Patients who are given general anaesthesia, majority of them undergo endotracheal intubation resulting in injury of vocal cords or airway mucosa which causes POST [1,2]. POST is amongst the major problem post anaesthesia according to ASA [2,3]. Incidence of POST ranges between 21% to 65% [4-7] while that for HOV is between 4% to 42% [3].
There have been different methods used to attenuate POST, HOV and cough successfully [8,9]. The non-pharmacological methods such as a smaller size endotracheal tube, a well lubricated endotracheal tube with soluble jelly, gentle laryngoscopy after fully relaxed patient, appropriate cuff pressure and gentle suctioning showed decrease in the incidence of POST [8].
On the other hand, pharmacological measures include steroid inhalation and other medicine gargles. The ionotropic glutamate receptors N-Methyl-D-Aspartate (NMDA), alpha-amino-3-hydroxyl-5-methyl-4-isoxazolepropionic acid and kainate receptors are found in the central nervous system as well as the peripheral nerves [9]. Behavioural studies shows that activation of these receptors can cause nociceptive behaviour and inflammatory pain [9,10]. Moreover, experimental studies showed that peripherally administered NMDA receptor antagonists are involved with antinociception and anti-inflammatory cascade at opioid receptors located in the oral and upper respiratory tract mucosa [9,11-15] NMDA-receptor antagonists, interact with cytokines production, inflammatory cells recritment, and inflammatory mediator regulation. This suggest that ketamine may have an anti-proinflammatory effect thereby reducing systemic inflammation and promoting healing [11,12]. There are many studies on reduction of POST with use of ketamine gargles, which found that 40-50 mg ketamine was better in terms of POST, HOV and cough outcome postoperatively [4,6,8,9].
The present study aimed to observe the effect of ketamine gargle in POST, HOV and cough followed by endotracheal intubation during surgeries under general anaesthesia.
Materials and Methods
This randomised control study was carried out at Dhiraj hospital, Piparia, Vadodara in Department of Anaesthesiology, from February 2019 to November 2020. The randomised controlled study was conducted after clearance from the Institutional Ethical Committee (Study Approval No. SVIEC/ON/MEDI/BNPG18/D19046.
Inclusion Criteria
Patients willing to sign the written informed consent.
Patients from both the sex between 18 to 55 years.
Patients undergoing elective surgical procedures, not lasting more than 1 hour and 30 minutes duration under general anaesthesia.
Patients belonging to ASA I and II.
Exclusion Criteria
Patients with history of prior sore throat, patients with known upper respiratory tract infection or lower respiratory tract infection.
Patients with known allergy, sensitivity or any other form of reaction to study drug.
Patients with anticipated difficult airway (Mallampati grade III and IV).
Patients with poor cardiovascular and respiratory reserve.
Sample size calculation: The power of study was calculated by using software G Power 3.0.10, taking the incidence of POST from the study of Canbay O et al., (65%) and considering a probability level of 0.05 (α-error) and power of 0.80 (1-β) yielded a sample size of 25 patients in each group [16].
Randomisation: Patients were allocated in a randomised manner by chit method into two groups of 25 each as group K to receive ketamine with normal saline and group C to receive normal saline. A consort flow diagram of patients and their progress through the various phases of this randomised trial is outlined in [Table/Fig-1].
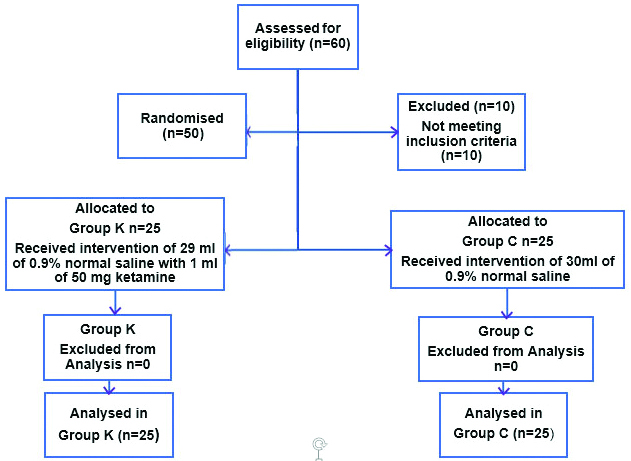
Intervention: Group K: ketamine 50 mg in 29 mL normal saline. Group C: 30 mL normal saline. Patients as well as anaesthesiologist for data collection were blinded for the study. Drug solution for the study were prepared by a different anaesthesiologist not involved in the study.
Patient intravenous access was obtained on the forearm with 18G i.v. cannula and fluids were started, after shifting to operating room. Heart rate, non-invasive blood pressure, SpO2 were monitored in multipara monitor. All patients were made to gargle for 30 seconds with the either ketamine or normal saline according to assigned group, 5 minutes prior to induction.
Intravenous injection ondansetron 0.1 mg/kg, injection glycopyrolate 0.04 mg/kg were given as premedication. Induction done with IV injection propofol 2 mg/kg and injection succinylcholine 2 mg/kg. Intubation was done with a soft seal cuffed sterile poly vinyl chloride endotracheal tube of 8-8.5 mm Internal Diameter (ID) in male and 7-7.5 mm ID in female. Endotracheal tube cuff inflated until no audible leak was heard. Anaesthesia was maintained on isoflurane, O2+ N2O (40-60) % mixture and IV atracurium 0.5 mg/kg bolus and then 0.1 mg/kg maintenance doses monitored on peripheral nerve stimulator. Inhalational agents were stopped and 100% oxygen was administered at the end of the surgery. Neuromuscular block was reversed. Oral suction was done under gentle direct laryngoscopy. After gaining consciousness the cuff was deflated and patients were extubated. Patients were shifted to postoperative ward with head up position and oxygen support through facemask.
Assessment of patients were done for POST, HOV, cough at 1,2,4 and 24 hours postextubation. Patients were assessed as per the four point scale (0-3) grading system [Table/Fig-2,3 and 4] [13].
Postoperative Sore Throat (POST) grading.
| Grade | Description |
|---|
| 0 | No sore throat |
| 1 | Mild (less than what is seen in common cold) |
| 2 | Moderate (like what is seen in common cold) |
| 3 | Severe (more than what is seen in common cold) |
Hoarseness of Voice (HOV) grading.
| Grade | Description |
|---|
| 0 | No hoarseness |
| 1 | Mild (no hoarseness at the time of interview but had it previously) |
| 2 | Moderate (like what is seen in common cold) |
| 3 | Severe (recognisable at the time of interview) |
| Grade | Description |
|---|
| 0 | No cough |
| 1 | Mild (less than what is seen in common cold) |
| 2 | Moderate (like what is seen in common cold) |
| 3 | Severe (more than what is seen in common cold) |
Statistical Analysis
Unpaired t-test was performed for statistical analysis. Results was considered statistically significant, if p-value was <0.05. The software used was Microsoft excel version 2012.
Results
[Table/Fig-5] shows the baseline characteristics of the study population. There was no significant difference observed amongst both the groups.
| Variables | Number of patients (N=50) | p-value |
|---|
| Group K {N=25 (%)} | Group C {N=25 (%)} |
|---|
| Age (Years) |
| 18-35 | 17 (68%) | 15 (60%) | 0.28 |
| 36-55 | 8 (32%) | 10 (40%) |
| Mean±SD | 32.76±8.24 | 32.72±9.43 | 0.77 |
| Gender |
| Male | 14 (56%) | 8 (32%) | 0.13 |
| Female | 11 (44%) | 17 (68%) |
| ASA grade |
| I | 16 (64%) | 12 (48%) | 0.13 |
| II | 9 (36%) | 13 (52%) |
Clinical Outcome Analysis
Three categorical outcomes were considered for analysis with reference to their timeframe of occurrence.
POST: No statistical significance was observed four and 24 hours onwards in terms of POST grading in both K and C group. However, in the beginning and at two hours, there were significant differences in observation of the POST grading [Table/Fig-6].
Clinical outcome of POST.
| Grading of discomfort | 1 hours | 2 hours | 4 hours | 24 hours |
|---|
| K, n (%) | C, n (%) | K, n (%) | C, n (%) | K, n (%) | C, n (%) | K, n (%) | C, n (%) |
|---|
| 0 | 25 (100) | 14 (56) | 25 (100) | 14 (56) | 20 (80) | 15 (60) | 13 (52) | 15 (60) |
| 1 | 0 | 8 (32) | 0 | 8 (32) | 5 (20) | 7 (28) | 11 (44) | 7 (28) |
| 2 | 0 | 3 (12) | 0 | 3 (12) | 0 | 3 (12) | 1 (4) | 3 (12) |
| Total number of patients having POST | 0 | 11 (44) | 0 | 11 (44) | 5 (20) | 10 (40) | 12 (48) | 10 (40) |
| p-value | <0.05 | <0.05 | 0.132 | 0.362 |
HOV: There was significant difference observed in the severity of HOV till 4 hours in group K and group C. It shows that ideal time duration to reduce voice quality issues with the drug was 4 hours [Table/Fig-7].
| Grading of discomfort | 1 hours | 2 hours | 4 hours | 24 hours |
|---|
| K, n (%) | C, n (%) | K, n (%) | C, n (%) | K, n (%) | C, n (%) | K, n (%) | C, n (%) |
|---|
| 0 | 25 (100) | 11 (44) | 24 (96) | 11 (44) | 20 (80) | 12 (48) | 13 (52) | 12 (48) |
| 1 | 0 | 10 (40) | 1 (4) | 10 (40) | 5 (20) | 10 (40) | 11 (44) | 10 (20) |
| 2 | 0 | 4 (16) | 0 | 4 (16) | 0 | 3 (12) | 1 (4) | 3 (12) |
| Total number of patients having POST | 0 | 14 (56) | 1 | 14 (56) | 5 (20) | 13 (52) | 12 (48) | 13 (32) |
| p-value | <0.05 | <0.05 | 0.035 | 0.585 |
Cough: It was observed that at four and 24 hour postsurgery, no drug was found to produce significant difference in terms of resolution of the coughing issues [Table/Fig-8].
Clinical outcome of cough.
| Grading of discomfort | 1 hours | 2 hours | 4 hours | 24 hours |
|---|
| K, n (%) | C, n (%) | K, n (%) | C, n (%) | K, n (%) | C, n (%) | K, n (%) | C, n (%) |
|---|
| 0 | 25 (100) | 14 (56) | 25 (100) | 14 (56) | 20 (80) | 15 (60) | 13 (52) | 15 (60) |
| 1 | 0 | 8 (32) | 0 | 8 (32) | 5 (20) | 10 (40) | 11 (44) | 7 (28) |
| 2 | 0 | 3 (12) | 0 | 3 (12) | 0 | 3 (12) | 1 (4) | 3 (12) |
| Total no of patients having POST | 0 | 11 (44) | 0 | 11 (44) | 5 (20) | 10 (40) | 12 (48) | 10 (40) |
| p-value | <0.05 | <0.05 | 0.132 | 0.362 |
Discussion
This study was carried out to observe the effect of ketamine gargles on POST, HOV and cough following endotracheal intubation in patients undergoing surgeries under general anaesthesia. Unlike other studies the patients in this study were not posted for a specific type of surgery but lasting for not more than 90 minutes.
Dose of ketamine employed and administration: All the studies showed attenuation of POST after ketamine gargle. The researchers [3,7,13,16-20] used a dose range of 40-50 mg of ketamine with 29 mL of normal saline and 30 mL of normal saline in control group as oral rinse prior to intubation [Table/Fig-9]. Thus, looking at the doses of ketamine gargles in this study the dose was comparable.
Comparision of various studies employing ketamine gargles.
| Sr. No. | Author and type of study | Study population | Type of surgery | Doses of ketamine used | Post grading scale | POST interval (Hour) |
|---|
| 1 | Rudra et al., [7]Prospective, randomised, placebo-controlled, single blinded study | 40Group C (Control): 20 Group K (Ketamine): 20 | Abdominal and pelvic surgeries | Ketamine 50 mg in 29 mL drinking waterGargling for 40 seconds | # | 4, 8, 24 |
| 2 | Lalwani J et al., [13]Prospective, randomised, placebo-controlled, single blinded study | 100Group C: 50Group K: 50 | Not specified | Ketamine 50 mg in 29 mL drinking waterGargling for 30 seconds | * | 0, 2, 4, 24 |
| 3 | Canbay O et al., [16]Prospective, randomised, controlled, single blinded study | 46Group C (Control): 23 Group K (Ketamine): 20 | Septorhinoplasty | Ketamine 40 mg in 30 mL salineGargling for 30 seconds | # | 0, 2, 4, 24 |
| 4 | Kamble N et al., [18]Prospective randomised double blinded study | 60Group 1 K (Ketamine): 30Group 2 C (Control): 30 | Abdominal and pelvic surgeries | Ketamine 50 mg in 29 mL distilled water | # | 0, 4, 8, 24 |
| 5 | Chan L et al., [19]Prospective double blind randomised control study | 44Group C (control): 22 Group K (Ketamine): 22 | Gynaecological surgeries | Ketamine 40 mg in 20 mL salineGargling for 30 seconds | # | 0, 2, 24 |
| 6 | Shrestha SK et al., [20]Prospective comparative study | 40Group C (Control): 20 Group K (Ketamine): 20 | Abdominal and orthopedic surgeries | Ketamine 50 mg in 30 mL drinking waterGargling for 30 seconds | # | 4, 8, 24 |
| 7 | Present study | 50GroupC (Control): 25K (Ketamine): 25 | Not specific | Ketamine 50 mg in 29 mL 0.9% normal salineGargling for 30 seconds | # | 1,2,4,24 |
#Four point scale (0-3) 0: No sore throat; 1: Mild sore throat (complains of sore throat only on asking); 2: Moderate sore throat (complains of sore throat on his/her own; 3: Severe sore throat (Change of voice or hoarseness, associated with throat pain); *0: No sore throat; 1: Mild (less than what is seen in common cold); 2: Moderate (like what is seen in common cold); 3: Severe (more than what is seen in common cold).
Patients were intubated with high volume low pressure cuffed polyvinyl chloride ETT of 7.0-7.5 mm ID (in females) and 8.0-8.5 mm ID (in males). The cuff was inflated till the disappearing of the air leak from trachea [17-20].
In this study, a four-point scale (0-3) [13] was used. Other studies used similar scales and have been tabulated in [Table/Fig-9]. POST, HOV and cough were assessed at 1 hour after arrival at the post anesthetic care unit at 2, 4 and 24 hours later.
In present study, the incidence of POST was significantly reduced at 1 and 2 hours in group K compared to group C postoperatively, the results were similar to the study conducted by Chan L et al., [19]. In contrast to the present study Rudra A et al., Lalwani J et al., Canbay O et al., Kamble N et al., and Shrestha SK et al., observed that incidence of POST was less in ketamine group as compared to control group upto 24 hours [Table/Fig-6,9] [7,13,16,18,20].
In present study the incidence of hoarseness in group C was higher compared to group K at one, two, four hours. In contrast Lalwani J et al., found that HOV was less in ketamine group upto 24 hours [Table/Fig-7,9] [13]. Incidence of cough in present study was higher in group C compared to group K at 1 and 2 hours. In contrast Lalwani J et al., observed that incidence of cough was significantly less in ketamine group upto 24 hours [Table/Fig-8,9] [13]. It was concluded that gargles with ketamine decreased the incidence of severity of POST, HOV and cough.
Sore throat due to endotracheal intubation can manifest by local trauma with instrumentation, oedema, pain, congestion leading to inflammation of pharyngeal mucosa. Ketamine gargle can be the reason for the reduction of inflammation and help in decreasing the incidence of POST [11-13]. There is a growing amount of experimental data on NMDA receptors present in peripheral nerves where the peripherally applicated NMDA receptor antagonists are studied for antinociception [13-15].
Though similar studies were carried out in the past it is not a common practice in routine surgeries prior to intubation. But the present study shows the benefits of such inexpensive and easily applicable procedure to reduce the incidence of POST, HOV and cough which are small yet neglected factors in view of patients’ comfort in immediate postoperative period.
Limitation(s)
Absence of the measurement of plasma levels of ketamine. Reduction of the inflammation by ketamine gargling may be the reason for decrease in POST, HOV and cough in the present study. However, a peripheral and central action following systemic absorption cannot be ignored.
Conclusion(s)
Ketamine gargles given in a dose of 50 mg in 29 mL of 0.9% normal saline significantly reduces the incidence of POST and cough upto 2 hours and HOV upto 4 hours in immediate postoperative period after extubation. It is a fairly easy, accessible, not expensive and applicable procedure.
#Four point scale (0-3) 0: No sore throat; 1: Mild sore throat (complains of sore throat only on asking); 2: Moderate sore throat (complains of sore throat on his/her own; 3: Severe sore throat (Change of voice or hoarseness, associated with throat pain); *0: No sore throat; 1: Mild (less than what is seen in common cold); 2: Moderate (like what is seen in common cold); 3: Severe (more than what is seen in common cold).