Mass Forming Chronic Pancreatitis Mimicking a Pancreatic Neoplasm: A Case Report
Sarang Gosavi1
1 Consultant, Department of Radiodiagnosis, Shri Siddhivinayak Ganapati Cancer Hospital, Miraj, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sarang Gosavi, Consultant, Department of Radiodiagnosis, Shri Siddhivinayak Ganapati Cancer Hospital, Sangli Road, Miraj, Maharashtra, India.
E-mail: saranggosavi14@gmail.com
Chronic pancreatitis can present as a focal inflammatory mass mimicking pancreatic neoplasm and also it has increased risk of developing pancreatic cancer. Even with the help of multiple new imaging modalities, convincing differentiating points between these two entities is not available. Hereby, the author present a case of 50-year-old female with epigastric pain since one month. No significant past history or any history of addictions was present. On clinical examination, there was tenderness in epigastric region, however no lump could be felt. Her laboratory parameters revealed, raised bilirubin levels. Amylase and lipase levels were slightly raised. Computed Tomography (CT) revealed heterogeneously enhancing mass involving head and uncinate process of pancreas with loss of fat planes between lesion and superior mesenteric vessels, atrophic pancreas with dilated pancreatic duct and multiple ductal calculi. CT guided biopsy of pancreatic mass was performed. Histopathology revealed pancreatic tissue with fibrocollagenous and fibroadipose tissue with dense and diffuse infiltration by mononuclear cells, histiocytes and a few foamy macrophages suggestive of acute on chronic inflammation with no evidence of any malignant cells.
Computed tomography, Histopathology, Inflammatory changes
Case Report
A 50-year-old female presented to the Emergency Department with epigastric pain since one month aggravated in last two days. There was no significant past history or any history of addictions. On clinical examination, there was tenderness in epigastric region, however no lump could be felt. Her laboratory parameters revealed, raised bilirubin levels (3.2 mg/dL), amylase (208 U/L) and lipase (210 U/L) levels were marginally raised.
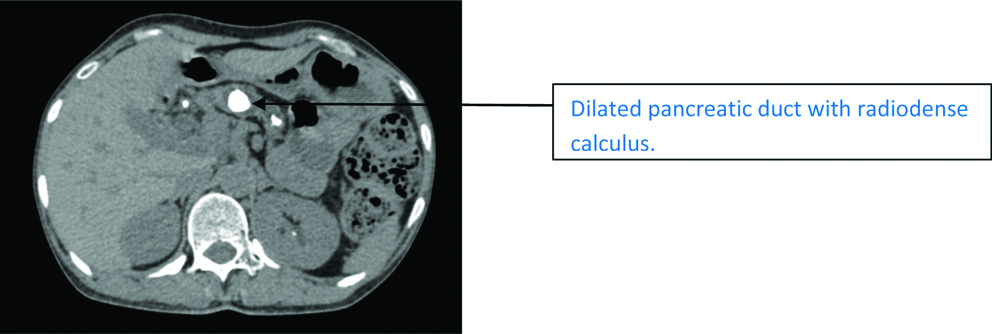
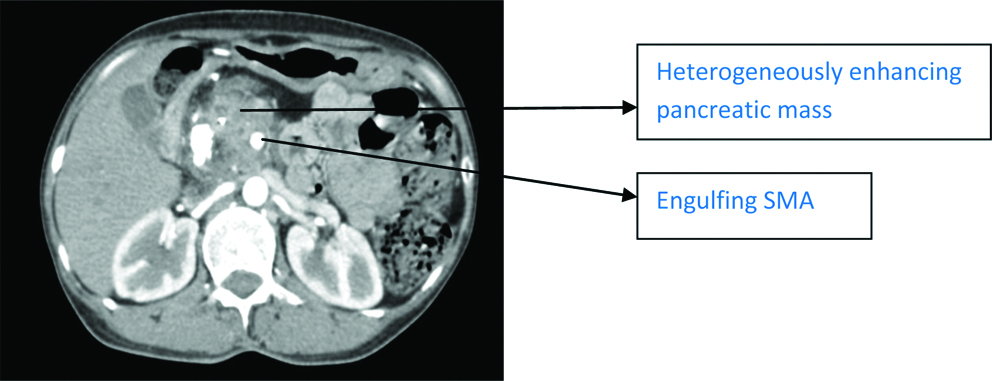
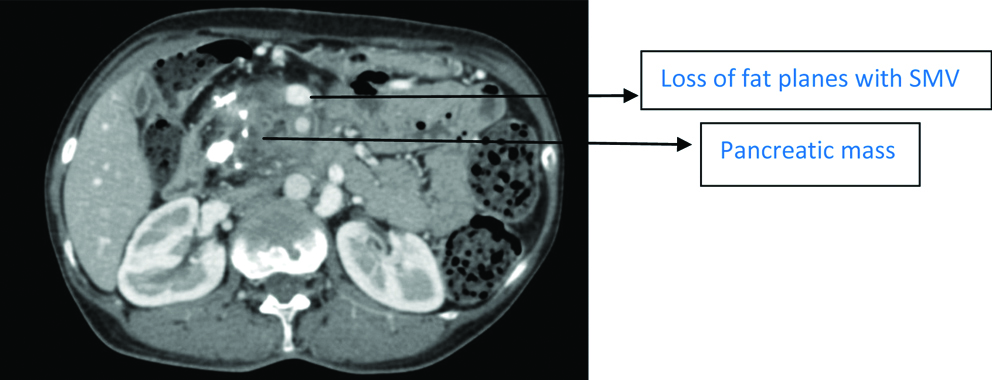
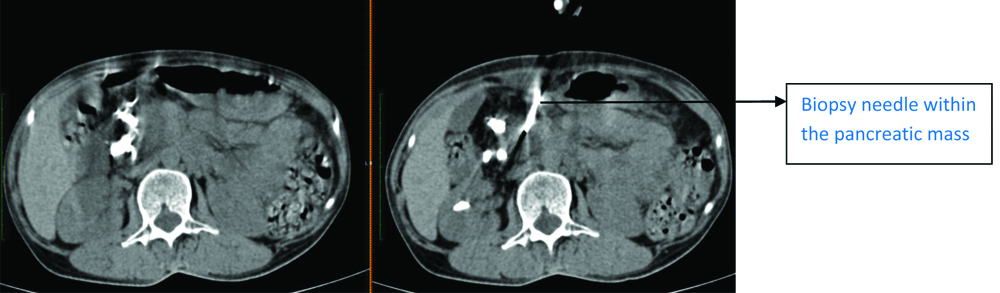
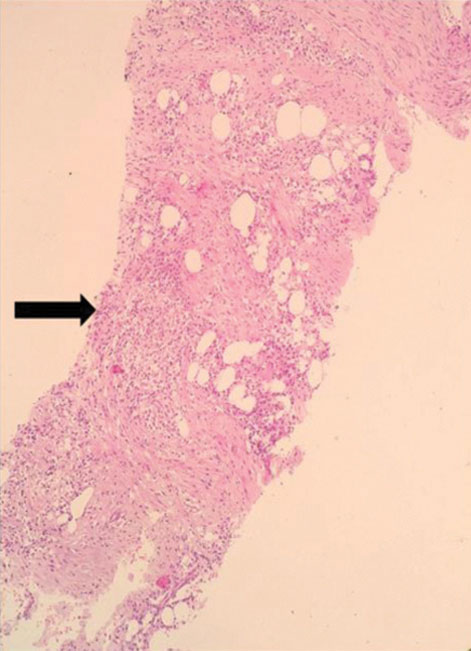
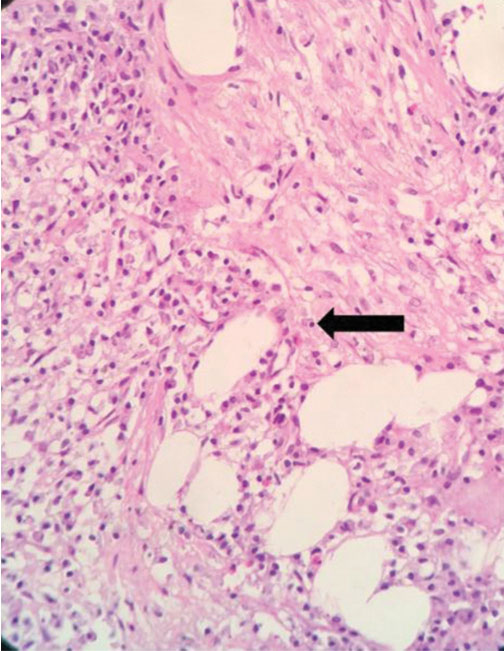
On Ultrasonography, an ill-defined hypoechoic mass was noted in the head of pancreas with multiple ductal calculi. CT revealed atrophic pancreas with dilated pancreatic duct and multiple ductal calculi [Table/Fig-1] and heterogeneously enhancing mass involving head and uncinate process of pancreas with loss of fat planes between lesion and superior mesenteric vessels [Table/Fig-2,3]. Common Bile Duct (CBD) was dilated and measured 8 mm, however there was no evidence of central or peripheral intrahepatic biliary radical dilatation. ‘Double duct sign’ was positive. Duct to parenchyma ratio was >0.34. The SMA:SMV ratio was <1. Moderate fat stranding was noted surrounding the lesion. Findings on CT favoured both mass forming pancreatitis as well as pancreatic adenocarcinoma. Hence, a CT guided biopsy of pancreatic mass was performed [Table/Fig-4]. Histopathology revealed pancreatic tissue with fibrocollagenous and fibroadipose tissue with dense and diffuse infiltration [Table/Fig-5] by mononuclear cells, histiocytes and a few foamy macrophages [Table/Fig-6] suggestive of acute on chronic inflammation with no evidence of any malignant cells.
Computed Tomography (CT) non enhanced axial image shows dilated pancreatic duct with multiple ductal caculi.
CT arterial phase axial image shows heterogeneously enhancing mass in the head and uncinate process of pancreas engulfing the Superior Mesenteric Artery (SMA).
CT venous phase axial image shows a hypoattenuating mass in head and uncinate process of pancreas with loss of fat planes with Superior Mesenteric Vein (SMV).
Axial images of CT guided biopsy of pancreatic mass.
Fibroadipose tissue infiltrated by inflammatory cells (4X).
High power shows infiltration by plasma cells, lymphocytes, histiocytes and few foamy macrophages (10X).
Because of the conclusive histopathology diagnosis, surgery was avoided. Patient was started on corticosteroids and other anti-inflammatory drugs. After one week, the symptoms settled down and the patient was referred to a non cancer hospital. No follow-up of the patient was done thereafter. Corticosteroids have therapeutic potential and hence, reduce the severity of repeat episodes of acute inflammation in chronic pancreatitis [1]. The patient was started on 1 mg/kg prednisone which was supposed to be continued for four weeks followed by tapering. Post one week, the patient was discharged and lost to follow-up.
Discussion
Chronic pancreatitis is a syndrome characterised by chronic and progressive inflammation, fibrosis and scarring leading to damage to the pancreatic cells and tissue. Most common cause of chronic pancreatitis is alcoholic pancreatitis followed by gall stones. Other causes include drugs, hyperlipedemia and idiopathic causes. The patients generally present with vague abdominal pain, pancreatic insufficiency, secondary cancer [2].
Even in presence of radiological findings of chronic pancreatitis it is not always possible to differentiate between mass forming chronic pancreatitis and pancreatic neoplasm especially adenocarcinoma. Misdiagnosis of pancreatic neoplasm at imaging may lead to unwanted surgery while mass formation secondary to chronic pancreatitis can be treated medically. Therefore, it is important to distinguish these two entities to prevent as they have different treatment protocols [3,4].
Various radiological modalities like Perfusion CT, dual energy CT, 18 Fluoro-D-Glucose (FDG) Positron Emission Tomography (PET)/CT combined with carbohydrate antigen 19-9, dynamic Magnetic Resonance Imaging (MRI), diffusion weighted MRI and quantitative ultrasound elastography are used to differentiate mass forming chronic pancreatitis from pancreatic adenocarcinoma, however it is not always possible to differentiate these two entities [5]. On CT, both mass forming pancreatitis and adenocarcinoma are typically hypoenhancing lesions [6]. Findings of chronic pancreatitis like atrophic pancreas with parenchymal or ductal calcifications favours focal mass is likely due to inflammatory changes [7]. ‘Duct penetrating sign’ and pancreatic duct-to-parenchyma ratio of less than 0.34 are supplementary findings in favour of mass forming pancreatitis [8]. Findings of a pancreatic adenocarcinoma are a mass with ill-defined margins with multiple secondary signs like abrupt cut off of the pancreatic duct, upstream pancreatic duct dilatation and decreased enhancement in the pancreatic parenchyma [9]. Similar case has been reported by Massimo T et al., where no accurate preoperative diagnosis was possible [10]. Multiple biopsies were inclusive and patient underwent Whipple pancreatico dudodenectomy. Histopathology diagnosed it as mass forming pancreatitis.
In another case by Ohtsubo K et al., reported a case of pancreatic cancer in young man in which it was difficult to discriminate between pancreatic cancer and mass forming pancreatitis or autoimmune pancreatitis on the basis of imaging modalities [11]. This case report highlights the dilemma faced by radiologist in making a conclusive diagnosis of mass forming pancreatitis or pancreatic carcinoma as both have overlapping features and how CT can be useful to take sample for tissue diagnosis which remains gold standard.
Conclusion(s)
Pancreatic adenocarcinoma is much more common than mass forming chronic pancreatitis. However, even with multiple newer advanced modalities and ancillary findings favouring either, it is not always possible to differentiate radiologically between a mass forming chronic pancreatitis and a pancreatic neoplasm, so CT or endoscopic ultrasound guided biopsy of the lesion is helpful. Histopathology remains gold standard for an accurate diagnosis.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 30, 2021
Manual Googling: Apr 20, 2021
iThenticate Software: Apr 28, 2021 (10%)
[1]. DiMagno MJ, DiMagno EP, Chronic pancreatitisCurr Opin Gastroenterol 2011 27(5):452-59.10.1097/MOG.0b013e328349e33321844753 [Google Scholar] [CrossRef] [PubMed]
[2]. Pham A, Forsmark C, Chronic pancreatitis and update of etiology, risk factors and managementF1000 research 2018 7(F1000 Faculty Rev):60710.12688/f1000research.12852.129946424 [Google Scholar] [CrossRef] [PubMed]
[3]. Dutta AK, Chacko A, Head mass in chronic pancreatitis: Inflammatory or malignantWorld J Gastrointest Endosc 2015 7(3):258-64.10.4253/wjge.v7.i3.25825789097 [Google Scholar] [CrossRef] [PubMed]
[4]. Schima W, Böhm G, Rösch CS, Rosch CS, Klaus A, Fugger R, Mass-forming pancreatitis versus pancreatic ductal adenocarcinoma: CT and MR imaging for differentiationCancer Imaging 2020 20:5210.1186/s40644-020-00324-z32703312 [Google Scholar] [CrossRef] [PubMed]
[5]. Jee KN, Mass forming chronic pancreatitis mimicking a pancreatic cystic neoplasm: A case reportWorld J Gastroenterol 2018 24(2):297-302.10.3748/wjg.v24.i2.29729375215 [Google Scholar] [CrossRef] [PubMed]
[6]. Wolske KM, Ponnatapura J, Kolokythas O, Burke LM, Tappouni R, Lalwani M, Chronic pancreatitis or pancreatiuc tumor? A problem-solving approachRadioGraphics 2019 39:1965-82.10.1148/rg.201919001131584860 [Google Scholar] [CrossRef] [PubMed]
[7]. Choueiri NE, Balci NC, Alkaade S, Burton FR, Advanced imaging of chronic pancreatitisCurr Gastroenterol Rep 2010 12(2):114-20.10.1007/s11894-010-0093-420424983 [Google Scholar] [CrossRef] [PubMed]
[8]. Eloubeidi MA, Luz LP, Tamhane A, Khan M, Buxbaum JL, Ratio of pancreatic duct caliber to width of pancreatic gland by endosonography is predictive of pancreatic cancerPancreas 2013 42(4):670-79.10.1097/MPA.0b013e31827305b823271395 [Google Scholar] [CrossRef] [PubMed]
[9]. Tamada T, Ito K, Kanomata N, Sone T, Kanki A, Higaki A, Pancreatic adenocarcinomas without secondary signs on multiphasic multidetector CT: Association with clinical and histopathologic featuresEur Radiol 2016 26(3):646-55.10.1007/s00330-015-3880-326084602 [Google Scholar] [CrossRef] [PubMed]
[10]. Massimo T, Giovanni M, Sonia I, Bianco R, Focal mass forming chronic pancreatitis: Indistinguishable from pancreatic carcinoma?Eurorad Case:14732 [Google Scholar]
[11]. Ohtsubo K, Watanabe H, Okada G, Tsuchiyama T, Mouri H, Yamaguchi Y, A case of pancreatic cancer with formation of mass mimicking alcoholic or autoimmune pancreatitis in a young man. Possibility of diagnosis by hypermethylation of pure pancreatic juiceJournal of Pancreas 2008 9(1):37-45. [Google Scholar]