Leiomyoma of the Breast- A Rare Case Report
Thoppil Reba Philipose1, Meghashree Vishwanath2, Siddharth Mulki3, Sandhya Ilanthodi4
1 Professor and Head, Department of Pathology, A.J. Institute of Medical Sciences and Research Centre, Mangalore, Karnataka, India.
2 Assistant Professor, Department of Pathology, A.J. Institute of Medical Sciences and Research Centre, Mangalore, Karnataka, India.
3 Assistant Professor, Department of General Surgery, A.J. Institute of Medical Sciences and Research Centre, Mangalore, Karnataka, India.
4 Professor, Department of Pathology, A.J. Institute of Medical Sciences and Research Centre, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Meghashree Vishwanath, Assistant Professor, Department of Pathology, A.J. Institute of Medical Sciences and Research Centre, Kuntikana, Mangalore-575004, Karnataka, India.
E-mail: meghavishwanth@gmail.com
Leiomyoma though a common entity encountered in our daily practise, its occurrence in breast is extremely uncommon. There are a very few reported cases of leiomyomas occurring in breast parenchyma. This tumour clinically simulate commonly occurring tumours of breast. Hereby, authors report a case of a mesenchymal neoplasm occurring in breast of a 33-year-old female of child bearing age. The histopathological diagnosis requires careful differentiation from lesions that have smooth muscle proliferation, especially leiomyosarcoma. The most commonly performed treatment is resection of the lesion with free margins. Although breast leiomyoma is rare, it should be considered among the differential diagnosis for breast nodules of benign appearance.
Intraparenchymal, Leiomyosarcoma, Mesenchymal, Smooth muscle
Case Report
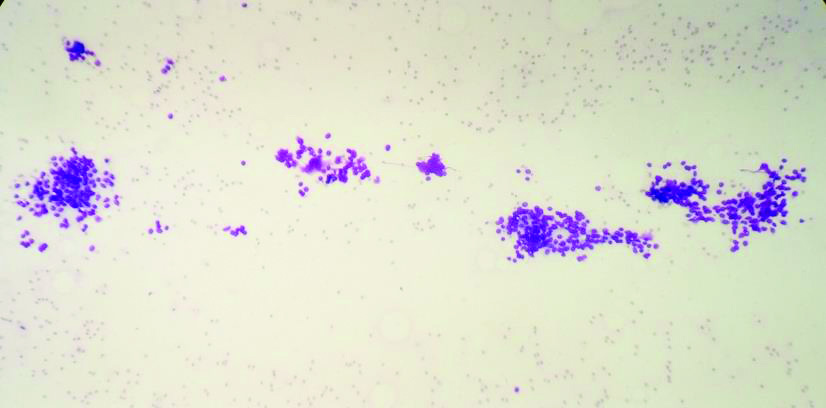
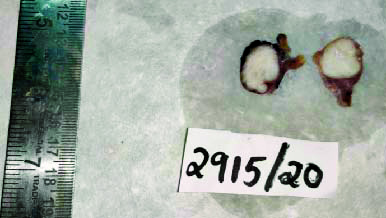
A 33-year-old female presented with history of painless swelling in left breast since 10 days. There was no history of nipple discharge, lactation or any hormonal therapy. A Fine Needle Aspiration Cytology (FNAC) was done and it revealed a benign lesion, probably fiboadenoma [Table/Fig-1]. Following this a lumpectomy was done and sent for histopathological examination. The tumour measured 2.5×1.5×1.5 cm. Cut surface had a grey white lobulated appearance and the tumour was firm in consistency [Table/Fig-2].
Aspirate showing ductal epithelial cells and myoepithelial cells May Grunwald Giemsa Stain (MGG), 10X).
Cut surface showing grey white lobulated appearance.
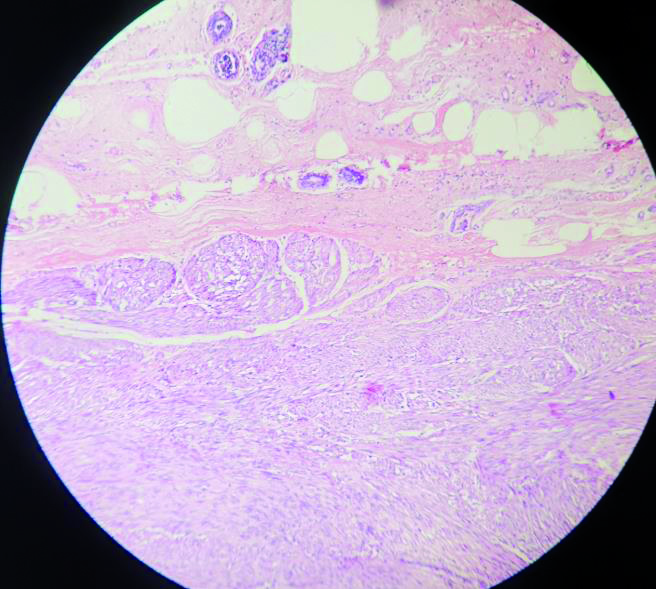
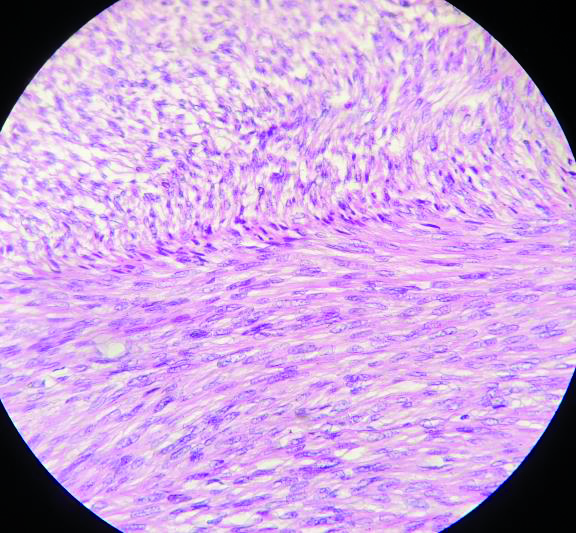
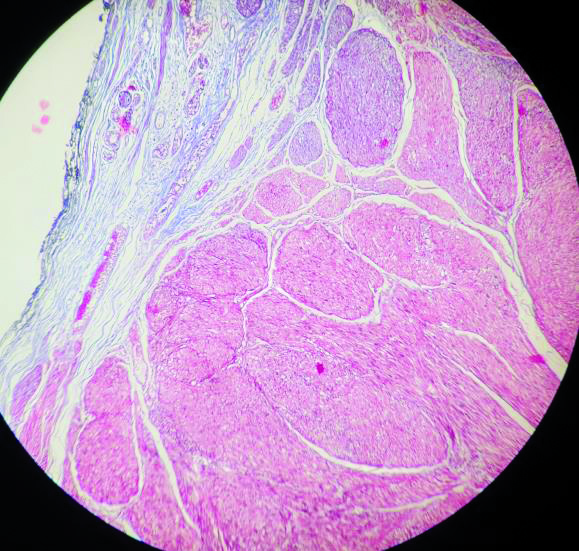
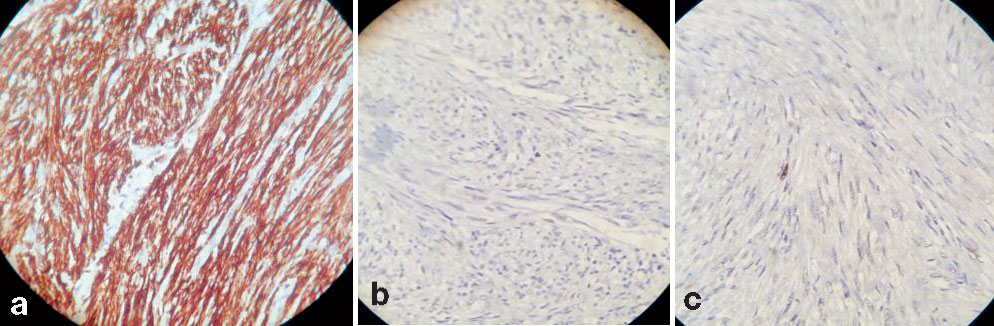
Microscopy showed partially encapsulated well circumscribed tumour composed of intersecting and interlacing fascicles of spindle cells with elongated blunt ended vesicular nuclei and eosinophilic cytoplasm [Table/Fig-3,4]. Mitosis was less than two per 10 high power field (hpf) with no atypia or areas of necrosis. The surrounding breast parenchyma showed features of fibrocystic change. Morphological differentials were between Leiomyoma and a benign neural tumour. Masson’s trichrome highlighted the presence of fibrous capsule and spindle cells as of probable smooth muscle origin [Table/Fig-5]. Immunohistochemistry showed diffuse strong positivity for desmin confirming smooth muscle origin, S-100 negativity which ruled out neural origin and a Ki-67 proliferative index of 8-10% [Table/Fig-6]. Thus a diagnosis of leiomyoma of breast was rendered.
Photomicrograph showing the lesion and surrounding breast parenchyma (H&E, 10X).
Photomicrograph showing intersecting fascicles of spindle cells having elongated blunt ended nucleus with vesicular nuclei (H&E, 40X).
Masson’s trichrome highlighting the fibrous capsule in blue and muscle fibres in red (10X).
Immunohistochemistry showing strong desmin positivity (a), S-100 negativity (b) and low Ki-67 (c).
The surgeon was informed of the involvement of the tumour till the resected margins and cautioned about the possibility of recurrence, at times as leiomyosarcoma in the long run. The patient was explained in detail about the possible unseen future occurrences and a simple mastectomy was done to alleviate all fears. Postoperative follow-up was uneventful with no complaints of swelling/pain. Breast reconstruction was advised for which currently the patient was not willing.
Discussion
Leiomyoma is a benign smooth muscle neoplasm that can occur anywhere in the body. It is considered as one of the most common mesenchymal neoplasms in the uterus and gastrointestinal tract. Its occurrence in breast is extremely rare [1]. To the best of our knowledge, there as less than 35 reported cases of leiomyoma breast in literature.
Smooth muscle tumours of the breast represent <1% of breast neoplasms [1]. Most cases of leiomyoma occur superficially in the skin, especially around the nipple-areola complex, and may affect both men and women, while deeper parenchymal lesions are extremely infrequent and affect only females [2]. Most breast leiomyomas are diagnosed in women of late middle age, and they usually occur in the right breast [3]. However, present case is of a woman in reproductive age and the lesion being in left breast. An increase in the prevelance of leiomyomas of breast with tamoxifen use is reported [3].
The credit of describing leiomyoma in the breast for the first time goes to Strong LW in the year 1913 [4]. There are various theories to explain the occurrence of this tumour in breast. Kaufman HL and Hirsch EF proposed that these tumours take origin from the myocytes around the capillaries in the subcutaneous tissue of breast [5]. Diaz-Arias AA et al., enlisted a set of possibilities for the occurrence of leiomyoma in breast- smooth muscle cells that migrate from the nipple during embryological life, teratoid origin coupled with significant overgrowth of the myomatous elements, a multipotent mesenchymal cell, angiomatous smooth muscle and myoepithelial cells [6].
The histopathologic features of leiomyoma of breast are no different from those occurring anywhere in the body. Interlacing fascicles of spindle cells with elongated cigar shaped nuclei having blunt ends and eosinophilic cytoplasm constitute the microscopy of the tumour. There is no cytologic atypia, mitosis or necrosis. They are stained positively for Vimentin, Desmin and Smooth Muscle Actin (SMA). This spindle cell tumour in breast has a wide range of differentials which include Fibromatosis, Spindle cell metaplastic carcinoma, Myofibroblastoma, Spindle cell variant of adenomyoepithelioma and Leiomyosarcoma [7]. Amongst all, differentiating an intraparenchymal leiomyoma from leiomyosarcoma is of utmost importance as the treatment, rate of recurrence and prognosis totally vary in these two entities. Leiomyosarcomas are characterised by interlacing bundles of smooth cells exhibiting cellular atypia, nuclear hyperchromasia, mitosis (2 to 50 mitotic figures per 10 hpf with an average of 12 per 10 hpf) [8], necrosis and vascular invasion. Presence of even two mitotic figures in 10 hpf accounts for Leiomyosarcoma. This calls for a careful analysis of the tumour. It is of interest to note that Boscaino A et al., in his study suggested terming bland appearing neoplasms with a mitotic activity of 2 per 10 hpf as smooth muscle neoplasms of indeterminate prognosis, instead of ordinary leiomyomas [9].
The management protocol for smooth muscle lesions of breast is surgical excision of lesion with two centimeter margin and sending for histopathological examination. If the smooth muscle neoplasm is benign with free surgical margins, then a follow-up with Magnetic Resonance Imaging (MRI) is recommended. If margins are involved, then there are two options- one is two centimeter margin resection or a regular follow-up. If the lesion turns out to be a leiomyosarcoma confirmed by immunohistochemistry and with involvement of surgical margins, simple mastectomy or quadrantectomy is done with no axillary dissection. If the margins are free, then a regular follow-up with MRI is done. Radiotherapy is mandatory if there is muscle involvement [10].
On FNAC identification of the lesion could not be done as no representative material was obtained from the lesion. The needle probably did not hit the lesion or failed to displace cells from lesion due to its hard nature. The adequate cellularity of the smears of surrounding breast parenchyma made us believe that lesion was aspirated. In this regard, a guided aspiration would have led us into the tumour proper and yielded a better cytodiagnosis. Further, in the lack of literature reference on Ki-67 proliferative index cut-off for leiomyosarcoma in breast, a Ki-67 of 8-10% with involvement of lumpectomy margins could have been a potential threat. The patient and her family members were explained clearly about the management protocols. The patient hailing from a remote village expressed her inability for a regular follow-up after a second surgery of margin resection. In the light of these facts, the team decided not to leave the patient to chance and simple mastectomy was thought to be a wise option. The patient and her family members also wanted a permanent remedy and chose the same.
With reference to this case, further studies regarding Ki-67 cut-off will go a long way in averting mastectomy in cases where atypia and necrosis are absent, which otherwise would be considered for mastectomy in the absence of adequate supporting literature.
Conclusion(s)
Intraparenchymal leiomyomas of breast are rarely encountered. Clinically and radiologically it can mimic other lesions of breast. A guided aspiration is always better while dealing with deep seated lesions. Careful histopathological examination supported by special stains and immunohistochemistry is the key for a definitive diagnosis of this mesenchymal lesion.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 03, 2021
Manual Googling: May 04, 2021
iThenticate Software: May 31, 2021 (15%)
[1]. Kafadar MT, Yalcin M, Gok MA, Aktas A, Yurekli TS, Arslan AI, Intraparenchymal leiomyoma of the breast: A rare location for an infrequent tumorEur J Breast Health 2017 13(3):156-58.10.5152/ejbh.2017.347228894856 [Google Scholar] [CrossRef] [PubMed]
[2]. Sampaio GP, Koch MV, Boechat M, Matos VE, Dos Santos AA, Leiomyoma of the breast: An uncommon tumorRadiol Bras 2016 49(5):343-44.10.1590/0100-3984.2014.013627818553 [Google Scholar] [CrossRef] [PubMed]
[3]. Pourbagher A, Pourbagher MA, Bal N, Oguzkurt L, Ezer A, Leiomyoma of the breast parenchymaAmerican Journal of Roentgenology 2005 185:1595-97.10.2214/AJR.04.145316304020 [Google Scholar] [CrossRef] [PubMed]
[4]. Shah SD, Gupta A, Roy S, Mukhopadhyay S, Intraparenchymal leiomyoma of the breast: A case reportIndian J Surg 2013 75:88-89.10.1007/s12262-011-0367-624426524 [Google Scholar] [CrossRef] [PubMed]
[5]. Kaufman HL, Hirsch EF, Leiomyoma of the breastJ Surg Oncol 1996 62:62-64.10.1002/(SICI)1096-9098(199605)62:1<62::AID-JSO13>3.0.CO;2-V [Google Scholar] [CrossRef]
[6]. Diaz-Arias AA, Hurt MA, Loy TS, Seeger RM, Bickel JT, Leiomyoma of the breastHum Pathol 1989 20:396-99.10.1016/0046-8177(89)90052-X [Google Scholar] [CrossRef]
[7]. Stafyla VK, Gauvin JM, Farley DR, A 53-year-old woman with a leiomyosarcoma of the breastCurr Surg 2004 61:572-75.10.1016/j.cursur.2004.05.00815590026 [Google Scholar] [CrossRef] [PubMed]
[8]. Koerner FC, Mesenchymal lesions. In: Brogi E, Hoda SA, Koerner FC, Rosen PPRosen’s Diagnosis of Breast Pathology4th edNew York:758-60. [Google Scholar]
[9]. Boscaino A, Ferrara G, Orabona P, Donofrio V, Staibano S, De Rosa G, Smooth muscle tumors of the breast: Clinicopathologic features of two casesTumori 1994 80(3):241-45.10.1177/0300891694080003168053085 [Google Scholar] [CrossRef] [PubMed]
[10]. Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, AJCC Cancer Staging Manual 2017 8th edNew YorkSpringer-Verlag10.1007/978-3-319-40618-3 [Google Scholar] [CrossRef]