Introduction
The deformity and imbalance in an osteoarthritic knee undergoing Total Knee Arthroplasty (TKA) are the result of a combination of bony and soft tissue changes locally. Proper and ideal balancing of ligaments is considered essential to the success of a TKA. There are numerous techniques to achieve soft tissue balance in varus knee. More recently, Medial Tibial Reduction Osteotomy (MTRO) has been described as an adjuvant to soft tissue release. Limited data exists on the outcomes of patients requiring a MTRO. There are not many Indian studies available regarding the radiographic and clinical outcomes of medial reduction osteotomy in severe varus deformity in TKA.
Aim
To find out the radiological and functional outcome of MTRO for severe varus deformity in patients undergoing TKA.
Materials and Methods
This study was prospective Cohort study conducted at the Department of Orthopaedics, Rajagiri Hospital, Chunangamveli, Aluva, Kerala from December 2018 to November 2019. Twenty patients 15 females and 5 males (30 knees), in the age group 55-80 years with osteoarthritis of knee with severe varus deformity, were enrolled in the study. Preoperative and postoperative standing leg Antero-posterior radiographs were taken for all patients and hip-knee-ankle angle was measured and amount of deformity correction was calculated. Postoperatively, radiographs were taken on the 5th day and 3rd month. Knee society scores were also recorded preoperatively and on the 5th postoperative day, postoperative visits on 6 weeks, 3 months and clinical outcome was assessed. The statistical analysis was performed by Statistical Package for Social Sciences (SPSS) version 25.0 using Analysis of Variance (ANOVA) and Wilcoxon Signed Rank test.
Results
The median knee score improved from 47±9 to 93±3 postoperatively. Similarly, median function score improved from 50±5 to 80±0. The improvement in function score and knee score were statistically significant (p-value 0.001). The correction of varus between preoperative, postoperative (p-value 0.001) day 5 and 3 months postoperatively was statistically significant. No patient required a release of the superficial Medial Collateral Ligament (MCL). The MTRO was associated with statistically significantly improved Knee Society scores and varus deformity correction.
Conclusion
In patients with fixed varus deformity of the knee, the MTRO is found to be safe and adequate to achieve coronal alignment.
Knee society score, Ligament balancing, Medial tibial osteophytes, Medial collateral ligament
Introduction
A fixed varus deformity is the most common deformity seen in patients with advanced osteoarthritis of the knee with numerous medial tibial osteophytes and adaptive changes in the medial proximal tibia. These cause tenting effects on medial soft tissue structures, including the MCL. Patient’s daily activities may be substantially affected by pain, and they have functional limitations because of the severe varus knee deformity [1].
The TKA is technically challenging with severe varus knee deformity when it is combined with contracture of medial soft tissue and laxity of lateral soft tissue. The more severe is the deformity, the surgical time is more and there is an increased difficulty in achieving soft tissue balance and optimal bony alignment. An optimal ligament balancing and bony alignment are the utmost factors that impact the long-term success [2,3].
There are numerous techniques to achieve soft tissue balance in varus knee like medial soft tissue releases that can be done as a periosteal sleeve off the tibia, discrete release of the superficial MCL and pes anserine tendons, pie-crusting of the superficial MCL and femoral medial epicondylar osteotomy. Each method has its own advantages and disadvantages. Extensive sub-periosteal stripping of the proximal medial tibial soft tissue sleeve may result in more bleeding [4,5]. Additionally, aggressive medial soft tissue release can lead to attenuation of the MCL with a risk of subsequent instability [6,7]. In MCL pie-crusting failure occurs within the ligament itself [8]. With femoral medial epicondylar osteotomy, the knee may become more unstable in flexion and a higher constraint implant may be necessary [9].
More recently, MTRO with lateralising the tibial tray and resection of the uncapped medial tibial bone has been described. Sequential steps include removal of osteophytes, deep MCL and semi-membranosus, and postero-medial capsular release. If an asymmetric extension gap remains after these releases, an MTRO is done. The superficial MCL is not released. The proximal medial tibia is resected along the longitudinal axis of the tibia. In some cases, this is associated with downsizing of the tibial base plate. By resecting the medial tibial bone, the intact medial soft tissue sleeve is decompressed. MTRO typically lessens the amount of medial soft tissue releasing required to correct the varus deformity and prevent over-release of medial structures [10]. The MTRO relatively lengthens the medial soft tissue sleeve once you remove the prominent proximal tibial flare which tents the medial structures. This lengthening helps to correct the varus deformities. Sometimes even removal of medial osteophytes results in complete correction of varus deformity due to relaxation of the tight medial soft tissue structures. In other instances, an additional MTRO may be required to achieve complete correction of the deformity and balancing [1]. Reduction osteotomy is a soft tissue sparing procedure for soft tissue balancing. If this scientific approach is properly utilised, the medial soft tissue release can be effectively avoided.
This study describes balancing of a fixed varus knee deformity by incorporating a series of medial soft tissue releases and a MTRO to achieve coronal mechanical alignment. On an average, one-degree correction can be obtained by resecting 2 mm of non osteophytic bone. An extensive bone resection can cause tibial component loosening and difficulty in revision surgery. Complications like osteolysis, loosening, or component subsidence usually occurs in long-term [11]. The sclerotic bone under the medial tibial articular surface from abnormal weight bearing due to the varus misalignment and the arthritic process, more often extends toward the midline so the risk of subsidence from lateralising the medial tibial tray is minimised. The medial tibial bone resorption or osteolysis can be due to thermal necrosis from the saw blade used for trimming the sclerotic medial tibia while doing a MTRO. In order to reduce the potential for thermal necrosis, MTRO may be done with a rongeur or add irrigation if the sclerotic medial tibial is being removed using a saw [10]. By performing a reduction osteotomy in knees with correctible varus deformity to <5° or more may lead to excessive medial slackening of soft tissue and over-correction.
In this study, radiological and clinical outcomes in patients with severe varus deformity undergoing MTRO were assessed. Hip Knee Ankle radiograph was used to evaluate limb alignment preoperatively and postoperatively. This radiograph is more reliable and reproducible for determining the knee alignment in the coronal plane after TKA [12-14]. An angle within 3° from the mechanical axis is supposed to reduce the risk of abnormal wear, premature loosening, and early implant failure [15-17]. Knee Society Score is used to measure the clinical outcome of MTRO, which has mainly two parts- knee score that rates only the knee joint and a functional score that rates the patient’s ability to walk and climb stairs [18].
Though there are various methods of achieving soft tissue balance including variety of ligament releases, the more recently described indirect method of soft tissue balancing is the MTRO [19]. It results in a reduction in surgical time and lessens the amount of medial soft tissue release. This study aimed to analyse the functional and radiological outcome of MTRO in severe varus TKA.
Materials and Methods
This prospective cohort study was conducted at the Department of Orthopedics, Rajagiri Hospital, Chunangamvely, Kerala, India from December 2018 to November 2019. The study population consisted patients with severe varus knee. Institutional Ethics Committee approval was obtained before starting the study (Ref No: RAJH/SRC/DNB/0011).
Inclusion criteria: Patients in the age group 55-80 years with severe varus deformity (>15), undergoing TKA during the study time period were included in the study.
Exclusion criteria: Patients with extra-articular deformity were excluded.
Sample size calculation: The study done by Ahn JH et al., was referred to and a sample size of 30 was arrived [20]. Assuming that 95% confidence interval and 90% power, based on the mean and SD values of pre-test 10.1±4.2 and post-test 0.6±1.6, the required minimum sample size is 10, using the formula:
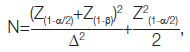
Where, Z(1-α/2) at α error of 5% is 1.96 and Z(1-β) at β error of 90% is 1.28
Where,
μ1: Pre-test mean
μ2: Post-test mean
σ1: Standard deviation in the pre-test
σ2: Standard deviation in the post-test
Δ: Effect Size
σ: Significance level
1-β: Power
Study Procedure
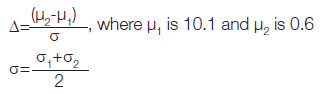
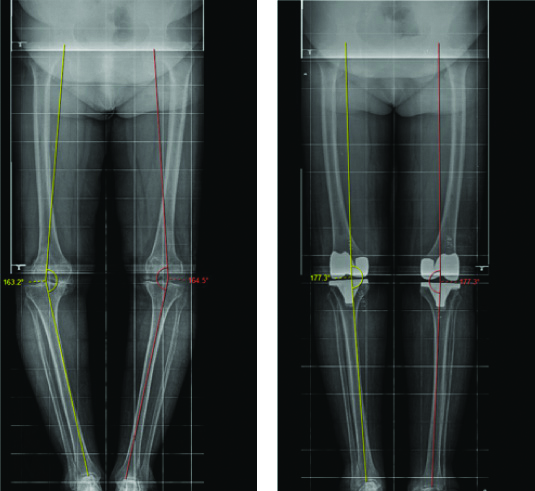
The MTRO was done in a sequential order as shown in [Table/Fig-1,2] [10]. Preoperative and postoperative standing long leg Anteroposterior (AP) radiographs were taken for all patients and Hip-Knee-Ankle angle was measured and amount of deformity correction was calculated as shown in [Table/Fig-3,4]. Postoperatively, radiographs were taken on the 5th day and 3rd month. Knee society scores were also recorded preoperatively and on the 5th postoperative day, postoperative visits in 6 weeks and 3 months. The mechanical axis of the femur is a line drawn from the centre of the femoral head to the centre of the knee [20]. The mechanical axis of the tibia is a line from the centre of the proximal tibial plateau to the centre of the talus. Both lines were drawn on long leg weight-bearing radiographs and Hip-Knee-Ankle angle was measured.
The uncapped medial tibial bone is well defined and marked with a skin marker.
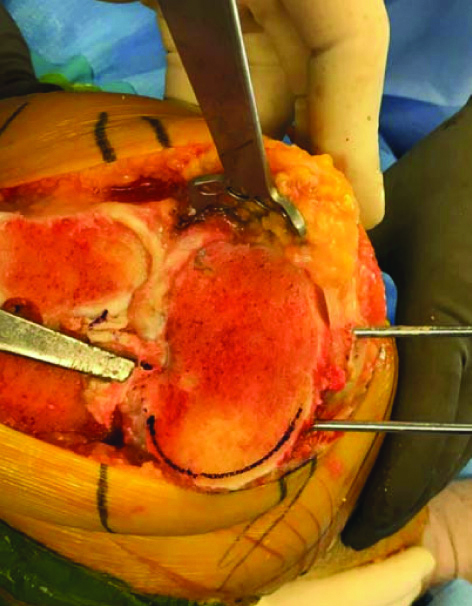
MTRO: Medial Tibial Reduction Osteotomy was done with a rounger instead of saw to avoid thermal necrosis.
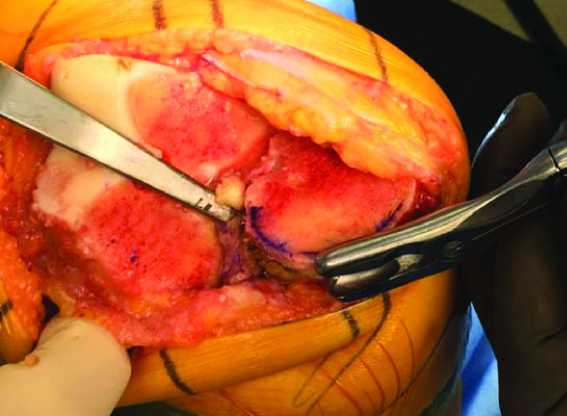
Preoperative and Postoperative X-ray measurement of Hip-Knee-Ankle angle in a unilateral TKA.
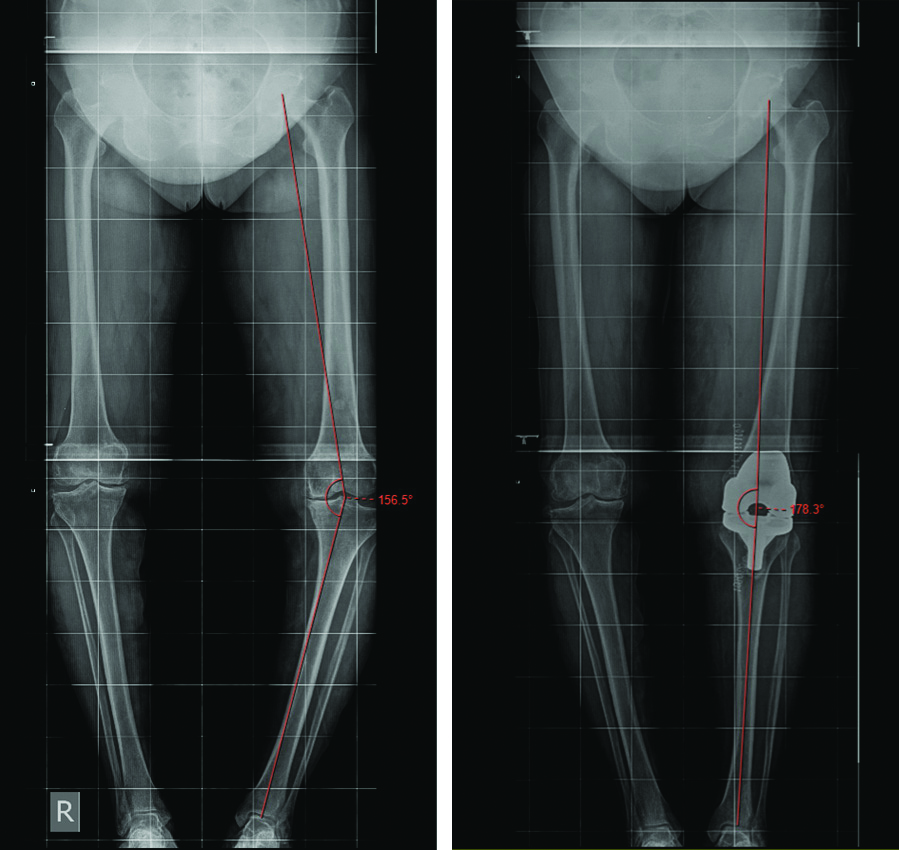
Preoperative and Postoperative X-ray measurement of Hip-Knee-Ankle angle in a bilateral TKA.
Knee Society Score
The original Knee society score has a “Knee Score” section (7 items) and a “Functional Score” section (3 items). Each part is scored from 0 to 100 with lower scores indicative of bad knee conditions, and higher scores mean good knee conditions. Knee society score is graded as- score of 80-100 as excellent, 70-79 as good, 60-69 as fair and score below 60 as poor. The preoperative knee society score was noted and later it was compared and analysed with postoperative day 5, 6 weeks and three month score as per the knee society score proforma [21].
Statistical Analysis
The statistical analysis was performed by SPSS 25. Qualitative variables were expressed as frequency and percentages and quantitative variables as mean and standard deviation. Association between various factors was assessed using Friedman’s ANOVA and Wilcoxon Signed Ranks test for categorical variable, ANOVA for quantitative variables. The p-value of <0.05 was considered to be statistically significant.
To determine the period of significant difference in function score and knee score post-hoc analysis was done using Wilcoxon Signed Ranks Test. Increase in Type 1 error (α error) was corrected using Bonferroni correction, α error fixed at 0.016.
Results
The study enrolled 20 patients (30 knees) with osteoarthritis of knee and having severe varus deformity. There were 15 females and the mean age was 63±5.601 years [Table/Fig-5].
Gender and age distribution.
| Demographic variables | N (%) |
|---|
| Gender |
| Female | 15 (75) |
| Male | 5 (25) |
| Age group (Years) |
| 55-60 | 10 (50) |
| 61-65 | 3 (15) |
| 66-70 | 5 (25) |
| 71-75 | 2 (10) |
The median function score improved from 50±5 to 80±0 [Table/Fig-6]. The difference in the function score from pre-operative period, day 5, 6 weeks preoperative and 3 months postoperative was statistically significant.
The functional outcome score measured preoperatively and postoperatively.
| Functional outcome score | Median | 25th percentile | 75th percentile | IQR | p-value |
|---|
| Preoperative | 50 | 45 | 50 | 5 | 0.001(Friedman’s Anova/Wilcoxon Signed test) |
| Postoperatively day 5 | 50 | 50 | 50 | 0 |
| Postoperatively 6 weeks | 70 | 70 | 70 | 0 |
| Postoperatively 3 months | 80 | 80 | 80 | 0 |
IQR: Interquartile range
The median knee score improved from 47±9 preoperatively to 93±3 postoperatively [Table/Fig-7]. The difference in the knee score from preoperative period, day 5, 6 weeks and 3 months was statistically significant.
The Knee Scores as analysed preoperatively and postoperatively.
| Knee scores analysis | Median knee score | 25th percentile | 75th percentile | IQR | p-value |
|---|
| Preoperative | 45 | 38 | 47 | 9 | 0.001(Friedman’s Anova/Wilcoxon Signed test) |
| Postoperative day 5 | 79 | 72.25 | 80.25 | 8 |
| Postoperative 6 weeks | 86.5 | 84.5 | 87 | 2.5 |
| Postoperative 3 months | 92 | 90 | 93 | 3 |
The correction of varus, seen radiologically, between preoperative, postoperative day 5 and 3 months postoperatively was statistically significant with p-value <0.05 (0.001) [Table/Fig-8].
Table showing correction of varus (radiological outcome).
| Radiological outcome | Mean±SD (degrees) | p-value |
|---|
| Preoperative | 17.74±2.46 | 0.001(ANOVA) |
| Postoperative day 5 | 1.76±0.677 |
| Postoperative 3 months | 1.76±0.677 |
Discussion
There are numerous studies which evaluated different methods for obtaining precise coronal alignment in the varus knee. Recently, the MTRO has been introduced as an alternative to medial soft tissue release, for correcting fixed varus knee deformities [20]. But there are limited data in the literature regarding the outcome of patients requiring an MTRO. So, the principal aim of the study was to assess the radiographic and clinical outcomes of MTRO in patients who underwent a varus TKA.
Thirty knees were evaluated in the study. These patients were suffering from knee pain and functional limitations. The functional outcome was assessed using the Knee Society Score which includes a Knee score and Function score. In the study, the change in knee scores and function scores preoperatively and postoperatively were statistically significant. The median knee score improved from 47±9 preoperatively to 93±3 postoperatively. Similarly, median function score improved from 50±5 to 80±0. Dixon MC et al., performed an MTRO on 10 patients with mean varus deformity of 24 degrees. Knee Society and function scores (24 and 34 to 94 and 85) showed great improvement and also no patient required revision surgery. The mean follow-up tibiofemoral angle was 4 degrees [22].
The radiological outcome was assessed using Hip-Knee-Ankle radiographs as they provide accurate information on the weight bearing mechanical axis. The surgical aim was to obtain a neutrally aligned lower limb with Hip-Knee-Ankle angle within 3° from mechanical axis as it was supposed to reduce the risk of abnormal wear, premature loosening, and early implant failure. The postoperative Hip-Knee-Ankle angle of all patients in the study was within this range.
Also, the correction of varus deformity based on Hip-Knee-Ankle angle was statistically significant. In this study, a mean correction of varus deformity from 17.74±2.460 preoperatively to 1.76±0.6770 postoperatively was achieved [Table/Fig-8]. Intraoperatively, no superficial MCL releases were required to achieve coronal balance and constrained implants were not used in any patients. Martin R et al., found out the excellent outcomes associated with MTRO using radiographic and clinical evaluation [10]. This study collated the outcomes of a matched cohort of patients that underwent TKA and compared between non MTRO and MTRO groups. Preoperatively, the tibiofemoral angle was 3.42° valgus versus 6.12° varus in the control and MTRO cohorts respectively (p=0.01). Mean postoperative tibiofemoral angles were 3.40° versus 2.43° valgus respectively. Postoperative Knee Society Scores were superior in the MTRO cohort (183.84 versus 174.58; p=0.04).
In this study, the amount of osteotomy done to attain the correction of residual varus deformity is not quantified. Mullaji AB et al., evaluated 71 primary TKAs in patients that required an MTRO and they quantified the effect of reduction osteotomy on the degree of varus deformity correction using intraoperative data [17]. For every 2 mm of tibial bone osteotomised, they achieved one degree of deformity correction. However, they did not studied about the effect of MTRO on clinical or radiographic outcome. Krackow KA et al., also reported a mean correction of 0.45° for every mm (millimeter) of bone resected in their study [4].
In this study, minimal medial soft tissue releases were done sequentially to attain the coronal ligamentous balance without releasing superficial MCL. The remaining varus deformity was corrected using MTRO. In another study by Mullaji AB et al., in 2005 evaluated 173 knees with varus deformity more than 20 degree [11]. Mean Knee Society score improved from 22.8 to 91.1, and function score from 22.8 to 72.1 at 2.6 years.
Dixon MC et al., reported no evidence of any osteolysis or component loosening in any of the patient at a mean follow-up of 42 months [22]. Zan P et al., conducted a study in 48 knees with bilateral varus knee deformity. They also found no case of premature loosening or subsidence of the tibia prosthesis with one-year follow-up [23]. Resorption of medial tibial bone can occur postoperatively secondary to thermal necrosis associated with performing an MTRO. In this study, there was no resorption of medial tibial bone. Rounger and irrigation were used for reduction osteotomy to decrease the chance of thermal necrosis.
Limitation(s)
This was a short-term study followed-up period was only 3 months. The amount of osteotomy performed was not measured in this study.
Conclusion(s)
The MTRO was found to be an effective method to achieve coronal ligamentous balance and alignment in patients with severe varus knee deformity more than 15 degree. The release of superficial MCL and use of constrained implant were not required in any patient. There was a statistically significant improvement in knee society scores and radiographic correction of varus deformity postoperatively. Hence, MTRO is recommended to achieve coronal balance in patients with severe varus knee deformity. Further studies examining long-term follow-up outcomes beyond two years are recommended for better results.
IQR: Interquartile range
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 21, 2020
Manual Googling: Mar 15, 2021
iThenticate Software: Apr 27, 2021 (25%)
[1]. Mullaji AB, Shetty GM, Correction of varus deformity during TKA with reduction osteotomyClin Orthop Relat Res 2014 472(1):126-32.10.1007/s11999-013-3077-523709274 [Google Scholar] [CrossRef] [PubMed]
[2]. Ahn JH, Back YW, Comparative study of two techniques for ligament balancing in total knee arthroplasty for severe varus knee: Medial soft tissue release vs. bony resection of proximal medial tibiaKnee Surg Relat Res 2013 25(1):13-18.10.5792/ksrr.2013.25.1.1323508134 [Google Scholar] [CrossRef] [PubMed]
[3]. Teeny SM, Krackow KA, Hungerford DS, Jones M, Primary total knee arthroplasty in patients with severe varus deformity. A comparative studyClin Orthop Relat Res 1991 (273):19-31.10.1097/00003086-199112000-00005 [Google Scholar] [CrossRef]
[4]. Krackow KA, Raju S, Puttaswamy MK, Medial over-resection of the tibia in total knee arthroplasty for varus deformity using computer navigationJ Arthroplasty 2015 30(5):766-69.10.1016/j.arth.2014.11.03425575730 [Google Scholar] [CrossRef] [PubMed]
[5]. Engh GA, The difficult knee: Severe varus and valgusClinical Orthopaedics and Related Research® 2003 416:58-63.10.1097/01.blo.0000092987.12414.fc14646739 [Google Scholar] [CrossRef] [PubMed]
[6]. Seo JG, Moon YW, Jo BC, Kim YT, Park SH, Soft tissue balancing of varus arthritic knee in minimally invasive surgery total knee arthroplasty: Comparison between posterior oblique ligament release and superficial MCL releaseKnee Surg Relat Res 2013 25(2):60-64.10.5792/ksrr.2013.25.2.6023741700 [Google Scholar] [CrossRef] [PubMed]
[7]. Saeki K, Mihalko WM, Patel V, Conway J, Naito M, Thrum H, Stability after medial collateral ligament release in total knee arthroplastyClinical Orthopaedics and Related Research® 2001 392:184-89.10.1097/00003086-200111000-0002211716381 [Google Scholar] [CrossRef] [PubMed]
[8]. Meneghini RM, Daluga AT, Sturgis LA, Lieberman JR, Is the pie-crusting technique safe for MCL release in varus deformity correction in total knee arthroplasty?J Arthroplasty 2013 28(8):1306-09.10.1016/j.arth.2013.04.00223680500 [Google Scholar] [CrossRef] [PubMed]
[9]. Mihalko WM, Saeki K, Whiteside LA, Effect of medial epicondylar osteotomy on soft tissue balancing in total knee arthroplastyOrthopedics 2013 36(11):e1353-57.10.3928/01477447-20131021-1424200437 [Google Scholar] [CrossRef] [PubMed]
[10]. Martin R, Levy D, Miner T, Conrad D, Jennings J, Dennis D, Medial tibial reduction osteotomy is associated with excellent outcomes and improved coronal alignmentReconstructive Review 2017 7(1):32-38.10.15438/rr.7.1.166 [Google Scholar] [CrossRef]
[11]. Mullaji AB, Padmanabhan V, Jindal G, Total knee arthroplasty for profound varus deformity: Technique and radiological results in 173 knees with varus of more than 20 degreesJ Arthroplasty 2005 20(5):550-61.10.1016/j.arth.2005.04.00916309988 [Google Scholar] [CrossRef] [PubMed]
[12]. Skyttä ET, Lohman M, Tallroth K, Remes V, Comparison of standard anteroposterior knee and hip-to-ankle radiographs in determining the lower limb and implant alignment after total knee arthroplastyScand J Surg 2009 98(4):250-53.10.1177/14574969090980041120218424 [Google Scholar] [CrossRef] [PubMed]
[13]. Skyttä ET, Haapamäki V, Koivikko M, Huhtala H, Remes V, Reliability of the hip-to-ankle radiograph in determining the knee and implant alignment after total knee arthroplastyActa Orthop Belg 2011 77(3):329-35. [Google Scholar]
[14]. Abu-Rajab RB, Deakin AH, Kandasami M, McGlynn J, Picard F, Kinninmonth AWG, Hip-Knee-ankle radiographs are more appropriate for assessment of postoperative mechanical alignment of total knee arthroplasties than standard AP knee radiographsJ Arthroplasty 2015 30(4):695-700.10.1016/j.arth.2014.11.02425702592 [Google Scholar] [CrossRef] [PubMed]
[15]. Matassi F, Cozzi Lepri A, Innocenti M, Zanna L, Civinini R, Innocenti M, Total knee arthroplasty in patients with extra-articular deformity: Restoration of mechanical alignment using accelerometer-based navigation systemJ Arthroplasty 2019 34(4):676-81.10.1016/j.arth.2018.12.04230685259 [Google Scholar] [CrossRef] [PubMed]
[16]. Slevin O, Hirschmann A, Schiapparelli FF, Amsler F, Huegli RW, Hirschmann MT, Neutral alignment leads to higher knee society scores after total knee arthroplasty in preoperatively non-varus patients: A prospective clinical study using 3D-CTKnee Surg Sports Traumatol Arthrosc 2018 26(6):1602-09.10.1007/s00167-017-4744-y29026941 [Google Scholar] [CrossRef] [PubMed]
[17]. Mullaji AB, Shetty GM, Lingaraju AP, Bhayde S, Which factors increase risk of malalignment of the hip-knee-ankle axis in TKA?Clin Orthop Relat Res 2013 471(1):134-41.10.1007/s11999-012-2520-322895692 [Google Scholar] [CrossRef] [PubMed]
[18]. Insall JN, Dorr LD, Scott RD, Scott WN, Rationale of the Knee Society clinical rating systemClin Orthop Relat Res 1989 (248):13-14.10.1097/00003086-198911000-00004 [Google Scholar] [CrossRef]
[19]. Huddleston J, Gobezie R, Rubash H, Revision Total Knee Arthroplasty springer:411/117-128http://eknygos.lsmuni.lt/springer/411/117-128.pdf [Google Scholar]
[20]. Ahn JH, Yang TY, Lee JY, Reduction osteotomy vs pie-crust technique as possible alternative for medial release in total knee arthroplasty and compared in a prospective randomized controlled trialThe Journal of Arthroplasty 016 31(7):1470-75.10.1016/j.arth.2016.01.01826869062 [Google Scholar] [CrossRef] [PubMed]
[21]. Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN, The New Knee Society Knee Scoring SystemClin Orthop Relat Res 2012 470(1):03-19.10.1007/s11999-011-2135-022045067 [Google Scholar] [CrossRef] [PubMed]
[22]. Dixon MC, Parsch D, Brown RR, Scott RD, The correction of severe varus deformity in total knee arthroplasty bytibial component downsizing and resection of uncapped proximal medial boneThe Journal of Arthroplasty 2004 19(1):19-22.10.1016/j.arth.2003.08.00114716645 [Google Scholar] [CrossRef] [PubMed]
[23]. Zan P, Fan L, Liu K, Yang Y, Hu S, Li G, Reduction osteotomy versus extensive lease on clinical outcome measures in simultaneous bilateral total knee arthroplastyMed Sci Monit 2017 23:3817-23.10.12659/MSM.90581528781360 [Google Scholar] [CrossRef] [PubMed]