Cataract surgery is the most commonly performed procedure in ophthalmic practice. It can provide good visual outcomes for most patients, owing to developments in surgical techniques, instrumentation and IOL technology. Despite advances in lens design and material, late complications associated with PCO cannot be always prevented [1].
PCO can be decreased when the IOL is in complete contact with the anterior capsule. There are multiple reports which have found that visually significant PCO rate could be 11.8% at one year, 20.7% at three years and 28.4% at five years after cataract surgery [2]. The PCO can lead to clinically significant reduction in visual acuity, impaired contrast sensitivity, glare disability and monocular diplopia [3].
There are many risk factors associated with formation of PCO. Diabetics have more propensity to develop PCO as compared to non diabetics. Other risk factors in which PCO formation occurs include uveitis, high myopia, retinitis pigmentosa, traumatic cataract and myotonic dystrophy. The PCO formation in cases of hydrophobic acrylic lens is less as compared to other IOL materials such as Polymethyl Methacrylate (PMMA) and hydrophilic acrylic lens [4].
The patients who have PCO with significantly reduced vision need opening up of posterior capsule. The techniques for posterior capsulotomy include Nd:YAG capsulotomy and surgical capsulotomy. The Nd:YAG laser capsulotomy is the procedure of choice done in PCO with a success rate of more than 95% [5]. The Nd:YAG laser is a man-made crystal of Neodymium doped Yttrium, Aluminium-Garnet. The Nd:YAG laser is a solid laser which causes tissue disruption by ionisation. Wavelength of the laser is 1064 nm. Therefore, it is a photo disrupter unlike the argon or krypton lasers [3].
Most common adverse effects of Nd:YAG laser capsulotomy include intraocular pressure elevation, cystoid macular oedema, endothelial cells reduction and damage, retinal tears and detachment and, most commonly, IOL damage, or so-called pitting [2].
The corneal endothelium is a single layer of polygonal cells that is firmly attached to Descemet’s membrane and is in contact with aqueous humour. It controls relative state of dehydration of corneal stroma through an active pumping mechanism and thereby provides transparency to cornea [4].
The structure and function of corneal endothelium in this study has been assessed by non contact specular microscopy. Modern specular microscopes use computer-assisted software to analyse shape, size and population of endothelial cells. It uses light that projects onto cornea and captures the image reflected from optical interface between corneal endothelium and aqueous humour. The reflected image is then analysed by the instrument and displayed as a specular photomicrograph [4].
Since there are very few studies in literature which have analysed the effects of Nd:YAG laser capsulotomy on corneal endothelium, this study was carried out to assess the corneal endothelial cell morphology and function before and after the laser procedure.
The main objectives of the present study were to compare the Cell Density (CD) and CV in pre and post Nd:YAG capsulotomy.
Materials and Methods
This was a prospective observational study conducted in the Out Patient Department (OPD) of Ophthalmology at Bharati Vidyapeeth (Deemed to be University) Medical College and Hospital, Sangli, Maharashtra, India from October 2020 to February 2021. The study was conducted in accordance with the ethical standards of Declaration of Helsinki and was approved by Institutional Ethical Committee (IEC, letter No. 395). Written informed consent was taken from patients.
Inclusion criteria: All patients presenting to Ophthalmology Department with PCO and undergoing Nd:YAG laser capsulotomy in the age group ranging from 35 years to 85 years were included in the study.
Exclusion criteria: Patients with corneal pathology like endothelial dystrophy, corneal scar or trauma, retinal pathology, pseudo exfoliation syndrome, active uveitis, traumatic cataract and patients with diabetes were excluded.
Study Procedure
Fifty eyes of 50 patients having developed PCO who presented during the study period were included in this study. Ophthalmic examination, including visual acuity assessment with Snellen’s visual acuity chart for distance; aided and unaided along with pinhole, anterior segment slit lamp examination, fundus examination using 90D lens and Indirect Ophthalmoscopy (IDO) and specular microscopy was done in all patients. Applanation tonometry was done to record IOP.
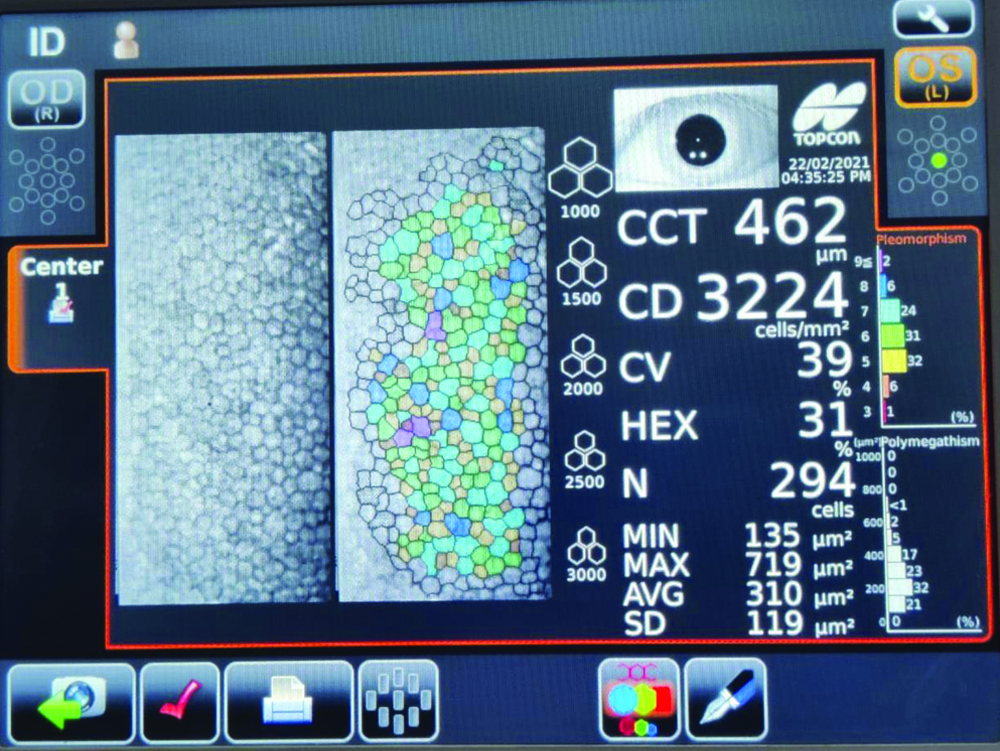
Specular microscopy was performed using a non contact specular microscope Topcon SP-3000P [Table/Fig-1]. Automatic mode was used to capture central area of cornea. Corneal ECD was calculated using cell centre method. Standard deviation of endothelial cell size from mean, CV and hexagonality was also evaluated.
Image showing the parameters measured by specular microscopy.
Before treatment with Nd:YAG laser, patient’s pupils were dilated using tropicamide 0.8% and phenylephrine 5%. A 0.5% proparacaine hydrochloride drops were instilled for anaesthetising cornea. Patients were then subjected to Q-switched Nd:YAG laser capsulotomy in the affected eye after measuring the IOP. The Nd:YAG capsulotomy was performed on a slit lamp equipped with Nd:YAG laser, with patient in seated position. Patient was asked to fixate the other eye at fixation target. Adjustment of stool, table and chin rest was done for optimal patient comfort.
The energy used for procedure ranged from 1.8-4.2 mJ depending on the type and thickness of PCO. The laser beam was placed at 125 μm posterior focusing mode. A 4 mm cruciate opening, beginning superiorly near 12 o’clock position and progressing downward toward 6 o’clock position was made. Shots were then placed at the edge of capsule opening, progressing laterally towards 3 and 9 o’clock positions. While performing Nd:YAG laser procedure in each eye, number of laser pulses was counted.
Postprocedure, patients were prescribed topical flurbiprofen eye drops thrice a day for two weeks and topical timolol (0.5%) eye drops twice a day for a week. The patients were then followed-up at one week and one month postprocedure. At each visit, BCVA, ECD, CV and hexagonality were assessed.
Statistical Analysis
All data were analysed by statistical software SPSS v26. Chi-square test and one-way repeated measures ANOVA test were applied and p-value <0.05 was considered significant.
Results
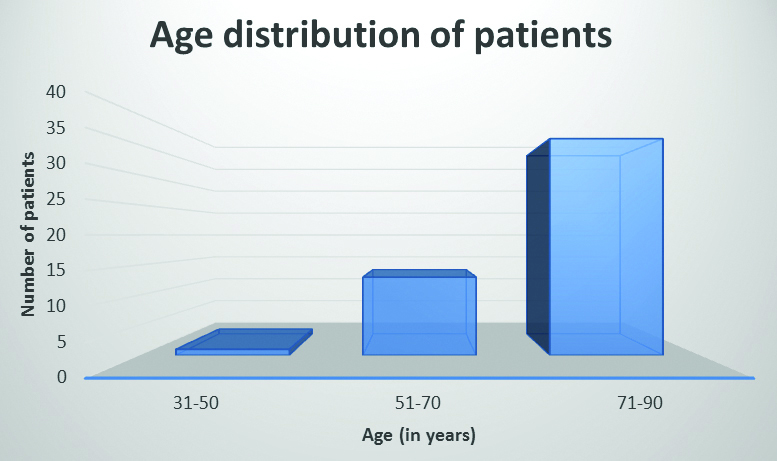
The study included 50 eyes of 50 patients who underwent Nd:YAG laser capsulotomy. All patients were aged between 35 to 85 years with majority of patients (72%) being above 60 years of age [Table/Fig-2].
Age distribution of patients.
The study included 23 females (46%) and 27 males (54%). The laterality distribution of eyes was right eye in 56% patients and left eye in 44% patients. Out of 50 eyes, 34 eyes (68%) had Elschnig’s Pearls type of PCO and 16 eyes (32%) had fibrosis type of PCO.
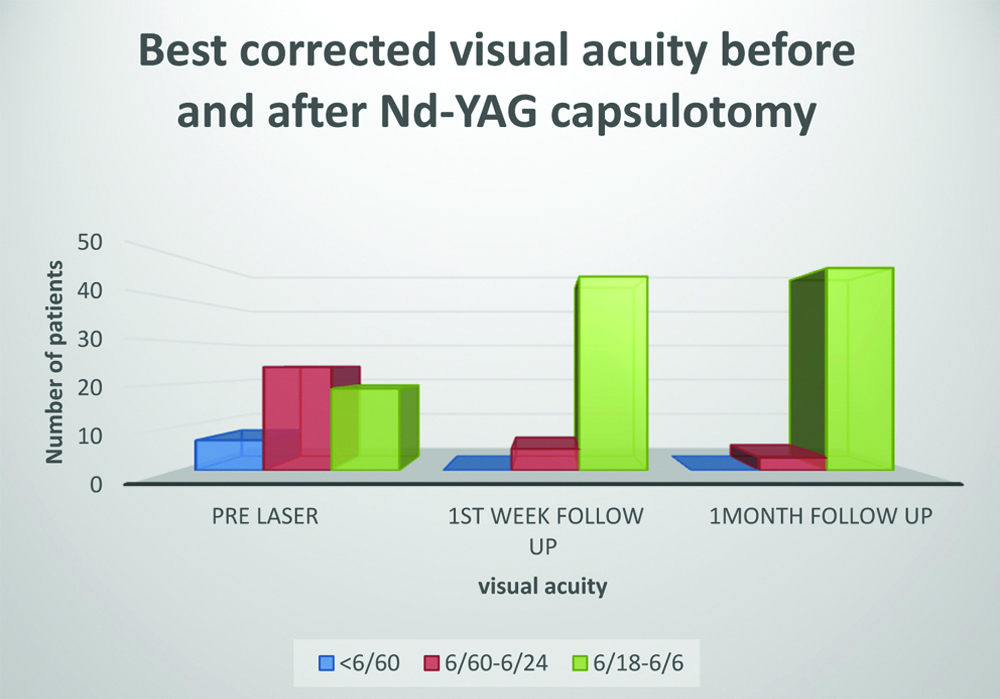
[Table/Fig-3] shows Visual Acuity outcome after Nd:YAG Laser Capsulotomy. Prelaser, majority of patients, i.e., 48% had visual acuity ranging from 6/60-6/24, 38% patients had visual acuity ranging from 6/18-6/6 and 14% patients had visual acuity worse than 6/60. Following Nd:YAG laser, 45 patients (90%) gained a BCVA of 6/18 or better after one week and 47 patients (94%) gained a BCVA of 6/18 or better after one month. The result was statistically highly significant (p<0.0001).
Image showing Best Corrected Visual Acuity (BCVA) before and after Nd:YAG laser capsulotomy.
The energy levels required for different types of PCO are shown in [Table/Fig-4]. The total cumulative energy (energy per pulse in mJ X number of pulses) required to perform adequate capsulotomy ranged from 25 to 110 mJ. Mean energy required for Elschnig Pearls type PCO was 54 mJ while for fibrous type of PCO, higher energy i.e., 86 mJ was required. Results indicate that percentage of patients who required less than 50 mJ cumulative energy was significantly more among patients with Elschnig Pearls PCO as compared with those with Fibrosis PCO. As against this, the percentage of patients who required more than 75 mJ cumulative energy was significantly less among patients with elschnig Pearls PCO as compared with those with fibrosis PCO. The result is statistically highly significant (Chi-square is 26.02, p<0.0001).
Energy levels required in different types of PCO.
| Cumulative laser energy in mJ. | Elschnig’s pearls | Fibrosis |
|---|
| Cases | % | Cases | % |
|---|
| <25 | 1 | 2.94% | 0 | 0 |
| 26-50 | 10 | 29.42% | 1 | 6.25% |
| 51-75 | 22 | 64.70% | 4 | 25% |
| 76-100 | 1 | 2.94% | 10 | 62.5% |
| 101-125 | 0 | 0 | 1 | 6.25% |
| Total | 34 | 100% | 16 | 100% |
| χ2*=26.02, p†=0.0003 |
*Chi-square value, †statistically significant p-value as measured by chi-square test
[Table/Fig-5] show the comparison of ECD at prelaser, one week and one month follow-up. Mean ECD prelaser was 2356.76 cells/mm2, which further decreased to 2231.8 cells/mm2 and 2199.2 cells/mm2 at one week and one month follow-up, respectively. The results indicate that there was statistically significant reduction in ECD from prelaser status to one month follow-up (p<0.0001) as measured by one way repeated measures ANOVA test.
Comparison of ECD prelaser, one week and one month follow-up.
| Parameters | Mean ECD (cells/mm2) | SD | F* | p-value† |
|---|
| Prelaser | 2356.76 | 213.092828 | 1911.8 | <0.0001 |
| One week | 2231.8 | 208.60127 |
| One month | 2199.2 | 209.563395 |
*F-Ratio †Statistically significant p-value as measured by one-way repeated measures ANOVA test
The mean CV before laser procedure was 33.74%. The CV increased to 35.58% at one week and 37.22% at one month follow-up. As shown in [Table/Fig-6], there was a gradual increase in CV from prelaser status to one month follow-up and this was statistically significant (p<0.0001) as shown by one-way repeated measures ANOVA test.
Comparison of CV prelaser, one week and one month follow-up.
| Parameters | Mean CV (%) | SD | F* | p-value† |
|---|
| Prelaser | 33.74 | 2.02847082 | 402.41 | <0.0001 |
| One week | 35.58 | 1.99069263 |
| One month | 37.22 | 2.13130218 |
*F-Ratio †Statistically significant p-value as measured by one-way repeated measures ANOVA test
The comparison of hexagonal cells prelaser and at one week and one month follow-up is shown in [Table/Fig-7]. The mean hexagonality at baseline was 65.34% which gradually decreased to 62.02% at one week and 60.42% at one month follow-up. Decrease in hexagonality from baseline to one month was measured by one way ANOVA test and was statistically significant (p<0.0001).
Comparison of hexagonal cells prelaser, one week and one month follow-up.
| Parameters | Mean Hexagonal Cells (%) | SD | F* | p-value† |
|---|
| Prelaser | 65.34 | 2.65429955 | 852.8 | <0.0001 |
| One week | 62.02 | 2.56737776 |
| One month | 60.42 | 2.40823417 |
*F-Ratio †Statistically significant p-value as measured by one-way repeated measures ANOVA test
Discussion
Visually significant PCO is the most common late complication of uncomplicated cataract surgery. The Nd:YAG laser has become a popular, effective and non invasive technique of creating a posterior capsulotomy in pseudophakic eyes with PCO [6].
A total of 50 eyes of 50 patients were included and analysed in the present study. There were 23 (46%) females and 27 (54%) males. There was no significant sex predilection among the patients who developed PCO. Cataract is leading cause of blindness worldwide and occurs equally among males and females. Complications like PCO also occur in equal proportions irrespective of gender. This is in agreement with the study of Aslam TM et al., Dharmaraju B et al., and Spalton DJ [7-9].
In the present study, out of 50 cases, 49 (98%) cases were in the age more than 40 years. This is perhaps the age at which patients with age related cataract present to the ophthalmologist and a greater number of cataract surgeries are performed as the age increases.
Out of 50 eyes, 68% eyes had elschnig’s Pearls type of PCO and 32% eyes had fibrosis type of PCO. The energy required to break posterior capsule depends upon the type of PCO. The fibrosis type of PCO being thicker requires more energy to create a capsulotomy. In our study, the fibrosis type PCO required a mean energy of 86 mJ which was significantly higher as compared to 50 mJ mean energy required for Elschnig’s Pearls type PCO. In a study [3], the mean energy required for fibrosis type PCO was 63.43 mJ and Elschnig’s Pearls type PCO was 51.22 mJ. Agarwal G et al., in their study also reported that a significantly higher mean energy was required for Fibrosis type PCO as compared to Elschnig’s Pearls type PCO [2].
In the present study, following Nd:YAG laser capsulotomy, 45 patients (90%) had a BCVA of 6/18 or better after one week. After one month, additional two patients i.e., total 47 patients (94%) gained visual acuity of ≥6/18. This shows that Nd:YAG capsulotomy in PCO improves patients’ BCVA with necessary refractive correction. Dharmaraju B et al., in his study on 100 patients undergoing Nd:YAG laser capsulotomy noted improvement in BCVA in 95% cases [8]. A similar study reported that nearly 90% patients had two or more than two Snellen’s line visual improvement following Nd:YAG laser capsulotomy [3].
The ECD in the present study ranged from 1895 to 2691 cells/mm2, with a mean ECD of 2356.76 cells/mm2 before laser treatment. The mean ECD reduced to 2231.8 at one week and 2199.2 cells/mm2 at one month follow-up. The difference between prelaser ECD and at one week was 124.56 cells/mm2. The difference between prelaser ECD and at one month was 157.56 cells/mm2 which shows that there was statistically significant reduction in ECD from prelaser status to one month follow-up (p<0.0001). The statistically significant reduction in ECD and hexagonality from prelaser status to one month could be attributed to a reduction in the activity of sodium-potassium.
The Adenosine triphosphate (ATP) pump in the endothelial cells thereby causes a decrease in cell number and distortion of the cell architecture with time [10]. A similar study by Rajappa N et al., reported a mean ECD of 2298.7 cells/mm2 before laser treatment, 2178.1 cells/mm2 at one week and 2121.3 cells/mm2 at 12 weeks following Nd:YAG Laser Capsulotomy [3]. There was a significant difference in ECD before and after laser treatment which correlates with findings of our study.
In a study by Qasim KF and Hasanain AR, mean ECD was 2047 cells/mm2 pre Nd:YAG Laser Capsulotomy, 1938 cells/mm2 at one week and 1916 cells/mm2 at one month follow-up [4]. The difference in mean ECD from prelaser status to one week was not significant whereas the difference in mean ECD from prelaser status to one month was statistically significant (p=0.025). These findings were comparable with those of the present study.
Kanchanaranya N and Sonthirathi S, in their study included 41 patients with PCO and found that the mean ECD prelaser was 2213 cells/mm2, which decreased to 2177 cells/mm2 at one month and 2237 cells/mm2 at three months postlaser [11]. The difference in ECD between prelaser and postlaser at one and three months were statistically insignificant.
There is wide variation in the absolute numbers of endothelial cells lost following Nd:YAG laser capsulotomy. This variation may be caused by several other factors such as the accuracy of technician’s endothelial cell measurement, the target tissue-endothelium distance, differences in delivery of the laser energy and the duration from cataract surgery to Nd:YAG laser capsulotomy. Further studies are thus, necessary to identify the significance of these factors.
Coefficient of variation represents the degree of variation in the sizes of the endothelial cells i.e., polymegathism. By measuring the variation in size between endothelial cells, we can measure how much cell loss is occurring. In our study, the mean CV prelaser was 33.74, at one week was 35.58 and at one month it was 37.22. The difference in CV from prelaser to one week was not significant. However, the difference in CV from prelaser status to one month was statistically significant (p<0.0001). A study reported a mean baseline CV of 33.7, 34.3 at one week and 34.5 at 12 weeks [3]. The difference in mean CV from baseline to one week and 12 weeks was not statistically significant.
Pleomorphism is a significant disruption in the regular hexagonal pattern of the endothelium that causes a decrease in endothelial mosaic stability. Thus, hexagonality represents the predominant cell shape in normal corneal endothelium. The mean hexagonality in our study at baseline was 65.34% which gradually decreased to 62.02% at 1 week and 60.42% at one month follow-up. The difference in hexagonality between one month and baseline was statistically significant. Rajappa N et al., in their study reported a mean hexagonality of 72.22% prelaser, 71.42% at one week (p<0.005) and 70.22% at 12 weeks (p<0.0001) which was significant, thus correlating with our study [3].
The Nd:YAG laser capsulotomy induced endothelial cell loss is in direct proportion to the energy used during the procedure. The study stresses on evaluating corneal endothelium by using Specular Microscopy in each and every case undergoing Nd:YAG capsulotomy. Also, effective use of energy in minimising endothelial cell loss will help in minimising corneal endothelial damage.
Limitation(s)
A major limitation of the present study was the relatively smaller sample size of 50 patients. Another limitation was that the duration of follow-up was shorter and the ECD was not recorded beyond one month. In addition, due to the smaller sample size, we have not correlated the energy used during the laser procedure with the amount of endothelial cell loss.
Conclusion(s)
The Nd:YAG laser capsulotomy is a safe, effective and non invasive method for the treatment of PCO. However, it is not devoid of complications and can cause damage to the corneal endothelial cells. The present study showed that there is a significant decrease in corneal ECD following Nd:YAG laser capsulotomy. Hence, in order to reduce the damage to corneal endothelial cells, it is necessary to minimise the laser energy delivered in the eye as much as possible. Damage to the corneal endothelial cells can also be reduced by ensuring that the posterior capsule is accurately focussed and the eye is stabilised by using a contact lens during the procedure.
*Chi-square value, †statistically significant p-value as measured by chi-square test
*F-Ratio †Statistically significant p-value as measured by one-way repeated measures ANOVA test
*F-Ratio †Statistically significant p-value as measured by one-way repeated measures ANOVA test
*F-Ratio †Statistically significant p-value as measured by one-way repeated measures ANOVA test