Parameshwara G conducted first spinal anaesthesia on a labour for the resection of a tuberculous ulceration of the ankle in 1898 [1], since then spinal anaesthesia has assumed immense popularity with the surgeons and anaesthesiologists particularly for lower limb and lower abdominal surgeries. The ease and long history of spinal anaesthesia may give an impression that it is a simple technique with little sophistication but an adequate understanding of the application and complications should be borne by every practitioner.
It is widely known that a fall in blood pressure remains one of the most common side effects of spinal anaesthesia. The cause and its management have been intriguing even after several decades of debate and research. The different methods have been advocated to reduce the incidence of hypotension include trendelenburg position, prophylactic vasopressors, leg wrapping and elevation, use of inflatable boots, prehydration and co-hydration with crystalloids and colloids [2-4]. Among these the prehydraton of fluids has stood the test of time.
Kee NDW et al., studied the efficacy of combination of crystalloid co-hydration and vasopressor infusion. They concluded that the incidence of hypotension in caesarean section after spinal anaesthesia can be completely eliminated with combination of high dose vasopressor infusion along with crystalloid infusion [4]. Kamenik M and Paver-Erzen V recommended that every patient undergoing subarachnoid block should receive crystalloid infusion to prevent decrease in cardiac output [5], whereas Mathru M et al., proved in their study albumin remained in the intravascular compartment longer than the crystalloid and there by reduced the incidence of hypotension after spinal anaesthesia [6].
The purpose of this study was to compare the influence of prehydration with isotonic saline and with polymerised gelatine for spinal induced hypotension in patients undergoing TURP surgery. The comparison of incidence and frequency of hypotension were the primary outcome and the side effects of polymerised gelatin and isotonic saline administration to prevent spinal induced hypotension were secondary outcome in the study.
Materials and Methods
This randomised double-blind study was conducted from April 2006 to April 2008 on patients admitted at Father Muller Medical College Hospital in the Urology Department. Sixty male patients were enrolled for TURP surgery after obtaining informed consent. The Helsinki declaration was respected and the guidelines were followed during the procedure and throughout the study.
Inclusion criteria: Male patients aged between 50-70 years, physical status ASA 1 and ASA 2, patients posted for TURP surgery.
Exclusion criteria: Patients with cardiac and respiratory diseases, raised intracranial tension, patients allergic to local anaesthetic drugs.
Study Procedure
A detailed history and complete clinical examination of patients was done. Routine investigation like haemoglobin, blood grouping, blood sugar, blood urea, serum creatinine, serum electrolytes, ECG, chest X-ray and coagulation tests were done. Patients involved in the study were premedicated with tablet ranitidine 150 mg and diazepam 10 mg orally night prior to the surgery.
The random number table for 60 patients was divided into two groups and sealed envelope were prepared and numbered sequentially. Then the patients were divided according to the envelope randomly. The person administering anaesthesia was not involved in uncoding data. The hemodynamic and other parameters were recorded by another anaesthesiologist who was blinded to study fluids used [Table/Fig-1].
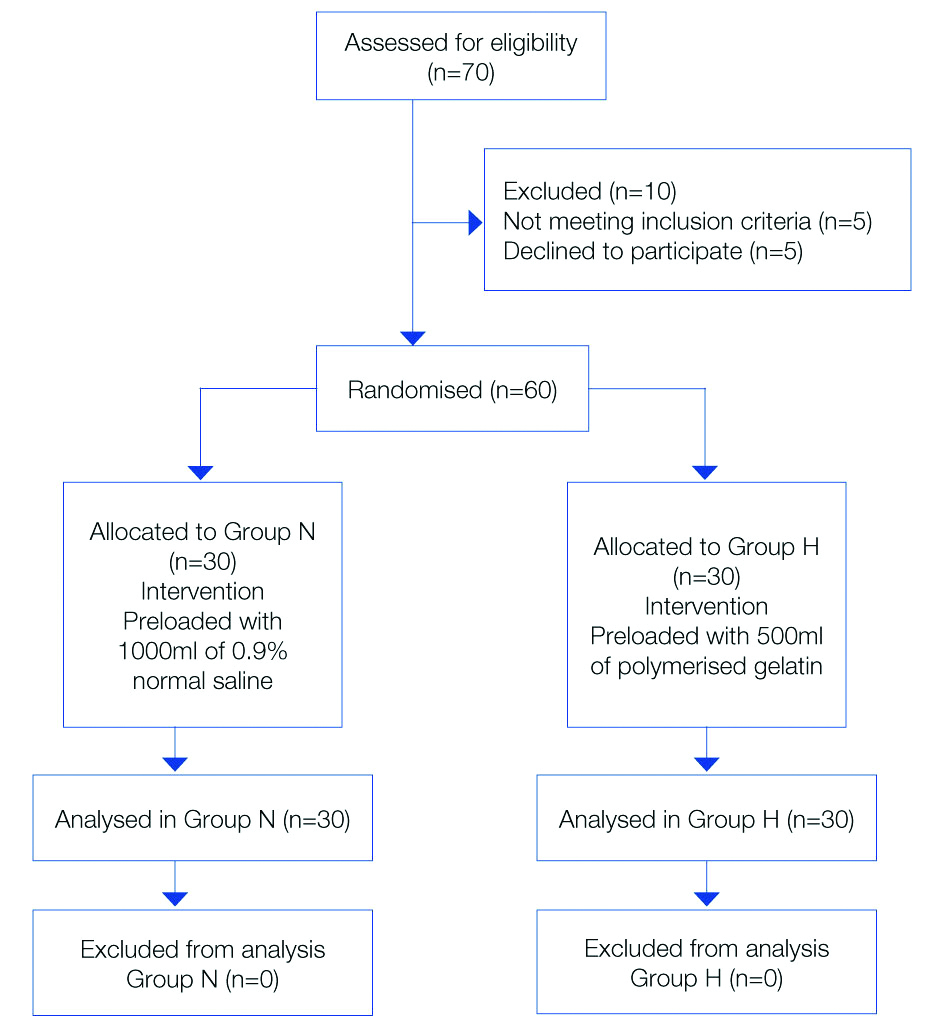
The patients were divided into two groups as follows:
Group N- patients were preloaded with 1000 mL of normal saline
Group H- patients were preloaded with 500 mL of polymerised gelatine
The standard monitors like pulse oximeter, non invasive blood pressure and electrocardiogram were connected to the patient. Vitals were recorded. Intravenous access was secured with 18G cannula. The patients were preloaded with study solutions either polymerised gelatin (Haemaccel, Nicholas Piramal India Ltd.,) 500 mL or 0.9% Normal saline (NS, Fresenius Kabi India Ltd.,) 1000 mL depending on group allocation 15 min prior to the subarachnoid block. After infusion of study solution, vitals were recorded. An average of three readings was considered as baseline recording. The anaesthesiologist, who performed the subarachnoid block was blinded to the group of study solution. Under aseptic precaution subarachnoid block was administered at L3-L4 interface with 3 mL of 0.5% bupivacaine (heavy) (Sensorcaine, Astra zeneca Pharmaceuticals, India) in the lateral position.
After the procedure, patient was positioned supine immediately. The extension of the block was assessed by the pinprick method every 5 minutes intraoperative monitoring included heart rate, systolic blood pressure, diastolic blood pressure, and mean arterial pressure were recorded at every two minutes for first 10 minutes, and then every 10 minutes for 30 minutes after the induction of spinal anaesthesia. Both the groups received infusion of ringer lactate at the rate of 2 mL/min throughout the period of surgery as maintenance fluid. Hypotension was defined as a fall in systolic blood pressure of greater than 30% of the preoperative as advocated by Cousins and Bridenbaugh [19]. Rescue therapy for hypotension comprised of Inj. Mephentermine 6 mg IV and repeated at every two minutes intervals as necessary. Complications and side-effects like nausea and vomiting were recorded throughout period of surgery.
The sample size was calculated based on a pilot study done in two groups with a difference of mean score 2. The power of study 80%, confidence interval of 95% and 90% power yielding, the sample size came out to be 30 patients per group.
Statistical Analysis
Statistical analysis was done using Mann-Whitney U test and analysis of variance for repeated measures (ANOVA). Chi-square test was used to find out possible associations. All the statistical calculations were done by statistician using software Statistical Package for Social Sciences (SPSS) version 16.0. P<0.05 was considered as significant.
Results
Demographic variables were comparable between the two groups [Table/Fig-1] with respect to age, weight and height [Table/Fig-2]. Level of sensory blockade attained was between T6-T8 dermatomal levels in all patients of both the groups, as assessed by pinprick method. The proportion of patients with sensory level attained at 10 minutes T8 was 18 (60%) in both the groups. Sensory level of T6 was 12 (40%) in group N and 11 (36%) in group H. One patient in group N had attained block extending to T4. The results were not statistically significant [Table/Fig-3].
| Variables | Group H (n=30) | Group N (n=30) | p-value |
|---|
| Age (y) | 63.47±4.15 | 64.37±4.86 | 0.279 |
| Weight (kg) | 65.20±8.32 | 64.43±5.63 | 0.72 |
| Height (cm) | 164.87±4.38 | 163.43±3.69 | 0.54 |
Values are in Mean±SD; Chi-square test used to calculate p-value; p<0.05 significant
Comparison of clinical data between the two groups.
| Variables | Group N | Group H | p-value |
|---|
| Incidence of hypotension§ | 27/30 (90%) | 18/30 (60%) | 0.19 |
| Time to hypotension (min)§ | 6.93±6.40 | 10.93±11.21 | 0.24 |
| Maximum fall of MAP (mm Hg)* | 77.90±10.71 | 79.07±7.04 | 0.006 |
| Lowest systolic BP (mm Hg)* | 97±18.9 | 102.3±9.26 | 0.003 |
| Lowest diastolic BP (mm Hg)* | 64.67±10.30 | 66.37±5.43 | 0.737 |
| Maximum heart rate (bpm)* | 84.20±12.15 | 80.9±9.5 | 0.545 |
| Maximum sensory block (T4) | 0 | 1 (4%) | 0.265 |
| Minimum sensory block (T8) | 18 (60%) | 18 (60%) | 0.372 |
| Total mephentermine dose (mg)§ | 3.83±2.58 | 1.10±1.32 | 0.03 |
| Incidence of nausea and vomiting§ | 1 (3%) | 0 | 0.07 |
Hypotension is defined as SBP<30% of baseline; p<0.05 is significant; Analysis of variance for repeated measures; *ANOVA, §chi-square test
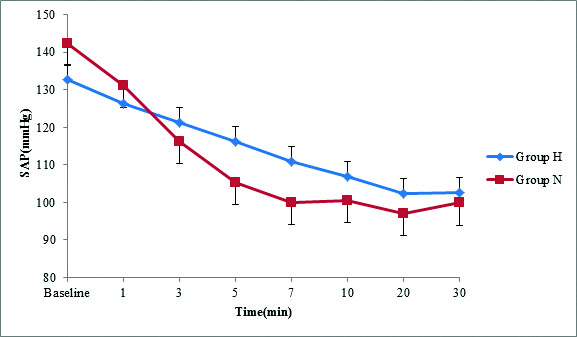
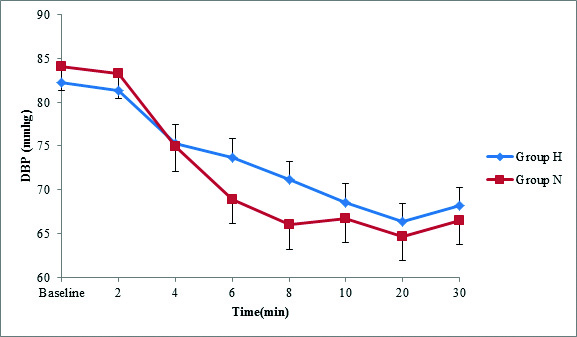
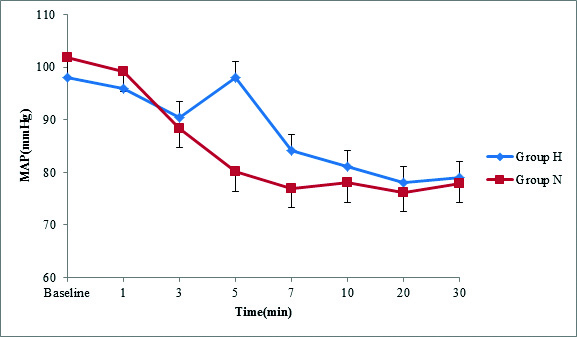
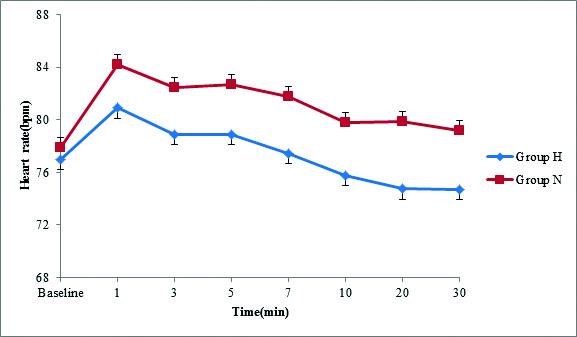
After spinal anaesthesia, the mean systolic blood pressure decreased in both the groups [Table/Fig-4] and it was lower in group N compared to group H. In both the groups, the decrease in systolic blood pressure from baseline was highly significant (p<0.001) throughout the period of observation. There was fall in diastolic blood pressure throughout the period of observation. The maximum fall was noted at 20th minute in both the groups. The significant fall (p<0.05) in diastolic was noted at 5th and 7th minute in group N compared to group H [Table/Fig-5]. A highly significant (p<0.01) difference in mean arterial pressure was noted in group N at 3rd, 5th, 7th and 10th minute after spinal anaesthesia when compared to group H [Table/Fig-6]. The baseline heart rate values were similar in both the groups and increased significantly after spinal anaesthesia. There was highly significant (p<0.01) difference in heart rate in group N compared to Group H after spinal anaesthesia [Table/Fig-7]. Vasopressor was required in 27 patients in group N compared to 18 in group H which was highly significant (p<0.001). The incidence of hypotension was 27 (90%) in group N compared to 18 (60%) in group H. The dose of mephentermine required in group N and group H was 3.84±2.58 mg and 1.10±1.32, respectively. There was no statistical difference in the incidence of nausea and vomiting between the groups [Table/Fig-3].
Mean systolic blood pressure.
Repeated measures ANOVA was used, p=0.003
Mean diastolic blood pressure.
Repeated measures ANOVA was used, P=0.737
Mean arterial blood pressure.
Repeated measures ANOVA was used, P=0.006
Heart rate.
Repeated measures ANOVA was used, P=0.545
Discussion
Intravenous fluid administration prior to subarachnoid block has been found to be safe and is an accepted practice in the prevention of spinal induced hypotension. Intravenous fluids per se do not reverse decrease in systemic resistance, but rather they increase the cardiac output [7]. Both crystalloids and colloids have been used in the management of spinal induced hypotension. Most of studies assessed in the obstetrics populations i.e., caesarean section and studies on other surgeries is less [6,8-10]. The present study is on elderly male patients posted for TURP surgery. In this study, the authors chose polymerised gelatin as colloid because it is included in the WHO list of essential drugs [11].
At diffusion equilibrium, crystalloid solution distributes in the ratio of approximately 1:3 between intra and extra vascular compartments, so that in adults around 1.2 litres will suffice for the compensation of blood pooling during spinal anaesthesia [12]. In this study one litre of isotonic saline 0.9% and 500 mL of polymerised gelatin were used to prevent spinal induced hypotension.
The maximum fall in the blood pressure was noted in the first 15 to 20 minutes after the subarachnoid block. So, first half an hour was the most vulnerable period. So, we chose initial 15 minutes as the period of preloading. On the contrary, Critchley LAH and Kee NDW suggested preloading at the time of subarachnoid block is more appropriate because of the progression of block and consequent vasodilatation [4,13]. In the present study, there was a significant fall in the systolic blood pressure in both the groups up to 30 minutes. The maximum hypotension occurred at 10 to 15 minutes after spinal anaesthesia. Similar observation was found in another study and the reduction in the incidence of hypotension was from 92% to 57% [15]. The authors concluded that fall in blood pressure is inevitable but the incidence of hypotension can be reduced after preloading. In this study, the incidence of hypotension was 90% in normal saline group and 60% in haemaccel group. This is consistent with the study conducted by Siddik S et al., on pregnant females undergoing caesarean section under spinal anaesthesia [8]. In contrast, the study conducted by Kamenik M et al., did not find any fall in blood pressure in the colloid group [6]. On the contrary, Vercauteren V et al., concluded that high volumes of intravenous fluids, even containing gelatin may not prevent cardiovascular instability, but they suggested that more attention should be paid onto the choice of regime [16]. The study conducted by Baraka AS et al., was on ASA2 and ASA3 patients, who are usually associated with medical problems underwent TURP surgery [20]. The co-morbid conditions affected incidence of hypotension in their study. Hence, the conclusions of their study cannot be attributed to spinal anaesthesia.
Many authors suggest that crystalloid preloading is not effective in reducing hypotension after spinal anaesthesia, as 75% of infused volume diffuse into the interstitial spaces and its efficacy in expanding the plasma volume is only transient [6,9,10]. Large volumes of crystalloids can decrease oxygen carrying capacity of the blood due to haemodilution and are associated with the risk of pulmonary and peripheral oedema due to accumulation of fluids in the extravasular space [10,17]. Colloids are mainly confined to the intravascular space because of their oncotic pressure. Hypertonic colloid solutions mobilise fluids from the interstitial space into the intravascular space. As colloid solution contains larger molecules, they do not decrease the plasma colloid pressure as much as crystalloid solutions, hence intravascular volume is maintained when compared to the crystalloid administration.
In this study, the vasopressor required in haemaccel group was 18 (60%) compared to crystalloid it is 27 (90%). This finding is probably due to the patient’s age. Most of the patients were above 40 years and this has been identified as a risk factor for the development of hypotension. The mean heart rate was higher in the crystalloid group than in colloid group. This was similar to other studies [14,18].
The spinal induced hypotension leading to cerebral hypoxia has been attributed as the cause for nausea and vomiting. There was no statistically significant incidence of side-effects in both the groups in this study. There were no complications like anaphylactic reaction to haemaccel or TURP syndrome. This could be because study population was limited to observe these complications.
The present study showed that preloading of fluids either with colloids or crystalloids prior to subarachnoid block reduces the incidence of hypotension but not completely eliminate it, also showed that colloids offset hypovolemia and hypotension more effectively than crystalloids in patients undergoing TURP surgery.
Limitation(s)
The selection of preloading fluid is specific for both crystalloid and colloid solution in this study. There is a scope for further study on different types of preloading fluids in both the groups for the accurate results. The sample size is small to draw a conclusion on precession of results. Lastly, other minor variables like blood loss, pre-existing extra cellular fluid volume, inter comparison of hemodynamic variables for the different levels of sensory and motor block were not assessed to get a precise results.
Conclusion(s)
From the observations and analysis of the present study, it can be concluded that preloading with either crystalloid or colloid solutions prior to subarachnoid block reduces the incidence of hypotension. Also, that colloids reduce hypovolemia and hypotension more effectively than crystalloids in patients posted for TURP surgery.
Values are in Mean±SD; Chi-square test used to calculate p-value; p<0.05 significant
Hypotension is defined as SBP<30% of baseline; p<0.05 is significant; Analysis of variance for repeated measures; *ANOVA, §chi-square test