Vitiligo is a disorder of skin pigmentation that is associated with tremendous psychological impact on the affected patients [1,2]. Vitiligo was referred to as SwetaKustha, which means “White Leprosy”. Hence, it was considered as a social taboo thus, severely impaired the quality of life. More so in Indian scenario in view of dark skin colour [2].
It is caused by selective destruction of epidermal melanocytes resulting in the formation of well-defined depigmented patches. The prevalence of vitiligo range from 0.1% to 8% [3]. The NBUVB therapy has been reported to be effective and a safe tool in vitiligo [4-6]. The exact mechanism of action of NBUVB in vitiligo is unknown. The predominant type of repigmentation after NBUVB is perifollicular. It exert its pigmentary effect in vitiligo through a two-step process. Both the steps occur simultaneously; the first step is stabilisation of the depigmenting process and second step is the stimulation of residual follicular melanocytes in the outer root sheath of a hair follicle, which are activated to proliferate and produce melanin [7,8].
Although there is enough literature to support utilisation of NBUVB phototherapy in vitiligo patients, the impact of this treatment on quality of life of these patients is not addressed adequately in the literature. There is no reported literature on quality of life before and after NBUVB phototherapy in South Indian dark skin population with vitiligo. Hence, this study was conducted to determine the effect of NBUVB treatment on vitiligo patients and to assess the impact on DLQI of patients before and after the therapy.
Materials and Methods
This was a prospective interventional study with pre and post study design. All the vitiligo patients attending Dermatology OPD at BGS Global Institute of Medical Sciences, Bengaluru, Karnataka, India from January 2019 to June 2019 were considered for the study. The study patients were recruited for six months. The three months treatment for patients recruited in June 2019 was completed by September 2019 and the follow-up of the last patient lasted for a period of another six months making the the total time period of the study from January 2019 to March 2020.
The study was conducted after obtaining Institutional Ethical Clearance Number (BGS GIMS/IEC/2018-19/28). An informed consent was obtained from all the patients regarding the treatment protocol before including them into the study. This study was done in the OPD setting.
Inclusion criteria: All adult patients aged above 18 years with vitiligo with depigmented patches involving more than 10% of body surface area since these patients were assumed to have decreased quality of life as compared to involvement of less than 10% body surface area were included.
Exclusion criteria: Patients with history of photosensitising disorders, those suffering from claustrophobia, patients with segmental vitiligo, the vitiligo patients with history of spontaneous repigmentation and patients with active infection were excluded.
The selected patients were advised to stop any previous treatment for at least four weeks before NBUVB monotherapy. These patients were further followed-up for six months to look for relapse of depigmentation patches.
A complete general, systemic, and dermatological examination was carried out, taking into account the number of depigmented macules and site of involvement. Complete blood count was done in all the patients. The equipment used was Whole-body, NB unit with 12 tubes (TL-01)-100 W, 6 ft. Ultraviolet glasses were used as eye shield.
The treatment was started with an initial dose of 300 mJ/cm2 in all the cases. It was administered twice a week excluding the weekends. It was administered on non consecutive days to allow for regeneration of cells. The NBUVB dose was increased by 50 mJ/cm2 on each subsequent visit. The optimal dose was determined once minimal erythema in the lesion was noticed and no further increment in the dose was done. In the present study, Minimal Erythema Dose (MED) was not calculated, instead the NBUVB therapy was initiated with a dose of 300 mJ/cm2 and gradually increased by 50 mJ/cm2 every sitting till MED was achieved. The treatment was withheld in case of any side effects such as severe erythema, burning pain, severe itching or blistering until its resolution and the irradiation dose was decreased by 50 mJ for further treatment. All the patients were asked to use sunscreens during daytime to avoid skin burns. Emollients were used at night. The maximum period of treatment was three months. It was stopped earlier if 75% or greater repigmentation was achieved in the course of treatment. The grade of repigmentation of vitiligo patches were classified as excellent (>75%), good (51-75%), average (25-50%) and poor (<25%) [9].
Dermatology Life Quality Index Questionnaire
The DLQI questionnaire designed by Finlay AY and Khan GK was used to determine the quality of life impairment in the study patients [10]. The DLQI consisted of 10 different questions, each one with four possible answers scored from 0 to 3, giving a maximum score of 30 and a minimum score of 0. The interpretation of meaning of DLQI scores was as follows: 0-1 no effect at all on patient’s life, 2-5 small effect on patient’s life, 6-10 moderate effect on patient’s life, 11-20 very large effect on patient’s life, 21-30 extremely large effect on patient’s life. The greater the score, the more the patient’s quality of life was impaired. The DLQI scoring was done twice, the first scoring at the start of therapy and the second scoring at the end of therapy. The scores were recorded for all the study patients. Further the patients were followed-up every four weeks for a duration of six months to observe for stability of repigmentation.
Statistical Analysis
All data collected were entered in MS Excel spreadsheet. Descriptive statistics were elaborated in the form of Mean, SD, and percentages. The DLQI before and after the therapy is compared using a non parametric test, i.e., Wilcoxon signed Rank Test. Data were analysed using statistical software SPSS version 20.0.
Results
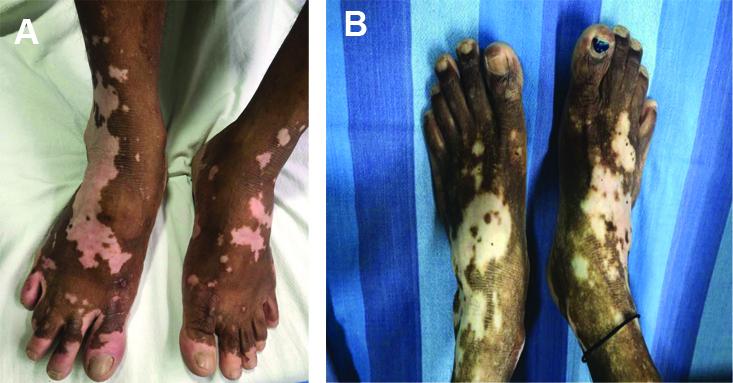
A total of 79 patients were included in the study. Age ranged from 18 to 72 years, with a mean age of 43.2±15.14 years. The mean body surface area involved was 34±6%. All the patients included in the study had generalised vitiligo or vitiligo vulgaris with or without acral vitiligo and lip tip vitiligo. Only 2 (2.5%) patients had family history of vitiligo and the remaining 77 (97.5%) did not have any family history. The sex distribution among study patients was almost equal, with 39 females and 40 males. The co-morbidities in the study population were seen in 32 (40.5%) patients. They were diabetes mellitus (n=24) and hypertension (n=8). The blood sugar levels and blood pressure were within acceptable limits as they were being treated optimally. The duration since patient had vitiligo depigmented patches ranged from two months to 120 months, with mean duration of 27.94±27.92 months. The distribution of study population based on duration of depigmented patches is represented in [Table/Fig-1]. However, there was no variation in the response to treatment among these group of patients. The distribution of patches on the body included following sites such as hand, forearm, arm, foot, leg, thigh, abdomen, chest, back, face and neck [Table/Fig-2,3]. The total body area of involvement with depigmented patches was more than 10% in all the patients. Hence, wholebody irradiation was done for all the patients. The cumulative number of NBUVB irradiation sessions ranged from 14 to 48, with an average of 22.65±7.42 sessions.
Distribution of study population based on duration of depigmented patches.
| Duration of vitiligo depigmented patches (in months) | Number of patients (Total=79) | Percentage (%) |
|---|
| 2-6 | 18 | 22.8 |
| 7-12 | 24 | 30.4 |
| 13-60 | 27 | 34.2 |
| 61-120 | 10 | 12.6 |
Depigmented vitiligo patches on the dorsum of the hand.

Depigmented vitiligo patches on the dorsum of the foot.
The grade of repigmentation in the study group was excellent in 2 (2.5%), good in 52 (65.8%), average in 25 (31.7%) and poor in none. The average rate of repigmentation among study population was 57.52±13.1%.
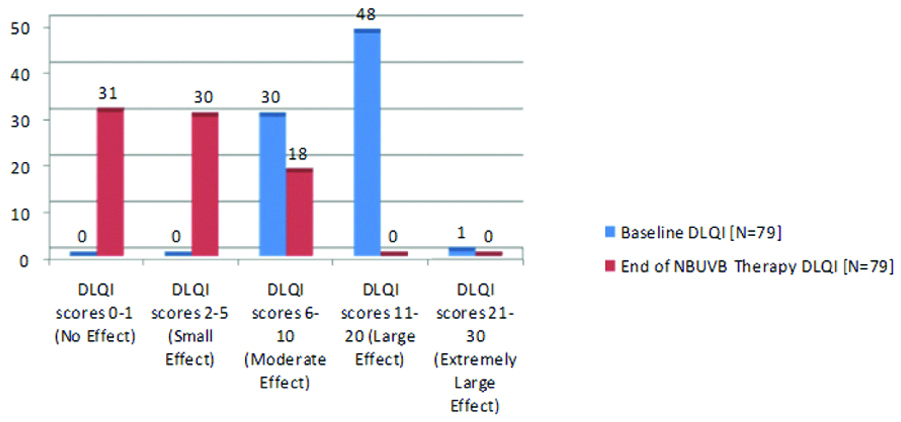
Among the study patients, the baseline DLQI score distribution ranged from 6 to 28, with mean score of 11.76±3.69. None of the study patients baseline DLQI score was <6. The end of therapy DLQI score ranged from 0-7, with mean score of 2.58±2.32. None of the study patients end of therapy DLQI score was >7 [Table/Fig-4]. The difference between the mean baseline DLQI score (11.76±3.69) and end of therapy DLQI score (2.58±2.32) was statistically significant (p=0.001). The DLQI before and after the therapy is compared using a non parametric test, i.e., Wilcoxon signed Rank Test.
The Effect of NBUVB therapy on Dermatology Life Quality Index (DLQI).
The adverse reaction was noted in 17 (21.5%) patients, of which 14 (17.7%) had erythema and 3 (3.8%) had itching. The relapse of depigmented macules in the present study was in 21 patients (26.5%) at six months follow-up.
Discussion
Vitiligo is caused by selective destruction of epidermal melanocytes resulting in the formation of well-defined depigmented patches. At present, NBUVB phototherapy is considered the treatment of choice in patients with generalised vitiligo [4-6].
The NBUVB therapy is far more effective, superior, and less dangerous when compared to PUVA therapy [11,12]. Nicolaidou E et al., suggested that initiation of phototherapy at 300 mJ/cm2 for skin types III-V with increments at 50 mJ/cm2 till Minimal Erythema Dose (MED) [13]. Kumar YHK et al., suggested 20% increment in dose of NBUVB till erythema [14]. Serish and Srinivas CR reported that mean MED for NBUVB as 300 mJ/cm2 for the Indian skin [15]. In the present study, MED was not calculated, instead the NBUVB therapy was initiated with a dose of 300 mJ/cm2 and gradually increased by 50 mJ/cm2 every sitting till MED was achieved.
Chahar YS et al., reported mean number of exposures 45.63±12.74 to achieve a repigmentation of 38.65% [16], whereas Njoo MD et al., reported similar repigmentation with more number of exposures (76.3±16.7) [5]. Similar observations were reported in another study by Yones SS et al., also [17]. In the present study, mean number of NBUVB irradiation exposure sessions required to achieve repigmentation of 57.52% was 22.65±7.42. Notably in the present study, less number of exposure sessions were required to achieve similar or better repigmentation in the vitiligo patches.
The mean baseline DLQI score in various studies were 8.64±4.32 in the study by Chahar YS et al., [16], mean score of 7.3 in the study by Finlay AY and Khan GK [10], a mean score of 4.82 in the study by Kent G and al-Abadie M [18] and mean baseline DLQI score of 10.67 in the study by Sangma LN et al., [19]. The difference in the baseline DLQI scores between these studies might be due to vitiligo causing greater quality of life impairment in the darker skin due to increased contrast between vitiligo patches and normal skin. The mean baseline DLQI score in our study was 11.76±3.69, which is high as compared to published literature. This can be explained because of darker complexion of our study patients (South Indian Population).
In the study done by Chahar YS et al., after NBUVB phototherapy, DLQI score reduced from a baseline score of 8.64±4.32 to end of therapy score of 5.86±2.15 [16]. Similarly in another study by Mou KH et al., the baseline DLQI score was 6.3±4.8 and after NBUVB therapy the score was 3.1±2.4 [20]. In the present study, after NBUVB irradiation for vitiligo patches the mean DLQI score reduced from 11.76±3.69 to 2.58±2.32, and was statistically significant. As it is noticed, in the present study the baseline DLQI score was higher than the reported literature. Hence, overall improvement in the quality of life was marginally better in patients as compared to reported literature.
After NBUVB therapy, relapse of depigmentation lesions on repigmented skin is noticed at varied rates in different studies. Natta R et al., reported a relapse of 25% and 43% at one and one and a half years [21], respectively, while Nicolaidou E et al., found a relapse rate of 44% within one year of stopping the treatment [13]. The relapse of depigmented macules in the present study was (n=21) 26% at six months follow-up, this is similar to the published reports. The adverse effects noticed in the present study such as erythema and itching were similar to that reported in various other studies [13,22].
Limitation(s)
The limitations in the present study were, the pre and post intervention assessment of DLQI score was not done separately based on the location of vitiligo patches such as neck, face, trunk and limbs and also based on duration of depigmented patches. It could not be done as number of study patients were not large enough.
Conclusion(s)
Narrow Band Ultraviolet B (NBUVB) treatment is effective on vitiligo patients in achieving repigmentation of depigmented patches. The baseline DLQI score of vitiligo patients were high, and it significantly decreased after the NBUVB therapy, thus reducing the patient suffering.