The World Health Organisation (WHO) and International Association for the study of pain have recognised pain relief as a basic human right. Postoperative pain is the most common fear of each patient undergoing any kind of surgery; whereas its management is a challenge for anaesthesiologist. Inadequate pain control causes physical discomfort and mental stress to patient and may result in increased morbidity and mortality [1,2].
Postoperation pain increases haemodynamic instability, altered breathing pattern, suppress cough reflexes, delaying bowel function, and prolong recovery period. Postoperative pain control is an important factor for smooth postoperative recovery.
Dexmedetomidine is alpha-2 adrenoceptor agonist which does not produce significant respiratory depression. It’s effects of sedation, anxiolysis and analgesia is dose dependent, and it act through spinal and supra-spinal sites [3,4]. Dexmedetomidine has synergistic effect with other anaesthesia drugs. It stimulates central α-2 and imidazoline receptors which causes perioperative sympatholysis thus decreases blood pressure [5,6]. The most frequently observed adverse effects include hypotension, bradycardia, dry mouth and nausea.
Fentanyl is a phenylpiperidine-derivative strong synthetic opioid agonist that is structurally related to meperidine. Biochemically, it is referred to as a Mu-selective opioid agonist. However, it has the capabilities to activate other opioid system receptors such as the delta, and potentially the kappa-receptors. Consequently, the activation of these receptors, particularly the Mu-receptors produces analgesia [7]. Although opioids are highly effective in pain control, its prolong and high dose use can lead to extended hospital stay due to undesirable adverse effects such as respiratory depression, nausea, vomiting, pruritus, and urinary retention [8].
This study was planned to compare role of dexmedetomidine and fentanyl in postoperative pain control. Although there are many studies who compared these two drugs as an adjuvant in regional anaesthesia but there was no study which compared these two drugs as sole intravenous agent to know their exact effect on postoperative pain in absence of compounding factor from other drugs. Primary objective of this study was to compare effect of these drugs on postoperative VAS score and analgesia requirement. Secondary objectives was to study effects of these drugs on perioperative haemodynamics.
Materials and Methods
This randomised trial was conducted over a period of one year between January 2019 to January 2020, in various operation theatres of King George’s Medical University, Lucknow, Uttar Pradesh, India. An approval was obtained from the Ethical Committee of the University (Ref.Code: 93rd ECM II B-Thesis/P32).
Inclusion criteria: Patients between 25-65 years who belonged to American Society of Anaesthesiology (ASA) grade I to III of either sex, gave informed consent and undergone abdominal surgery during study time period were included in study.
Exclusion criteria: Patients with severe infection, severe anaemia (Haematocrit <30%), brain stroke, intracranial bleeding, uncontrolled hypertension, haemodynamically, instability, dementia and with expected duration of surgery more than four hours were excluded from study.
Sample size calculation: The sample size was calculated by using the formula given below and based on a previous study [8]:
n=(Zα+Zβ)2(S12+S22)/d2
Where, Zα=1.96 at 5% significant level; Zβ=0.842 at 20% of MAP, S1=13.6 the maximum SD, in the 1st group; S2=17.8 maximum SD of MAP in 2nd group; d=Mean difference of two comparative group; After keeping the values in place, n came out to be 30 for each group.
Study Procedure
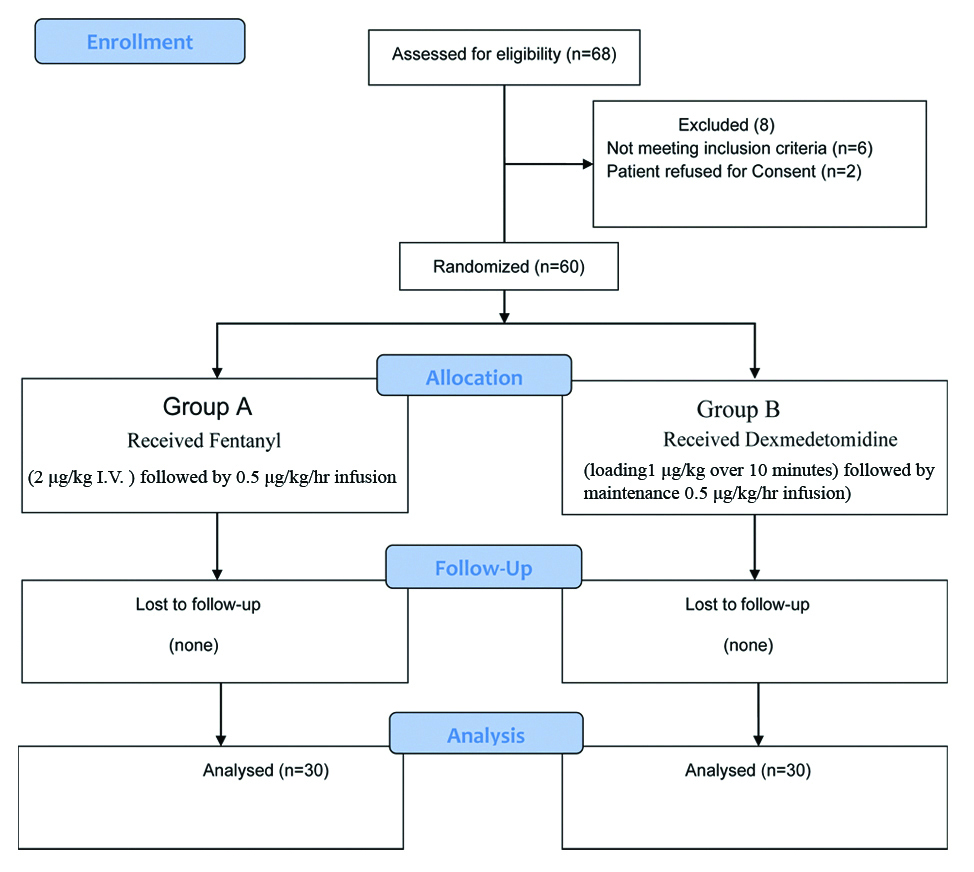
After preoperative evaluation, patients were taken to operation theatre, then standard monitors were attached (pulse oximeter, non-invasive blood pressure, electrocardiogram) and an intravenous line was secured. Patients were randomly allocated into one of the two groups by using computer generated random number table and closed envelope method. Group A (n=30) received fentanyl loading dose as slow I.V bolus 2 μg/kg followed by continuous infusion at a rate of 0.5 μg/kg/hr up to four hours during surgery, and group B (n=30) received dexmedetomidine loading 1 μg/kg over 10 minutes followed by continuous infusion at a rate of 0.5 μg/kg/hr during surgery up to four hours. All the patients were induced by I.V administration of 2 mg/kg propofol and intubation was facilitated by I.V administration of 0.1 mg/kg vecuronium and general anaesthesia maintained by inhalation of 1% isoflurane in oxygen and nitrous oxide in ration of 1:2. Normocapnia (EtCO2 between 35 and 40 mm Hg) was maintained by controlled ventilation.
Haemodynamic parameters (HR and MAP) were recorded after the start of study drug infusion, before and after intubation, then every 15 minutes till one hour and every 30 minutes till end of surgery. After completion of surgical procedure, extubation was done after full reversal (using glycopyrrolate 0.01 mg/kg with neostigmine 0.04 mg/kg). After appropriate neuromuscular recovery, patients were transferred to the Postanaesthesia Care Unit (PACU). In PACU, infusion of both the study drugs were continued and haemodynamic parameter (HR and MAP) were recorded hourly till eight hours. Postoperative analgesia was assessed hourly till eight hours by Visual Analogue Scale (VAS). This scale ranges from 0 to 10, where 0 represents no pain and 10 represents worst pain. Postoperatively intravenous paracetamol (20 mg/kg) was given as primary rescue analgesia when VAS score >4 and Tramadol (2 mg/kg) was given as secondary rescue analgesia when pain was not relieved by paracetamol and VAS score was above four. The total amount of rescue analgesia (both primary and secondary) required were recorded.
Statistical Analysis
The statistical analysis was done using SPSS (originally, Statistical Package for the Social Sciences, later modified to Statistical Product and Service Solutions) Version 21.0 Software. Results on continuous measurements were shown as Mean±SD and results on categorical measurements were shown in frequency (n) and percentages (%). Analysis of variance was used to find the significant difference of parameters between two groups. Chi-square test was used to find the significance of study parameters on categorical scale between two groups. The p-value <0.05 was considered significant.
Results
Sixty patients belonging to ASA Grade I, II and III were recruited in study who were posted for abdominal surgeries under general anaesthesia. Patients were randomly divided into two groups of 30 each [Table/Fig-1]. The mean age, weight and height of the patients were comparable [Table/Fig-2].
| Variable | Group A | Group B | t-value | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Age (Year) | 43.47±5.64 | 45.43±6.43 | -1.26 | 0.213 |
| Weight (Kg) | 59.63±7.20 | 60.77±7.23 | -0.61 | 0.545 |
| Height (cm) | 163.80±4.82 | 162.13±5.95 | 1.19 | 0.238 |
Students t-test, p-value <0.05 was significant
On comparing the VAS score between the groups, it was found to be significantly less in group B as compared to group A, just after extubation (p<0.001), one hour (p<0.001), two hour (p=0.010), four hour (p=0.006), seven hour (p=0.047) and eight hour (p=0.045) [Table/Fig-3].
Intergroup comparison of VAS.
| VAS | Group A | Group B | z-value | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| After extubation | 4.80±1.54 | 3.00±1.39 | -4.20 | <0.001 |
| 1 h | 4.93±1.55 | 3.07±1.01 | -4.46 | <0.001 |
| 2 h | 4.40±1.19 | 3.67±1.06 | -2.59 | 0.010 |
| 3 h | 4.00±1.31 | 3.67±1.65 | -1.16 | 0.244 |
| 4 h | 3.50±1.07 | 2.73±1.31 | -2.77 | 0.006 |
| 5 h | 2.87±1.11 | 2.57±1.30 | -0.83 | 0.409 |
| 6 h | 2.37±0.67 | 2.10±0.84 | -1.57 | 0.115 |
| 7 h | 2.07±0.25 | 1.93±0.25 | -1.98 | 0.047 |
| 8 h | 2.10±0.31 | 1.97±0.18 | -2.00 | 0.045 |
h: Hour
The proportion of patients provided with primary rescue analgesia was significantly more in group A than group B (p=0.023). The proportion of patients provided with secondary rescue analgesia was significantly more in group A than group B (p<0.001) [Table/Fig-4].
Intergroup comparison of rescue analgesia given.
| Rescue analgesia | Group A | Group B | Chi-square test | p-value |
|---|
| n (%) | n (%) |
|---|
| Primary rescue analgesia given | No | 1 (3.3%) | 9 (30.1%) | 5.19 | 0.023 |
| Yes | 29 (96.7%) | 21 (69.9%) |
| Secondary rescue analgesia given | No | 9 (30.0%) | 25 (83.3%) | 17.38 | <0.001 |
| Yes | 21 (70.0%) | 5 (16.7%) |
| Total | 30 (100.0%) | 30 (100.0%) |
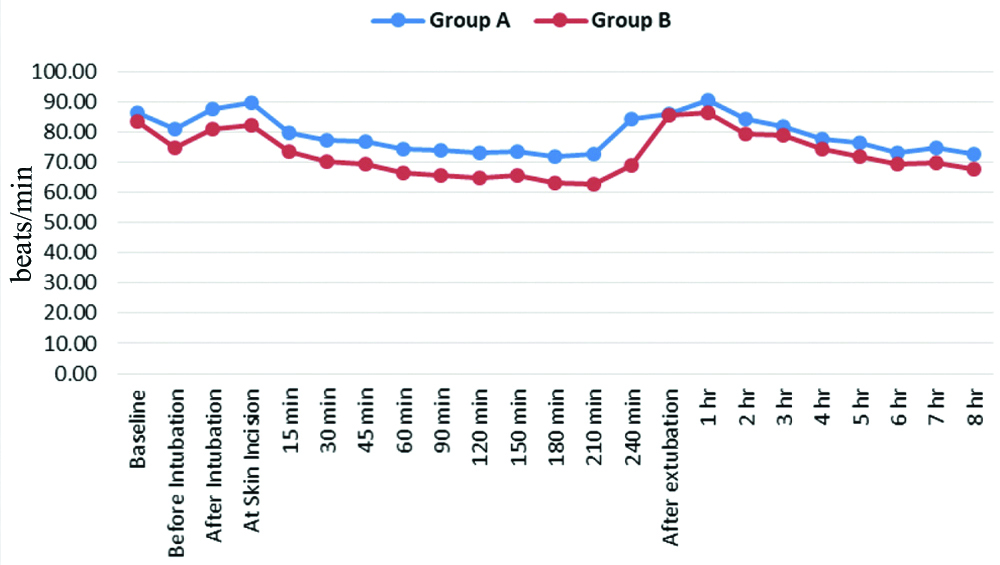
On comparing HR between the groups, it was found significantly less in group B, before intubation (p=0.002), after intubation (p=0.002) and from skin incision to 240 minutes (p<0.05). It was also less in group B from 2nd hour after extubation to 8 hour (p<0.05) [Table/Fig-5].
Intergroup comparison of Heart Rates (HR).
On comparing the MAP between the groups, it was significantly less in group B as compared to group A, before intubation to 15 minutes (p<0.001), 45 minutes to 120 minutes (p<0.001) and then just after extubation (p=0.022), three hour after extubation (p=0.084), five hour (p=0.112) and seven hour (p=0.039) [Table/Fig-6].
Intergroup comparison of Mean Arterial Pressure.
| MAP (mm of Hg) | Group A | Group B | t-value | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 99.70±4.35 | 97.87±4.29 | 1.64 | 0.106 |
| Before intubation | 89.23±5.49 | 84.57±4.58 | 3.57 | 0.001 |
| After intubation | 94.77±4.45 | 89.37±3.33 | 5.33 | <0.001 |
| At skin incision | 91.57±7.19 | 84.97±6.79 | 3.65 | 0.001 |
| 15 min | 87.27±7.55 | 80.80±7.07 | 3.42 | 0.001 |
| 45 min | 88.43±4.04 | 84.33±3.34 | 4.29 | <0.001 |
| 60 min | 87.40±4.33 | 82.87±3.44 | 4.49 | <0.001 |
| 120 min | 83.97±4.76 | 78.33±4.36 | 4.74 | <0.001 |
| 180 min | 87.52±7.75 | 84.09±6.20 | 1.66 | 0.104 |
| 240 min | 86.38±4.93 | 76.00±0.00 | 2.85 | 0.022 |
| After extubation | 97.67±6.23 | 93.23±8.23 | 2.35 | 0.022 |
| 1 h | 99.47±7.30 | 97.53±5.36 | 1.17 | 0.247 |
| 3 h | 94.80±6.71 | 91.67±7.11 | 1.76 | 0.084 |
| 5 h | 89.57±6.93 | 86.97±5.47 | 1.61 | 0.112 |
| 7 h | 87.90±5.48 | 85.10±4.74 | 2.12 | 0.039 |
*All bold p-values to be significant
Discussion
Pain has always been one of the most troublesome symptoms associated with any surgery and its management is still a challenge for anaesthesiologists. Multimodal analgesic techniques have been shown to decrease the requirement of opioids intraoperatively and postoperatively. However, none of those drugs were effective and sufficient as the sole analgesic and thus the need for evaluating newer drugs as replacement of opioids in the intraoperative period is still going on. Alpha-2 agonists such as clonidine and dexmedetomidine have shown promising results in this context [8].
This study was done to compare intravenous dexmedetomidine and fentanyl for postoperative pain relief provided by them, in terms of VAS score, intraoperative and postoperative haemodynamic stability assessed by HR, MAP, and amount of rescue analgesia required. Studies so far conducted were between intrathecal fentanyl and dexmedetomidine or epidural fentanyl and dexmedetomidine.
The rationale for choosing concentration of fentanyl (2 μg/kg) in bolus with continuous infusion of the fentanyl (0.5 μg/kg/hr) is supported by study of Goyal S et al., where they compared intravenous dexmedetomidine and fentanyl in breast cancer surgery with same dose of fentanyl [9].
Dexmedetomidine (1 μg/kg) as bolus over 10 minutes with continuous infusion of the dexmedetomidine (0.5 μg/kg/hr) supported by study of Hamid MH where they showed that same concentration of dexmedetomidine provide better control of haemodynamic stability and lesser requirement of rescue analgesia [8]. In another study done by Goyal S et al., where they used dexmedetomidine 1 μg/kg as loading dose with maintenance dose of 0.25 μg/kg/hr [9]. They found no statistically significant difference (p=0.739) of total rescue analgesia requirement in both fentanyl and dexmedetomidine group, which may be due to underdose of dexmedetomidine in infusion. Therefore, present study used dexmedetomidine (0.5 μg/kg/hr) infusion, as was used by Hamid MH [8].
In both the groups, a decline in HR from baseline was observed during intraoperative and postoperative period, while decline was more in group B than group A. In present study, it was found that HR before intubation was significantly low (p=0.002) in group B (74.90±4.71) as compared to group A (80.83±8.63). The HR continued to be significantly low in group B (81.23±5.50) than group A (87.63±9.02) after intubation (p=0.002) and also, throughout intraoperative period (p<0.05). After extubation and 2nd hour, 5th hour, 6th hour,7th hour and 8th hour postoperatively, HR was significantly less (p<0.05) in group B as compared to group A. In a study conducted by Goyal S et al., they also found that HR was lower in dexmedetomidine group as compared to fentanyl group intraoperatively, before and after extubation with a significant p-value [9].
Above results were comparable with the study conducted by Aksu R et al., where they found that in dexmedetomidine group, HR was not significantly increased after extubation; however, in the fentanyl group, HR was significantly increased compared with the pre-extubation values (p=0.007) [10]. HR was significantly higher in the fentanyl group compared with the dexmedetomidine group at pre-extubation values. Results of this study was also supported by research conducted by Hamid MH, Feld JM et al., Shalaby M et al., where they found that HR was significantly lower in dexmedetomidine group as compared to fentanyl group [8,11,12].
There was no significant (p=0.106) difference in baseline MAP in group A and B. In both groups, MAP was lower than baseline during the intraoperative and postoperative observation period. During intraoperative period, MAP in group B was found significantly (p<0.05) lower as compared to group A at all the points of observation except 30th, 180th and 210th minute of surgery. Postoperatively, MAP was found significantly lower in group B as compared to group A after extubation, 2nd hour (p=0.022), 6th hour (p=0.047), 7th hour (p=0.039).
Comparative results were also found in study conducted by Hamid MH, where they reported significantly lower MAP in dexmedetomidine group as compared to fentanyl group at all the point of observation intraoperatively and postoperatively [8].
Similar results were seen in study conducted by Goyal S et al., where they observed that MAP was significantly lower in dexmedetomidine group compared to fentanyl group [9]. Similar observation was also seen in study conducted by Kalla RS et al., where MAP was significantly decreased after administration of the dexmedetomidine after endotracheal intubation and it remained significantly lower than the baseline values [13]. In fentanyl group, the MAP significantly increased after endotracheal intubation as compared to the baseline values.
In present study, VAS score was lower in group B at all points of time, however the difference was significant in comparison to group A after extubation (p<0.001), 1st hour (p<0.001), 2nd hour (p=0.010), 4th hour (p=0.006), 7th hour (p=0.047) and 8th hour (p=0.045) postoperative period.
Baseline VAS score in group A was 4.80 after extubation, which was increased to 4.93 at one hour which gradually kept on declining up to eight hours. First line rescue analgesia was given whenever VAS score >4. We observed that VAS score was >4, after extubation, one hour, two hour, three hour postoperatively. VAS score remained between (2.87±1.11) from 5th hour to (2.10±0.31) at 8th hour except at seven hours (2.07±0.31).
Baseline VAS score in group B was 3.0±1.39 after extubation, which increased to 3.07±1.01 at one hour, and further increased at two hours and three hours. Then VAS score started declining at four hours and continued decreasing to 1.97±0.18 till eight hours, and remained between 2.73 to 1.97 during four hours to eight hours of postoperative period. Decline in VAS after 4th hour is probably due to rescue analgesia given to patients in group B. Most of the patients needed rescue analgesia between 3rd and fourth hour.
This study was in line with some previous studies. Study conducted by Hamid MH, that compared I.V dexmedetomidine with fentanyl in shoulder surgery, found significantly less VAS score in dexmedetomidine group after extubation, at 30 minutes and one hour than fentanyl group [8]. Similarly pain score was found less in study done by Feld JM et al., in dexmedetomidine group [11].
In a study, conducted by Safari F et al., they found that Dexmedetomidine added to bupivacaine in spinal anaesthesia is more effective with less postoperative pain scale than fentanyl [14]. In another study, conducted by Govindswamy S and Curpod P, they found that dexmedetomidine provide significantly longer duration of analgesia (p<0.001) than fentanyl when added intrathecally [15].
In this study, requirement of first rescue analgesia was significantly earlier in group A as compared to group B (p=0.04) after extubation. Total amount of rescue analgesia given after one hour of extubation was significantly higher in group A compared to group B (p<0.001). On the contrary, the number of patients required rescue analgesia in 2nd and 3rd hours after extubation was more in group-B.
In this study, it was found that the number of patients who required primary rescue analgesia was significantly more in group A (36.7%) than group B (13.3%) after extubation (p=0.037) and after one hour of extubation (p<0.001). While, patients who needed primary rescue analgesia at 3rd hour of postoperative period was significantly (p=0.001) more in group B (12%) as compared to group A (0.0%). Significant early requirement of primary rescue analgesia was seen in group A as compared to group B. Patients who required maximum primary rescue analgesia in group A was seen at one hour of extubation (46.7%) as compared to group B which required analgesia during three hours (33.3%). The number of patients provided with primary rescue analgesia was significantly more in group A than group B (p=0.023).
The number of patients who were provided with secondary rescue analgesia was significantly more in group A than group B (p<0.001). The mean amount of total paracetamol and tramadol required in group B was relatively less than the group A but not statistically significant. In a previous study, done by Goyal S et al., they found that time for first rescue analgesic dosage required was 31.63 minutes in dexmedetomidine group and 26.47 minutes in fentanyl group which was comparable in both the groups and total requirement of rescue analgesia was more in fentanyl group than dexmedetomidine group [9].
Similarly, another study done by Feld JM et al., found that requirement of rescue analgesia (morphine) was decreased in dexmedetomidine group as compared to fentanyl group in patient undergoing gastric bypass surgery in bariatric surgery [11]. Similar results were found by Soliman R and Eltaweel M, where quality of analgesia was better along with lower requirement for opioids in dexmedetomidine group than fentanyl group [16].
Limitation(s)
Small sample size was the limitation in the present study.
Conclusion(s)
From the study, it can be concluded that I.V infusion of dexmedetomidine provide better Postoperative analgesia and peri-operative haemodynamic stability as compared to fentanyl group. The mean VAS score was significantly less in dexmedetomidine group during postoperative period, as compared to fentanyl group. Thus, patients required significantly less and delayed primary and secondary rescue analgesia in dexmedetomidine group, after extubation and the requirement was more and earlier in fentanyl group. Haemodynamic parameters (HR and MAP) were more stable in dexmedetomidine group as compared to fentanyl group. Hence, it can be said that dexmedetomidine provides better haemodynamic stability than fentanyl.
Students t-test, p-value <0.05 was significant
h: Hour
*All bold p-values to be significant