Vitamin D as a Substitute of Catheter Ablation in a Paediatric Patient with High Burden Premature Ventricular Contractions: A Case Report
Gabriel Cismaru1, Cecilia Lazea2, Simona Cainap3, Daniela Iacob4
1 Assistant Professor, Department of Cardiology, Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Cluj, Romania.
2 Associate Professor, Department of Paediatric Cardiology, Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Cluj, Romania.
3 Assistant Professor, Department of Paediatric Cardiology, Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Cluj, Romania.
4 Associate Professor, Department of Paediatric Cardiology, Iuliu Hatieganu University of Medicine and Pharmacy, Cluj-Napoca, Cluj, Romania.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Gabriel Cismaru, Viilor 46-50 Rehabilitation Hospital, Cluj-Napoca, Cluj, Romania.
E-mail: gabi_cismaru@yahoo.com
Catheter ablation is established as a treatment option for patients with high number Premature Ventricular Contractions (PVCs). However, complications can occur like cardiac tamponade, coronary artery injury or infectious endocarditis. Reversible causes such as hypocalcaemia, hypomagnesaemia and hypokalemia can be responsible for PVCs. Here, a case of nine-years-old boy, with vitamin D deficiency that presented high number PVCs which corrected using vitamin D dietary supplementation was described. Patient was hospitalised in the Cardiology Department for catheter ablation of PVCs. He presented with shortness of breath during football matches and asthenia. Electrocardiography (ECG) and Holter ECG demonstrated high number PVCs with a morphology consistent of Right Ventricular Outflow Tract (RVOT) origin. Catheter ablation was postponed until Vitamin D came to normal values. Dietary supplementation was performed, together with Holter ECG monitoring. After vitamin D normalisation, PVC burden reduced significantly without the need of catheter ablation or antiarrhythmic drugs. Catheter ablation and antiarrhythmic drugs can be avoided in patients with frequent PVCs and vitamin D deficiency.
Cholecalciferol, Dilated cardiomyopathy, Holter electrocardiography, Right ventricular outflow tract
Case Report
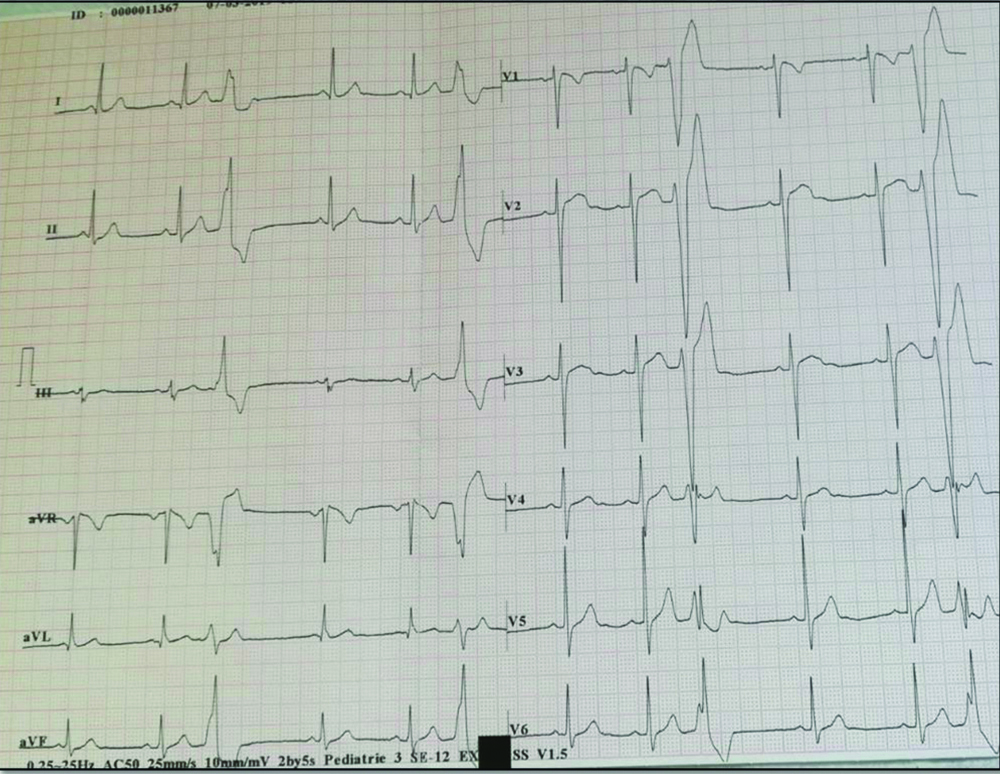
A nine-year-old boy, football player was referred to the Cardiology Department for catheter ablation of high number PVCs (18.400 /24 hours). He was hospitalised three months before his presentation in the Paediatric Clinic for effort dyspnoea and asthenia. ECG showed ventricular bigeminism [Table/Fig-1,2] with Left Bundle Branch Block (LBBB)-like morphology and superior axis of the PVC consistent with a right ventricular outflow tract (RVOT) origin. His echocardiography was normal without signs of cardiomyopathy (normal dimensions of the left ventricle with Ejection Fraction (EF) =60%).
Twelve lead ECG showing PVCs with an LBBB-like morphology with transition in lead V5, consistent with an RVOT origin.
LBBB: Left bundle branch block; RVOT: Right ventricular outflow tract; ECG: Electrocardiography; PVC: Premature ventricular contractions
On 24 hours Holter ECG the patient had multiple runs of 3 consecutive PVCs.
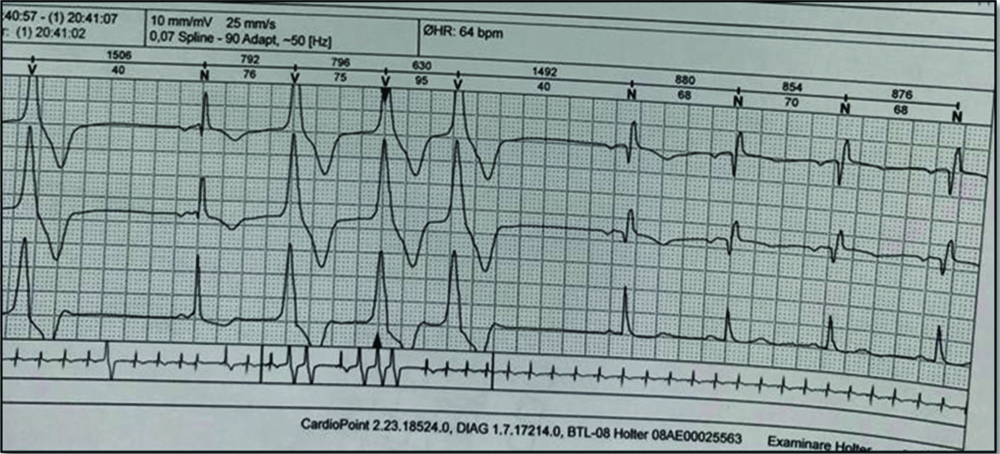
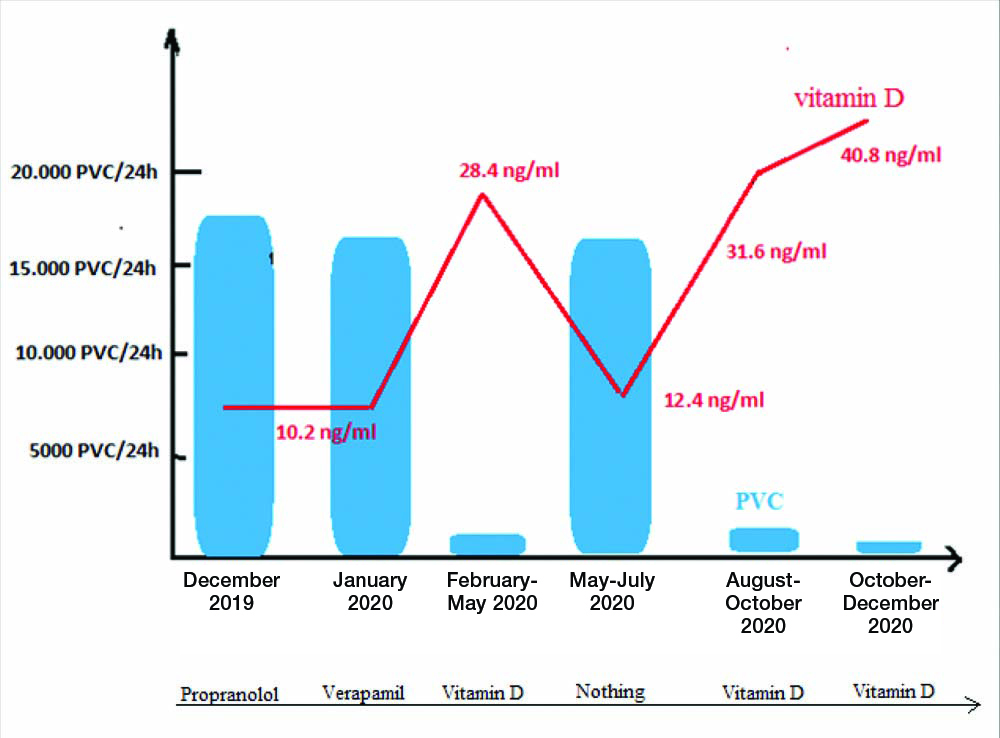
The laboratory tests revealed normal for complete blood count and biochemistry. The only value which was found abnormal was 25- Hydroxyvitamin D (25-OH Vitamin D) i.e. 10.2 ng/mL (normal value >30 ng/mL) although calcium in the blood was normal. Treatment with betablockers was started: Propranolol 10 mg thrice a day for one month, with a mild decrease in the number of PVCs: 17.940/24 hours. The treatment was further changed with Verapamil 3×40 mg/day for one month without significant decrease in the number of PVCs 17.420/24 hours. Therefore, the paediatric cardiologist decided to send the patient for catheter ablation of PVCs. Before catheter ablation, the authors decided to supplement vitamin D and then proceed with the Electrophysiology (EP) study. After 10 days of treatment with 2000 units/day the child felt better, with no PVC on 12-lead ECG. The authors decided to stop Verapamil and continue only with vitamin D for three months and re-evaluate the indication of catheter ablation afterwards.
After three months of vitamin D supplementation, PVCs number decreased to 920 /24 hours, combined with an increase in 25-OH Vitamin D to 28.4 ng/mL. The ablation procedure was canceled and the child was advised to practice performance football. After four months, the parents of the child returned as the PVCs reappeared with the same shortness of breath during football games. Before any treatment, 25-OH-Vitamin D was reassessed and authors found a decrease to 12.4 ng/mL associated with an increase in PVC number: 17.100/24 hour as the child stopped vitamin D supplements. Therefore authors decided to continue with long-term vitamin D supplementation with follow-up at 3, 6 and 12 months.
After three months, the level of vitamin D was 31.6 ng/mL with a decrease of PVCs to 1400/24 hour and after six months, the level of vitamin D was 40.8 ng/mL with a further decrease to 412 PVCs/24 hours [Table/Fig-3]. The patient remained without any antiarrhythmic drug and was treated only with vitamin D supplementation. Informed written consent was obtained from the patient’s father for the publication of this clinical case report except for the images with the child’s face or body.
Relationship between number of PVCs during Holter EKG and 25-OH Vitamin D concentration.
EKG: Electrocardiogram; 25-OH Vitamin D: 25-Hydroxyvitamin D
Discussion
In the vast majority of cases, PVCs have no known cause or occur spontaneously. Common aetiologies include caffeine consumption, high levels of catecholamines, anxiety, and electrolyte imbalance such as low potassium, low magnesium, and low or high calcium [1].
PVCs are common in the general population. They are present in 75% of healthy individuals when monitored with a 48-hour Holter EKG [2]. However, a high burden PVCs can be threatening as it can induce arrhythmogenic cardiomyopathy with dilated left ventricle and reduced EF. Therefore, when PVC burden is high >15%/24 hours catheter ablation is recommended. The success rate of catheter ablation is 94%, on the contrary, the complication rate has been reported 3.1 to 5.2%, among several studies. The most dangerous complications are: cardiac tamponade, coronary artery damage and endocarditis. PVC treatment includes electrolyte correction (hyper/hypocalcaemia, hypokalemia, hypomagnesemia), correct oxygenation (hypoxia, hypercapnea), treatment for hyperthroidism, and avoidance of caffeine and tobacco which might imbalance the adrenergic status and promote PVCs. Hypocalcaemia was demonstrated to trigger both PVCs and sustained Ventricular Tachycardia (VT) [3,4].
Altered vitamin D metabolism can lead to hypocalcaemia or normal calcaemia with inadequate use of calcium at the level of myocardium or skeletal muscles [6]. The main function of vitamin D is to regulate the absorption of calcium from the intestine, maintain the homeostasis of calcium in the blood, bones and muscles. The present report demonstrated that low levels of vitamin D can trigger PVCs, moreover are a reversible cause which can be treated with dietary supplementation.
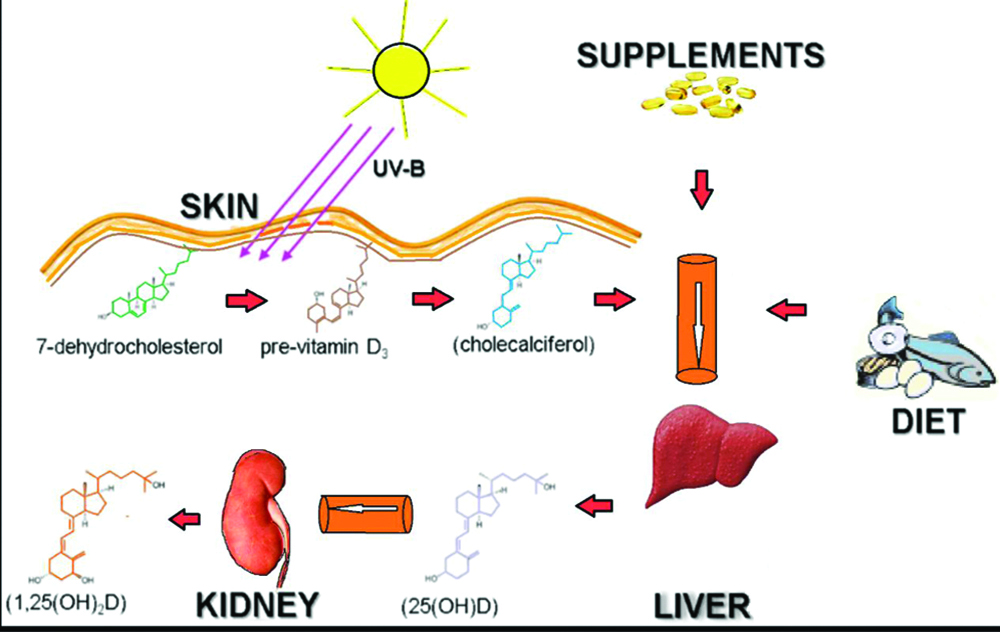
Vitamin D is provided by the nutritional intake and synthesis at the skin level, which is done by the intervention of the sun’s type B ultraviolets. At the liver level it is converted to 25-hydroxyvitamin D. After a further hydroxylation in the kidney gives birth to 1.25 dihydroxyvitamin D, the active form of vitamin D. The concentration of 1,25-(OH) two vitamin D (calcitriol) reflects the activity of 1-alpha renal hydroxylase [Table/Fig-4]. Although calcitriol is the most potent metabolite of vitamin D, 25-OH vitamin D (calcidiol) reflects more accurately the body’s reserves and is therefore preferred as an initial test for assessing vitamin D status. The recommendations for determining 1,25- (OH) 2 vitamin is as second line test for assessing the status of vitamin D, especially in patients with renal disorders.
Structure and biosynthesis of vitamin D [8].
The optimal level of 25- OH vitamin D is still unknown. In 2010, the Institute of Medicine recommended a normal value of >20 ng/mL with values less than 20 ng/mL being considered vitamin D deficiency [7]. In 2011, the Endocrine Society recommended vitamin D levels over 30 ng/mL and in order to guarantee sufficiency, it suggested levels between 40 to 60 ng/mL for both children and adults [8]. As this patient presented a decrease in PVC number after further increasing the 25- OH vitamin D levels from 28.4 to 40.8 ng/mL, authors believe that the adequate level of 25 OH vitamin D should be higher than 30 ng/mL [9].
Few clinical trial studies on vitamin D deficiency and cardiovascular events are available in children [10]. Dong Y et al., in a randomised controlled trial showed that vitamin D administration slows down the progression of aortic stiffness and reduces adipose tissue [11]. Atabek ME et al., also demonstrated that there is a strong correlation between low levels of vitamin D and carotid intima media thickness as well as metabolic syndrome [12]. In addition, improvement of glucose homeostasis was observed after vitamin D supplementation [13]. Furthermore, children with vitamin D deficiency shows insulin resistance which correlates with the degree of deficiency. Vitamin D was demonstrated to inhibit parathyroid hormone production in children, through a feedback mechanism. Thus, the chronic vitamin D deficiency leads to a decrease in intestinal calcium absorption and implicitly to the mobilisation of calcium from the bones. This increases the Parathyroid Hormone (PTH) production and PTH leads to cardiac arrhythmias [14,15].
However, there are 2 reports that are similar to the present case: a 31-year-old male patient with RVOT PVCs due to intermittent fasting 18 hours/day. Holter ECG showed frequent PVCs >17300, which disappeared after the end of fasting period. Even though electrolytes were normal in this case, the authors do not mention the level of vitamin D. This could be one of the causes of PVCs, especially since the supply during intermittent fasting was done during the night [16]. The second case was of a 54-year-old athletic patient, in whom cardiac rehabilitation associated with vitamin D supplementation led to a significant decrease in PVC number [17].
The prognosis for this patient was good because there was no structural heart disease. Given the significant reduction in the number of PVCs only through vitamin D supplementation, the direct cause could be corrected.
Conclusion(s)
Present report demonstrates that PVCs induced by vitamin D deficiency can be corrected using vitamin D supplementation, without the need of catheter ablation or antiarrhythmic drugs. Vitamin D deficiency could be one of the most important causes of PVCs, which should be further investigated on prospective studies, because it is a common deficiency in European countries and treatment is surprisingly simple.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 28, 2020
Manual Googling: Apr 02, 2021
iThenticate Software: Apr 28, 2021 (11%)
[1]. Olivero JJ, Cardiac consequences of electrolyte imbalanceMethodist Debakey Cardiovasc J 2016 12(2):125-26.10.14797/mdcj-12-2-12527486499 [Google Scholar] [CrossRef] [PubMed]
[2]. Ng GA, Treating patients with ventricular ectopic beatsHeart 2006 92(11):1707-12.10.1136/hrt.2005.06784317041126 [Google Scholar] [CrossRef] [PubMed]
[3]. Cecchi E, Grossi F, Rossi M, Giglioli C, De Feo ML, Severe hypocalcemia and life-threatening ventricular arrhytmias: Case report and proposal of a diagnostic and therapeutic algorithmClin Cases Miner Bone Metab 2015 12(3):265-68.10.11138/ccmbm/2015.12.3.26526811710 [Google Scholar] [CrossRef] [PubMed]
[4]. Wang JS, Shen YG, Yin RP, Thapa S, Peng YP, Ji KT, The safety of catheter ablation for premature ventricular contractions in patients without structural heart diseaseBMC Cardiovascular Disorders 2018 18:177-82.10.1186/s12872-018-0913-230170545 [Google Scholar] [CrossRef] [PubMed]
[5]. Zhong L, Lee YH, Huang XM, Asirvatham SJ, Shen WK, Friedman PA, Relative efficacy of catheter ablation vs antiarrhythmic drugs in treating premature ventricular contractions: A single-center retrospective studyHeart Rhythm 2014 11(2):187-93.10.1016/j.hrthm.2013.10.03324157533 [Google Scholar] [CrossRef] [PubMed]
[6]. Fichtner S, Senges J, Hochadel M, Tilz R, Willems S, Eckardt L, Safety and efficacy in ablation of premature ventricular contraction: Data from the German ablation registryClin Res Cardiol 2017 106(1):49-57.10.1007/s00392-016-1022-927484499 [Google Scholar] [CrossRef] [PubMed]
[7]. Ling Z, Liu Z, Su L, Zipunnikov V, Wu J, Du H, Radiofrequency ablation versus antiarrhythmic medication for treatment of ventricular premature beats from the right ventricular outflow tract: Prospective randomized studyCirc Arrhythm Electrophysiol 2014 7(2):237-43.10.1161/CIRCEP.113.00080524523413 [Google Scholar] [CrossRef] [PubMed]
[8]. Kennel K, Drake M, Hurley D, Vitamin D deficiency in adults: When to test and how to treatMayo Clin Proc 2010 85(8):752-58.10.4065/mcp.2010.013820675513 [Google Scholar] [CrossRef] [PubMed]
[9]. Institute of Medicine Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride 1999 Washington, DCNational Academy Press:71-145. [Google Scholar]
[10]. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society Clinical Practice GuidelineJ Clin Endocrinol Metab 2011 96(7):1911-30.10.1210/jc.2011-038521646368 [Google Scholar] [CrossRef] [PubMed]
[11]. Dong Y, Stallmann-Jorgensen IS, Pollock NK, Harris RA, Keeton D, Huang Y, A 16-week randomized clinical trial of 2000 international units daily vitamin D3 supplementation in black youth: 25-hydroxyvitamin D, adiposity, and arterial stiffnessJ Clin Endocrinol Metab 2010 95(10):4584-91.10.1210/jc.2010-060620660028 [Google Scholar] [CrossRef] [PubMed]
[12]. Atabek ME, Eklioglu BS, Akyürek N, Alp H, Association between vitamin D level and cardiovascular risk in obese children and adolescentsJ Pediatr Endocrinol Metab 2014 27:661-66.10.1515/jpem-2013-037924756047 [Google Scholar] [CrossRef] [PubMed]
[13]. Ashraf AP, Alvarez JA, Gower BA, Saenz KH, McCormick KL, Associations of serum 25-hydroxyvitamin D and components of the metabolic syndrome in obese adolescent femalesObesity 2011 19(11):2214-21.10.1038/oby.2011.11021546933 [Google Scholar] [CrossRef] [PubMed]
[14]. Andersson P, Rydberg E, Willenheimer R, Primary hyperparathyroidism and heart disease-a reviewEur Heart J 2004 25(20):1776-87.10.1016/j.ehj.2004.07.01015474692 [Google Scholar] [CrossRef] [PubMed]
[15]. Foley RN, Parfrey PS, Harnett JD, Kent GM, Martin CJ, Murray DC, Clinical and echocardiographic disease in patients starting end-stage renal disease therapyKidney Int 1995 47(1):186-92.10.1038/ki.1995.227731145 [Google Scholar] [CrossRef] [PubMed]
[16]. Kahraman S, Dogan A, Ventricular arrhythmia linked to long intermittent fastingJournal of Electrocardiology 2019 58:125-27.10.1016/j.jelectrocard.2019.10.00831838312 [Google Scholar] [CrossRef] [PubMed]
[17]. Cismaru G, Gurzau D, Fringu F, Martis A, Caloian B, Comsa H, Vitmamin D supplementation with cardiac rehabilitation reduces the number of RVOT premature ventricular contractionsBalneo Research Journal 2020 11:566-68.10.12680/balneo.2020.406 [Google Scholar] [CrossRef]