Multilocular Thymic Cyst in a Patient with Diffuse Infiltrative Lymphocytosis Syndrome
Nitin Gupta1, Anivita Aggarwal2, Madhavi Tripathi3, Sundeep Malla4, Neeraj Nischal5
1 Senior Resident, Department of Medicine, All India Institute of Medical Sciences, New Delhi, India.
2 Senior Resident, Department of Medicine, All India Institute of Medical Sciences, New Delhi, India.
3 Professor, Department of Nuclear Medicine, All India Institute of Medical Sciences, New Delhi, India.
4 Senior Resident, Department of Radiodiagnosis, All India Institute of Medical Sciences, New Delhi, India.
5 Associate Professor, Department of Medicine, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Neeraj Nischal, Department of Medicine, Teaching Block, 3rd Floor, AIIMS, New Delhi, India.
E-mail: neerajnischal@gmail.com
Diffuse Infiltrative Lymphocytosis Syndrome (DILS) is a multisystem disorder characterised by bilateral salivary gland enlargement and/or xerostomia in patients with Human Immunodeficiency Virus (HIV) infection. A 16-year-old young male patient, presented with bilateral painless parotid swelling since five years. On evaluation, patient was found to have oral thrush and bilateral cervical lymphadenopathy. He turned out to be positive for HIV with a cluster of differentiation 4 (CD4) count of 237/mcl. On Positron Emission Tomography- Contrast Tomography (PET-CT), a multiloculated thymic cyst (13×9×6 cm) was noted. He was diagnosed to have DILS with a large multiloculated thymic cyst. The patient was managed with tenofovir, lamivudine and efavirenz along with cotrimoxazole prophylaxis and fluconazole and was followed uptil nine months for the regress of the conditions. The case highlights the rare association between DILS and thymic cyst.
Human immunodeficiency virus, Parotid, Thymus multisystem disorders
Case Report
A 16-year-old male patient presented with bilateral painless parotid and submandibular swelling, slowly increasing in size, since five years. He did not have any history of fever, loss of appetite or loss of weight. His father died early in his childhood and his mother had a history of prolonged illness after which she moved out of the house. He was currently living with his aunt. He had no history of any high-risk behaviour.
On examination, he was found to have whitish patches involving the oral mucosa and palate (candidiasis), enlarged parotid glands of both sides and bilateral cervical lymphadenopathy. The parotid gland openings were not visualised.
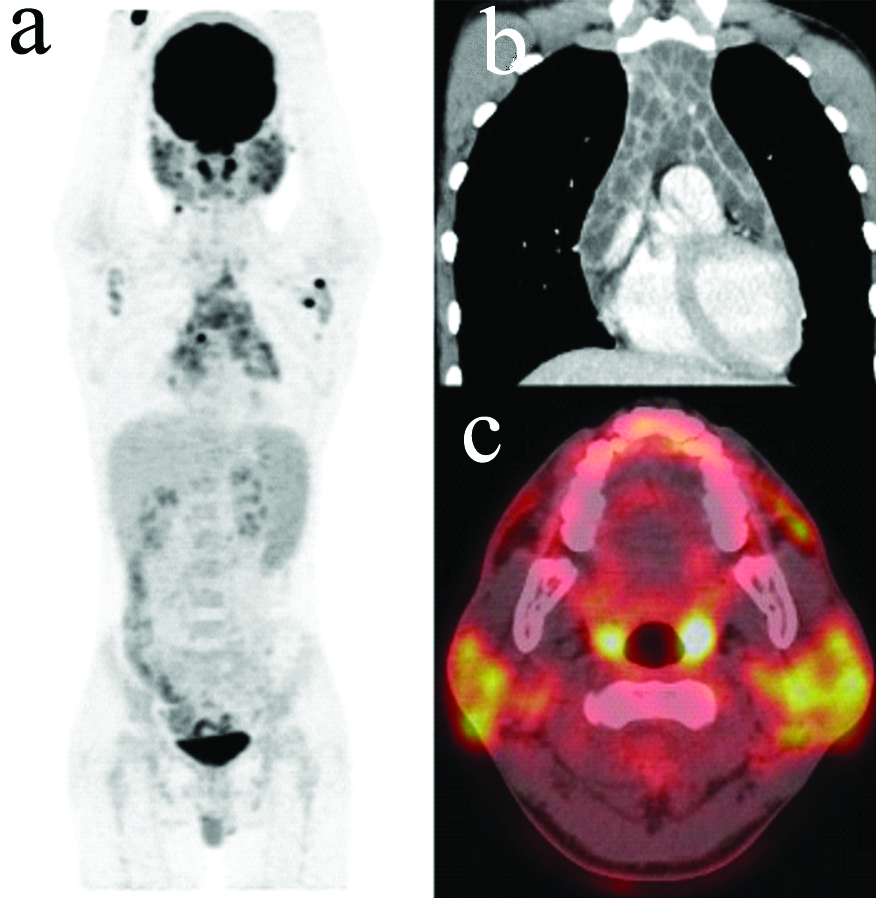
His routine haematological and biochemical parameters were normal except for relative lymphocytosis. Ultrasonography of the neck revealed cervical lymphadenitis with cystic enlargement of bilateral parotid and submandibular glands. He was found to be positive for HIV-1 by serology. His CD4 count was found to be 237/mcl (6%). HIV was initially suspected as he had lymphadenopathy with oral thrush. Also, since both his parents had a history of prolonged illness, vertical transmission was suspected. A biopsy of the left supraclavicular lymph node was done which showed lymphocytic infiltration without any granulomas and was negative for bacterial, fungal (for endemic mycoses) and mycobacterial cultures. Auto-immune profile and Schirmer’s test were negative. On Positron Emission Tomography-Contrast Tomography (PET-CT), a multiloculated thymic cyst (13×9×6 cm) was noted [Table/Fig-1].
(a) Whole body PET showing metabolically active cysts in thymus and parotid along with right cervical, right internal mammary and left axillary lymphadenopathy; (b) Coronal section of thorax showing a multiloculated cystic lesion in anterior mediastinum suggestive of a thymic cyst; (c) Transverse section showing metabolically active cysts in the parotid gland.
The patient was diagnosed with DILS based on the clinical, radiological and histopathological findings. He was initiated on tenofovir, lamivudine and efavirenz along with cotrimoxazole prophylaxis and fluconazole (for oral candidiasis). No active intervention was planned for the thymic cyst as it was asymptomatic and is known to regress spontaneously.
His oral candidiasis improved within a week. Patient did not report any fever on follow-up after three months. His neck swellings had significantly reduced on follow-up after nine months. Repeat imaging could not be performed because of financial constraints. The aunt was counselled about the importance of adherence to medications. The patient was asked to follow-up in the local antiretroviral therapy centre.
Discussion
The Diffuse Infiltrative Lymphocytosis Syndrome (DILS) is a multisystem disorder characterised by bilateral salivary gland enlargement and/or xerostomia for atleast six months in individuals with HIV infection [1]. The diagnosis requires histologic confirmation of lymphocytic infiltration without any evidence of granuloma or neoplasia [1]. DILS can be associated with the involvement of other organs such as lungs, liver, kidney etc. Multilocular thymic cyst as a part of DILS is an extremely rare entity [1-5]. Parotid enlargement and lymphocytic interstitial pneumonia were concurrently present in some of the reported cases [4]. These cysts are usually detected as an incidental finding on radiology [4]. They are located in the anterior mediastinum and can grow up to a maximum of 17-20 centimetres [3]. Their histopathology resembles that of benign lymphoepithelial cysts [6].
Since the patient had HIV, bilateral parotid enlargement and bilateral cervical lymphadenopathy, the following differential diagnoses were kept: tuberculosis, lymphoma, Sjogren’s syndrome and sarcoidosis [7-10]. However, the biopsy of the lymph node showed lymphocytic infiltration without any granulomas, which decreased the possibility of tuberculosis. The negative auto-immune profile and Schirmer’s test pointed against Sjogren’s syndrome [11-13]. To evaluate for sarcoidosis and lymphoma, a PET-CT was done, which showed a multiloculated thymic cyst. Based on the clinical presentation, lymphocytic infiltration and the thymic cyst, a diagnosis of DILS was made.
A thymic cyst is an important differential diagnosis of patients presenting with an anterior mediastinal mass. Thymic cysts may be congenital or acquired. While congenital thymic cysts are usually small and unilocular, acquired cysts are large and multilocular [6]. Similar to this patient, acquired thymic cysts as a part of DILS have been described in young patients with HIV with a slight male preponderance [14]. The clinical course of this DILS has been described as relatively slow, and most cases show an eventual reduction in thymic size. In the series by Kontny HU et al., the size of cyst reduced in five of the eight patients without any surgery while two of the patients showed complete resolution [14]. In asymptomatic HIV positive patients with characteristic cysts and no features suggestive of malignancy, active intervention may not be required. Surgical intervention may be warranted in those with large symptomatic masses [14].
Conclusion(s)
The report presented a newly diagnosed HIV patient with bilateral parotid and submandibular swelling. The clinical presentation was initially thought to be due to opportunistic infection or malignancy, but the patient was later diagnosed with DILS. The PET-CT showed a multilocular thymic cyst which has shown to be a rare manifestation of the same syndrome.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 26, 2020
Manual Googling: Apr 19, 2021
iThenticate Software: Apr 28, 2021 (1%)
[1]. Ghrenassia E, Martis N, Boyer J, Burel-Vandenbos F, Mekinian A, Coppo P, The Diffuse Infiltrative Lymphocytosis Syndrome (DILS). A comprehensive reviewJ Autoimmun 2015 59:19-25.Epub 2015 Feb 710.1016/j.jaut.2015.01.01025660200 [Google Scholar] [CrossRef] [PubMed]
[2]. Tamagno M, Bibas BJ, Bernardi F, Lian YC, Bammann RH, Fernandez A, Giant multilocular thymic cyst in an HIV-infected adolescentJ Pediatr Surg 2011 46(9):1842-45.10.1016/j.jpedsurg.2011.06.00921930000 [Google Scholar] [CrossRef] [PubMed]
[3]. Shi X, Nasseri F, Berger DM, Nachiappan AC, Large multilocular thymic cyst: A rare finding in an HIV positive adult femaleJ Clin Imaging Sci 2012 2:55Epub 2012 Aug 3010.4103/2156-7514.10037923029638 [Google Scholar] [CrossRef] [PubMed]
[4]. Leonidas JC, Berdon WE, Valderrama E, Neveling U, Schuval S, Weiss SJ, Human immunodeficiency virus infection and multilocular thymic cystsRadiology 1996 198(2):377-79.10.1148/radiology.198.2.859683510.1148/radiology.198.2.8596835 [Google Scholar] [CrossRef] [PubMed]
[5]. Chou SH, Prabhu SJ, Crothers K, Stern EJ, Godwin JD, Pipavath SN, Thoracic diseases associated with HIV infection in the era of antiretroviral therapy: Clinical and imaging findingsRadiographics 2014 34(4):895-911.10.1148/rg.34413011525019430 [Google Scholar] [CrossRef] [PubMed]
[6]. Suster S, Rosai J, Multilocular thymic cyst: An acquired reactive process: Study of 18 casesAm J Surg Pathol 1991 15(6):388-98.10.1097/00000478-199104000-000082006719 [Google Scholar] [CrossRef] [PubMed]
[7]. Elyamany G, Fouly A, Alqahtani A, Alrumeh A, Asiri S, Faifi SA, Cytological diagnosis of plasmablastic lymphoma involving the parotid gland: A case report with review of the literatureCase Rep Oncol 2021 14(1):244-48.10.1159/00050974633776711 [Google Scholar] [CrossRef] [PubMed]
[8]. Saha D, Tapadia R, Lobo FD, Dhavalpure N, Swamy M, Murali N, Lymphoepithelial sialadenitis involving HIV-infected and sjogren syndrome patients: A cytologic studyIndian J Otolaryngol Head Neck Surg 2019 71(2):176-81.10.1007/s12070-017-1066-931275826 [Google Scholar] [CrossRef] [PubMed]
[9]. Gupta N, Aggarwal A, Tripathi M, Nischal N, Parotid gland tuberculosisQJM: An International Journal of Medicine 2020 113(7):500-01.10.1093/qjmed/hcz26631613366 [Google Scholar] [CrossRef] [PubMed]
[10]. Pijpe J, Kalk WW, Bootsma H, van der Wal JE, van Imhoff GW, Vissink A, Bilaterale zwelling van de glandulae parotideae als onderdeel van een systeemziekte [Bilateral swelling of the parotid glands as part of a systemic disease]Ned Tijdschr Geneeskd 2003 147(47):2309-15. [Google Scholar]
[11]. Thorne I, Sutcliffe N, Sjögren’s syndromeBr J Hosp Med (Lond) 2017 78(8):438-42.10.12968/hmed.2017.78.8.43828783408 [Google Scholar] [CrossRef] [PubMed]
[12]. Witte T, Sjögren-Syndrom [Sjögren’s syndrome]Z Rheumatol 2019 78(6):511-17.German10.1007/s00393-019-0625-830937527 [Google Scholar] [CrossRef] [PubMed]
[13]. Ramos-Casals M, Brito-Zerón P, Sisó-Almirall A, Bosch X, Primary Sjogren syndromeBMJ 2012 344:e382110.1136/bmj.e382122700787 [Google Scholar] [CrossRef] [PubMed]
[14]. Kontny HU, Sleasman JW, Kingma DW, Jaffe ES, Avila NA, Pizzo PA, Multilocular thymic cysts in children with human immunodeficiency virus infection: Clinical and pathologic aspectsJ Pediatr 1997 131(2):264-70.10.1016/S0022-3476(97)70164-1 [Google Scholar] [CrossRef]