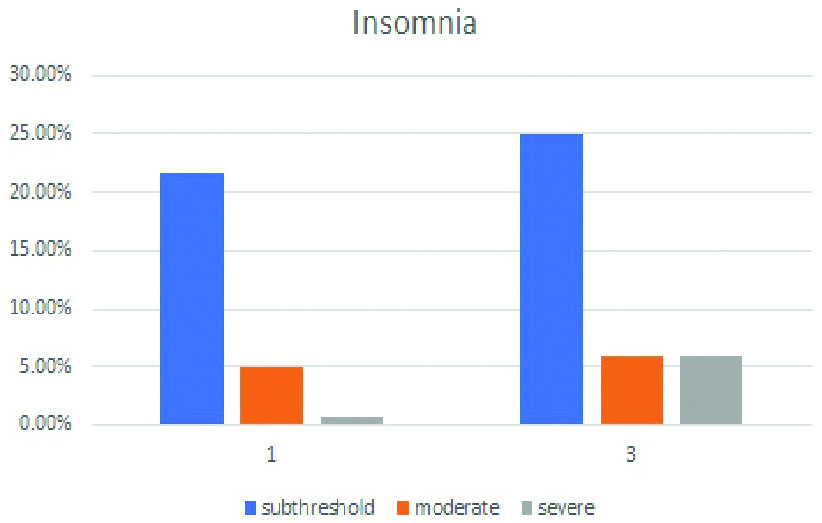
Many physicians also suffered from insomnia. [Table/Fig-2] shows that 21.7% to 25% experienced subthreshold insomnia whereas 4.9% to 5.93% of physicians experienced moderate insomnia [3,5]. A minor number, only 0.8%, of physicians were severely insomniac [3]. The Insomnia Severity Index (ISI) scale was used for assessment. The ISI comprises seven items assessing the perceived severity of difficulties initiating sleep, staying asleep, and early morning awakenings, satisfaction with current sleep pattern, interference with daily functioning, noticeability of impairment attributed to the sleep problem, and degree of distress or concern caused by the sleep problem. The ISI scores (0-7) indicated normal insomnia, (8-14) subthreshold, (15-21) moderate, and (22-28) severe insomnia [5].
Summary of the percentage of physicians, suffering from insomnia, obtained from the selected studies. 1,2,3,4 on the x-axis are representing refrence studies [3,5] respectively.
Stress and Anxiety
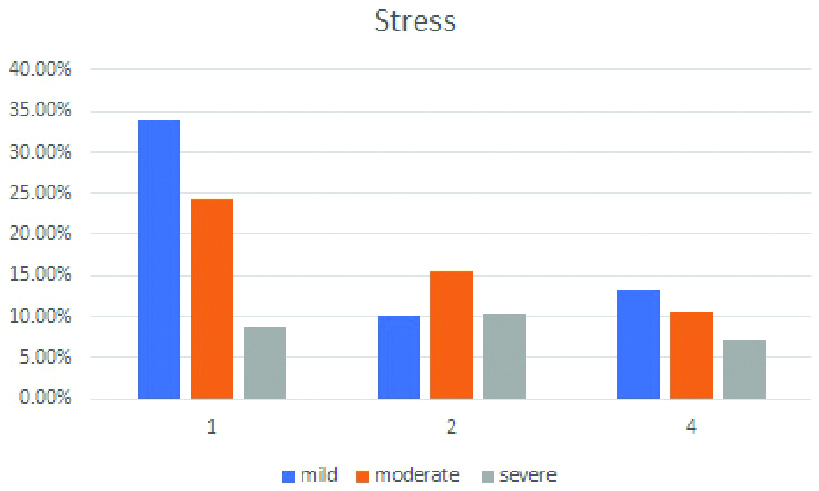
In studies using the DASS-21 scale, for stress subscale as is represented in [Table/Fig-3], 10.2% to 33.9% of the sample reported mild stress symptoms, 10.5% to 24.3% reported moderate, 7.2% to 10.4% reported severe and 5.0% reported extremely severe anxiety symptoms [3,4,6].
Summary of the percentage of physicians working in the frontline, suffering from stress, obtained from the selected studies. 1,2,3,4 on the x-axis are representing refrence studies [3,4,6] respectively.
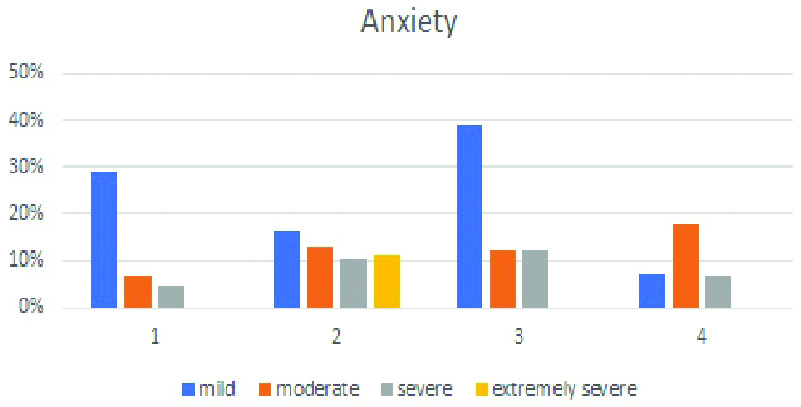
Previous studies assessing anxiety reported that 7% to 39.07% of the physicians were considered to have mild anxiety symptoms, 5% to 17% were considered to have moderate symptoms and on an average 11.5% were considered to have extremely severe anxiety symptoms. The prevalence of the aforementioned symptoms has been pictorially depicted in [Table/Fig-4] [3-6]. The studies were conducted using the Generalised Anxiety Disorder (GAD-7) questionnaire and the DASS-21 tool. [2,3,4]. GAD-7 is a seven-item instrument that is used to measure or assess the severity of GAD. Each item asks the individual to rate the severity of his or her symptoms over the past two weeks. The GAD-7 score is calculated by assigning scores of 0, 1, 2 and 3, to the response categories of “not at all,” “several days,” “more than half the days,” and “nearly every day,” respectively, and then adding together the scores for the seven questions. Scores of (0-4) represent normal, (5-9) represent mild, (10-14) represent moderate, and (15-21) represent severe anxiety [5].
Summary of the percentage of physicians working in the frontline, suffering from anxiety, obtained from the selected studies. 1,2,3,4 on the x axis are representing refrence studies [3,4,5,6] respectively.
Exposure to severe and chronic stressors can particularly predispose doctors to experience burnout. During these times there is excessive workload, long working hours, fatigue, emotional interactions, and restricted autonomy, all of it fostering emotional exhaustion, depersonalisation, and a sense of reduced personal accomplishments which is termed as burnout. Burnout among physicians has been reported to increase the risk of mental morbidities such as depression, anxiety, sleep disturbances, fatigue, and even suicide [7]. In addition to the obvious effects on physicians’ lives, these changes may reduce patient access to healthcare compromising the already coping healthcare system to meet population demands. Burnout can drive physicians to make suboptimal decisions or errors in patient care, demonstrate hostility towards patients, disengage from work, and may also increase healthcare expenditures indirectly via higher rates of malpractice claims and absenteeism [8].
Discussion
The deranged psychological assessment can be attributed to a lot of factors. The shortage of PPE and increased working hours along with an increased number of COVID-19 positive patients are the major contributing factors. The risk of spread of infection to family, peers, and self is attributable to increased levels of stress, anxiety, and insomnia. Being young, female, and single is also associated with a poor outcome. Low professional experience and attention towards negative information about the pandemic are also important aspects that cannot be ignored. While stress and worries seem to be limited to the period of exposure to the outbreak, effects in terms of burnout can be long-lasting . Evidence also proposes that physicians working in the healthcare system are more likely to suffer from mental health issues like anxiety than their non-medical counterparts who are also working in the healthcare system. [9].
Studies have shown that many doctors find it difficult to convey to their employers or colleagues about the difficulties being faced by them in terms of mental health. The most common reasons for the same included perceived stigma and anticipated damage to future career prospects which may be further compromised by feelings of shame and failure on the professional front as well as worries about licencse restrictions. In order to tackle the stigma surrounding mental health in the workplace, creating a culture that promotes open communication thereby reducing stigmatiszation of psychological vulnerability can be beneficial. Including activities that encourage a healthy behavioural change such as the anti-stigma campaign “Time to Change” which aims at reducing mental health-related stigma and discrimination can be beneficial. Peer support training programmes such as the Trauma Risk Management programme (TRiM) where non-clinical personnel are trained to monitor and manage colleagues following traumatic events and provide short-term support or access to professional care if required. [10-13].
There can be various ways of mitigating the negative impact of this pandemic on physicians in terms of psychological distress. One of the earliest steps that could be taken to tackle this hurdle is to screen out those who already have a predisposing condition making them more vulnerable than others. Early counselling and intervention can help reduce the incidence of such psychological disorders amongst physicians amidst this pandemic. Physical exercise and adequate rest can greatly reduce stress and improve sleep quality. Aerobic exercises not only improve cardiovascular and pulmonary function but also pave the way to sound sleep and alleviate mental stress. Physical exercise of convenient intensity and adequate quantity can restore psychological stability [14]. There are various online platforms to bust stress which have proven to be effective in many psychiatry research studies [15]. Many evidence-based strategies employable by physicians include mindfulness, stress-management training, self-care efforts, and yoga [16-19]. On the professional front, providing HCWs with adequate protective measures like PPEs along with the frequent provision of information is associated with higher work motivation and could result in less adverse psychological outcomes. Considering the wide availability of smartphones and the internet, online mental health education, online psychological counselling services, and online psychological self-help intervention systems should be developed. Ensuring proper implementation of quarantine rules for HCW could decrease the risk of transmission of infection to family members, thereby alleviating the stress associated with it.
Conclusion(s)
Data collected in this viewpoint may provide an insight regarding the realities of the psychological impact of COVID-19 and prepare ourselves with the necessary tools to mitigate the burden on physicians and ultimately the entire healthcare system. The sudden emergence of such pandemics can pose adverse effects on the health of HCW, especially those on the frontline. Although the negative effects cannot be completely averted, mitigation strategies can be planned beforehand so as to curtail the incidence of psychiatric problems. As their service during these times is crucial for the welfare of the community, failing to address these significant issues can have adverse consequences not only at the individual level, but also in the quality of treatment the patients receives. As the evidence in the viewpoint strongly suggests the prevalence of psychological diseases amongst physicians working in the frontline, the proposed measures can be implemented for the betterment of physicians as well as healthcare response capacity at a systemic level.
[1]. Felice C, Di Tanna GL, Zanus G, Grossi U, Impact of COVID-19 outbreak on healthcare workers in Italy: Rresults from a national e-surveyJ Community Health 2020 45(4):675-83.10.1007/s10900-020-00845-532440724 [Google Scholar] [CrossRef] [PubMed]
[2]. Maunder R, Hunter J, Vincent L, Bennett J, Peladeau N, Leszcz M, The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospitalCanadian Med Asso. Can Med Assoc J 2003 168(10):1245-51.12743065 [Google Scholar] [PubMed]
[3]. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019JAMA Netw Open 2020 3(3):e20397610.1001/jamanetworkopen.2020.397632202646 [Google Scholar] [CrossRef] [PubMed]
[4]. Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E, Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemicsPsychiatry Res 2020 290:11313010.1016/j.psychres.2020.11313032497969 [Google Scholar] [CrossRef] [PubMed]
[5]. Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, Psychological impact of the COVID-19 pandemic on healthcare workers: A cross-sectional study in ChinaGen Psychiatr 2020 33(3):e10025910.1136/gpsych-2020-10025932596640 [Google Scholar] [CrossRef] [PubMed]
[6]. Chatterjee SS, Bhattacharyya R, Bhattacharyya S, Gupta S, Das S, Banerjee BB, Attitude, practice, behavior, and mental health impact of COVID-19 on doctorsIndian J Psychiatry 2020 62(3):257-656.10.4103/psychiatry.IndianJPsychiatry_333_2032773868 [Google Scholar] [CrossRef] [PubMed]
[7]. Kumar S, Burnout and doctors: Prevalence, prevention, and interventionHealthcare (Basel) 2016 4(3):37-45.10.3390/healthcare403003727417625 [Google Scholar] [CrossRef] [PubMed]
[8]. West CP, Dyrbye LN, Shanafelt TD, (Mayo Clinic, Rochester, MN; and Stanford University Medical Center, Stanford, CA, USA). Physician burnout: Contributors, consequences, and solutions)J Intern Med 2018 283:516-29.10.1111/joim.1275229505159 [Google Scholar] [CrossRef] [PubMed]
[9]. Shanafelt TD, Balch CM, Dyrbye L, Bechamps G, Russell T, Satele D, Special report: Suicidal ideation among American surgeonsArch surgery 2011 146(1):54-62.10.1001/archsurg.2010.29221242446 [Google Scholar] [CrossRef] [PubMed]
[10]. Hassan TM, Ahmed SO, White AC, Galbraith N, A postal survey of doctors’ attitudes to becoming mentally illClin Med 2009 9(4):327-32.10.7861/clinmedicine.9-4-32719728504 [Google Scholar] [CrossRef] [PubMed]
[11]. Hassan TM, Sikander S, Mazhar N, Munshi T, Galbraith N, Groll D, Canadian psychiatrists’ attitudes to becoming mentally illBrit J Med Pract 2013 6(3):a619-23. [Google Scholar]
[12]. Chew-Graham CA, Rogers A, Yassin N, I wouldn’t want it on my CV or their records’: Medical students’ experiences of help-seeking for mental health problemsMed Edu 2003 37(10):873-80.10.1046/j.1365-2923.2003.01627.x12974841 [Google Scholar] [CrossRef] [PubMed]
[13]. White A, Shiralkar P, Hassan T, Galbraith N, Callaghan R, Barriers to mental healthcare for psychiatristsPsychiatr Bull 2006 30(10):382-84.10.1192/pb.30.10.382 [Google Scholar] [CrossRef]
[14]. Wu K, Wei X, Analysis of psychological and sleep status and exercise rehabilitation of front-lLine clinical staff in the fight against COVID-19 in ChinaMed Sci Monit Basic Res 2020 26:e92408510.12659/MSMBR.924085 [Google Scholar] [CrossRef]
[15]. Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidenceCurr Psychiatry Rep 2020 22(8):43-64.10.1007/s11920-020-01166-z32651717 [Google Scholar] [CrossRef] [PubMed]
[16]. Regehr C, Glancy D, Pitts A, LeBlanc VR, Interventions to reduce the consequences of stress in physicians: A review and meta-analysisJ Nerv Ment Dis 2014 202:353-59.10.1097/NMD.000000000000013024727721 [Google Scholar] [CrossRef] [PubMed]
[17]. Ruotsalainen JH, Verbeek JH, Marine A, Serra C, Preventing occupational stress in healthcare workersCochrane Database Syst Rev 2015 4:CD00289210.1002/14651858.CD002892.pub525847433 [Google Scholar] [CrossRef] [PubMed]
[18]. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD, Interventions to prevent and reduce physician burnout: A systematic review and meta-analysisLancet 2016 388:2272-81.10.1016/S0140-6736(16)31279-X [Google Scholar] [CrossRef]
[19]. Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysisJAMA Intern Med 2017 177(2):195-205.10.1001/jamainternmed.2016.767427918798 [Google Scholar] [CrossRef] [PubMed]