Monoblastic Sarcoma- A Rare Case Report of Myeloid Sarcoma Variant
Nupur Kaushik1, Lalit Kumar2, Pooja Agarwal3, Harendra Kumar4, Brijesh Sharma5
1 Junior Resident, Department of Pathology, Sarojini Naidu Medical College, Agra, Uttar Pradesh, India.
2 Junior Resident, Department of Pathology, Sarojini Naidu Medical College, Agra, Uttar Pradesh, India.
3 Professor, Department of Pathology, Sarojini Naidu Medical College, Agra, Uttar Pradesh, India.
4 Associate Professor, Department of Pathology, Sarojini Naidu Medical College, Agra, Uttar Pradesh, India.
5 Assistant Professor, Department of Orthopaedics, Sarojini Naidu Medical College, Agra, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Harendra Kumar, Associate Professor, Department of Pathology, Sarojini Naidu Medical College, Agra, Uttar Pradesh, India.
E-mail: dr_haren@yahoo.co.in
Myeloid sarcoma also known as chloroma, granulocytic sarcoma, extramedullary Acute Myeloid Leukaemia (AML), myeloblastoma or extramedullary myeloid tumour is a rare manifestation, characterised by the proliferation of immature myeloid cells, myeloblasts or monoblasts occurring as one or more tumour at an extramedullary site. It is associated with disruption of normal architecture of tissue in which it is found. Monoblastic sarcoma is a rare variant of myeloid sarcoma. Hereby, the authors report a case of primary monoblastic sarcoma in a 64-year-old male patient presented with complaint of swelling over right side lower cervical region. He had no history of AML. On physical examination, the swelling was over medial one-third of right clavicle measuring 6×5.8×3 cm. The swelling was excised and sent for histopathological examination, which was diagnosed as monoblastic sarcoma, and confirmed on immunohistochemistry.
Immunohistochemistry, Monoblasts, Monoblastic variant
Case Report
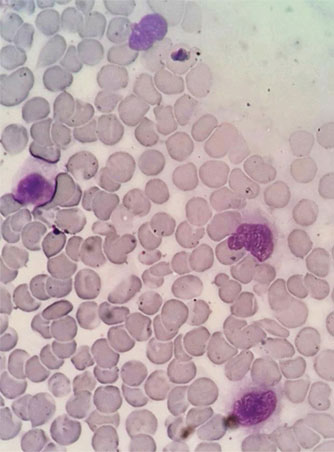
A 64-year-old male presented with chief complaint of swelling over right side lower cervical region since one and half year. There was no significant past history. The swelling was gradual in onset and progressively increasing in size. On physical examination, the swelling was over medial right clavicular region, measuring 6×5.8×3 cm. The swelling was non tender, soft to firm in consistency. Complete Blood Count (CBC) and Peripheral Blood Smear (PBS) were within normal limit. On Fine Needle Aspiration Cytology (FNAC), the smear examined revealed cellular smear comprising of discohesive cluster and singly dispersed monomorphic cell population in haemorrhagic background. The cells had minimal pleomorphism, slightly indented or clefted nuclei, fine chromatin, occasionally prominent nucleoli and moderate basophilic cytoplasm with well-defined outline [Table/Fig-1]. On the basis of these findings, differential diagnosis of myeloid sarcoma and malignant lymphoma was made and histopathological examination was advised.
Showing low cellularity with singly dispersed tumour cells in haemorrhagic background, cells having moderate amount of cytoplasm indented nuclei with clumped chromatin and conspicuous nucleoli in few cells; suggestive of Myeloid Sarcoma variant (May Grunwald Giemsa (MGG) stain, 1000X).
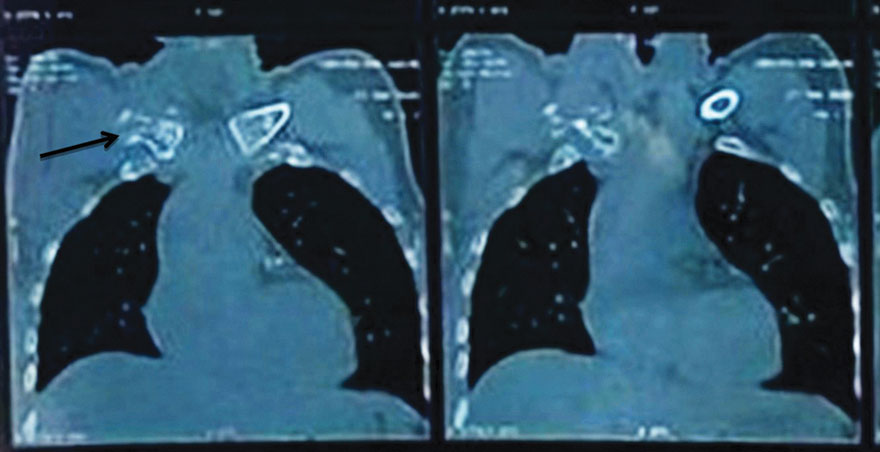
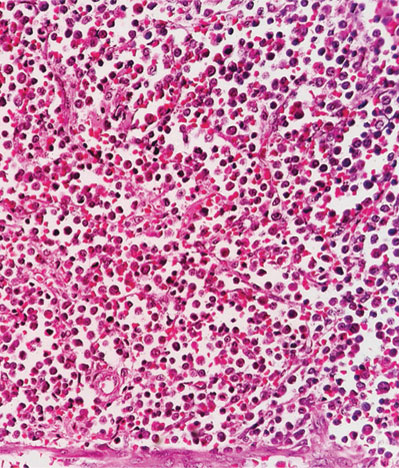
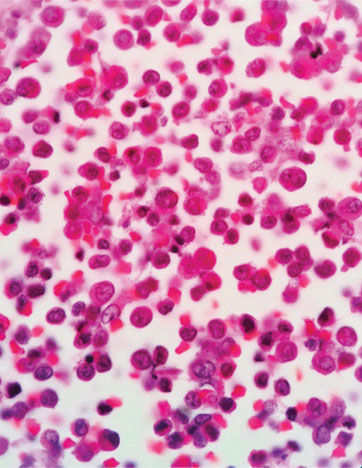
Magnetic Resonance Imaging (MRI) right clavicle with contrast revealed a hetero-signal intensity destructive bony lesion involving medial aspect of right clavicle measuring 5.2×5.4×5.6 cm intermingled multiple small calcifications [Table/Fig-2]. The swelling was excised and sent for histopathological examination. On gross examination, the specimen revealed one firm reddish grey globular piece of tissue with attached piece of bone. The tissue was measuring 6.7×6.8×3 cm and bone measuring 7 cm in length and diameter varied from 1-4 cm with eroded bony surface [Table/Fig-3]. On histopathological examination, the sections examined revealed highly cellular tumour comprising of mononuclear cells arranged in sheets. The cells were medium to large in size with moderate eosinophilic cytoplasm, round to oval nuclei with fine stranded chromatin and conspicuous nucleoli in most of cells [Table/Fig-4,5].
Showing hetero-signal intensity destructive bony lesion involving medial aspect of right clavicle with intermingled multiple small calcifications.
Showing cut surface of gross specimen with reddish grey globular piece of tissue along with attached bone.

Showing mononuclear cells arranged in sheets. The tumour cells are medium to large with moderate eosinophilic cytoplasm and fine chromatin; Monoblastic sarcoma (H&E, 400X).
Showing mononuclear cells arranged in sheets. The tumour cells are medium to large with moderate eosinophilic cytoplasm and fine chromatin; Monoblastic sarcoma (H&E, 1000X).
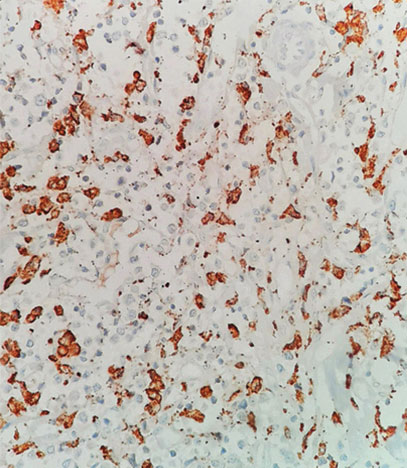
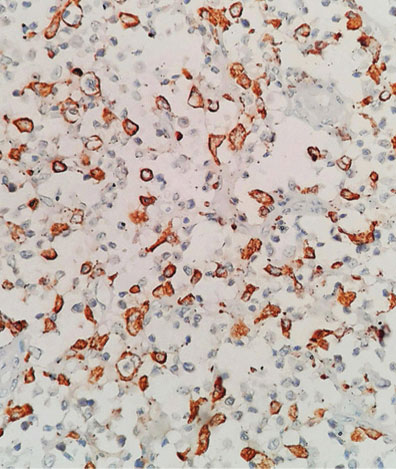
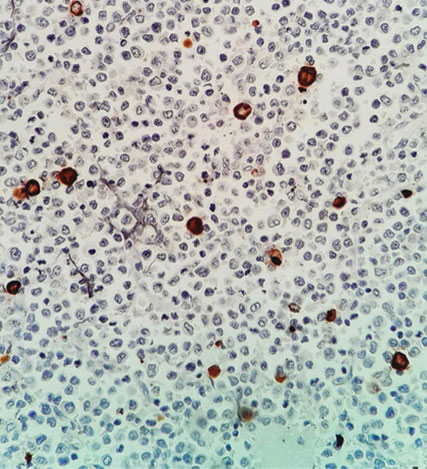
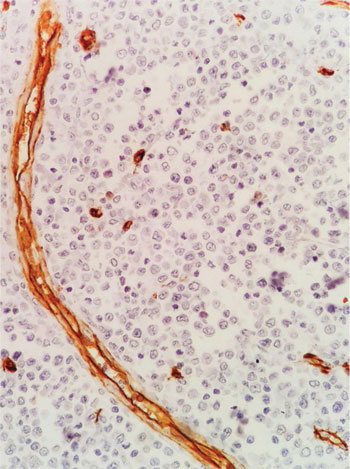
On histological examination, the diagnosis of monoblastic sarcoma was made with the differential of Non-Hodgkin Lymphoma (NHL) and small round cell tumour. On Immunohistochemistry (IHC), the tumour was found CD68 Phosphoglucomutase 1 (PGM1) [Table/Fig-6], CD163 [Table/Fig-7] positive and scattered Myeloperoxidase (MPO) [Table/Fig-8] positivity and negative for CD34 [Table/Fig-9]. On the basis of IHC, the diagnosis of monoblastic sarcoma was confirmed. After surgery and IHC confirmation of diagnosis, the patient was referred to Radiotherapy Department for further treatment. Patient received 25 cycles of radiotherapy followed by six cycles of chemotherapy along with symptomatic treatment. Now patient is on regular follow-up and doing well. Last follow-up was done on1st April, 2021.
Discussion
Granulocytic sarcoma was first described by Burns in 1811 and in 1853 King gave name chloroma while renamed in 1966 by Rappaport as Granulocytic sarcoma. It has an estimated incidence of 0.7 per million children and two per million adults [1]. It can occur in any age and can involve any anatomical site throughout the body [2]. Myeloid sarcoma may develop de novo or simultaneously with systemic bone marrow leukaemia which is known as secondary myeloid sarcoma. Myeloid sarcoma occurring in absence of a history of leukaemia, myelodysplastic syndrome, myeloproliferative neoplasm and without bone marrow involvement, is termed as primary myeloid sarcoma [3]. Monoblastic sarcoma is a rare variant of myeloid sarcoma comprising of more than 80% monoblasts [4]. Myeloid sarcoma is a neoplasm present at any extramedullary sites and comprising of immature granulocytes, monocytes, or both [5]. Initially, described as chloroma due to green coloured appearance on exposed to air, which occur due to the presence of MPO in the tumour cells. Because the greenish colour is not a consistent finding and proven granulocytic origin, so the terms granulocytic sarcoma or myeloid sarcoma are preferably used by most of the authors.
On the basis of different site involvement, such as soft tissues, skin, bones, lymph nodes; the patients present with various clinical presentation [6]. Myeloid sarcomas may be found in one of four settings [7]: 1) The active phase of the disease in patients with known AML; 2) The myeloid sarcoma may be the first manifestation of blastic transformation of chronic myeloproliferative disorder and myelodysplastic syndrome; 3) Relapse as the first manifestation in patients previously treated for primary or secondary acute leukaemia; 4) De novo in healthy subjects, in whom typical form of AML occurs after an interval of weeks to years. Myeloid sarcoma has been reported from one month to 89 years with male preponderance with maximum number of cases in their last decade of life [8]. Myeloid sarcoma is often misdiagnosed as NHL in approximately 46% of patients, with other differential diagnosis including, Ewing’s sarcoma, extramedullary hematopoiesis, malignant mastocytosis with atypical mast cells and malignant histiocytosis. The definitive diagnosis of granulocytic sarcoma is usually based on immunohistochemistry and/or immunophenotyping [9]. On the basis of extensive morphological and immunohistochemical analyses, the myeloid sarcomas are classified into five types [5]: i) immature granulocytic sarcoma; ii) differentiated granulocytic sarcoma; iii) monoblastic sarcoma; iv) monocytic sarcoma; and v) myelomonocytic sarcoma. Microscopically monoblastic sarcomas are composed of a large population (>80%) of monoblasts.
The large sized neoplastic cells with abundant eosinophilic cytoplasm, round/oval nuclei with dispersed chromatin and one or multiple prominent nucleoli are strongly positive for CD43, lysozyme, CD68, CD163, while weakly positive for CD4, and negative for CD34 [6]. Cytochemical stain such as Myeloperoxidase (MPO) and lysozyme helps in definitive diagnosis. MPO is positive in most myeloblastic variants, while lysozyme is frequently expressed in monoblastic variants. Megakaryoblastic cells characteristically express factor VIII, CD61, and CD31 while Glycophorin C and/or blood group proteins are usually expressed in the rare erythroblastic variant [10]. Immunohistochemical study plays an essential role in obtaining a correct diagnosis of monoblastic sarcoma. MPO immunopositivity is specific for granulocytic differentiation, while CD68 (PGM1)-positivity indicate monocytic differentiation without any symptom of leukaemia. The most sensitive markers for myeloid differentiation are MPO and CD117, while monocytic precursors are most strongly expressed by CD68 [5]. In our case, photomicrographs demonstrated positive immunohistochemical staining for CD68, CD163, and with scattered positivity for MPO, and negative for CD34 [Table/Fig-6,8 and 9].
Showing CD68 PGM1 cytoplasmic granular positivity (IHC, 400X).
Showing CD163 cytoplasmic granular positivity (IHC, 400X).
Showing MPO scattered positivity in occasional tumour cells (IHC, 400X).
Showing CD34 negative tumour cells with blood vessels positivity-internal control (IHC, 400X).
The treatment recommended for isolated monoblastic sarcoma or myeloid sarcoma and myeloid sarcoma occurring in AML patients is AML type chemotherapy. Better overall survival in patients presenting with myeloid sarcoma with or without concomitant AML, shown to be associated with haematopoietic stem cell transplantation. In case of monoblastic sarcoma prompt diagnosis and initiation of chemotherapy as early as possible prevents distant spread to other organs [8,11].
Conclusion(s)
Myeloid sarcoma is an uncommon entity and monoblastic sarcoma is one of its rare variant. Histopathological examination and IHC is required for confirming the diagnosis.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 12, 2021
Manual Googling: Apr 10, 2021
iThenticate Software: Apr 28, 2021 (19%)
[1]. Mehta DP, Trivedi P, Anand AS, Parikh S, Chirmade P, Primary intracranial granulocytic sarcoma: A case report and review of literatureJ NTR Univ Health Sci 2017 6:169-73.10.4103/JDRNTRUHS.JDRNTRUHS_42_17 [Google Scholar] [CrossRef]
[2]. De Andrade BAB, Farneze RB, Agostini M, Cortezzi EB, Abrahao AC, Cabral MG, Myeloid sarcoma of the oral cavity: A case report and review of 89 cases from the literatureJ Clin Exp Dent 2017 9(9):1167-71.10.4317/jced.5393529075423 [Google Scholar] [CrossRef] [PubMed]
[3]. Nguyen R, Sayar H, Primary myeloid sarcoma of the prostate: A case report and literature reviewCase Report in Hematol 2018 2018:360429810.1155/2018/360429829854498 [Google Scholar] [CrossRef] [PubMed]
[4]. Alexiev BA, Wang W, Ning Y, Chumsri S, Gojo I, Rodgers WH, Myeloid sarcomas: A histologic, immunohistochemical and cytogenetic studyDiagn Pathol 2007 2:4210.1186/1746-1596-2-4217974004 [Google Scholar] [CrossRef] [PubMed]
[5]. Yin Q, Chen D, Chen J, Wei X, Guan J, Spinal monocytic sarcoma presenting as an acute cord compression without any symptom of leukaemic disease: One case report and literature reviewChin J Clin Oncol 2008 5:465-67.10.1007/s11805-008-0465-9 [Google Scholar] [CrossRef]
[6]. Alpeshkumar K, Mitul M, Harsha P, Priti T, Nirmal L, Sonia P, Monoblastic sarcoma/Myeloid sarcoma of paraspinal region as acute paraparesis in aleukemic patient- A rare case report from western IndiaGujarat Cancer Society Research Journal 2016 18(2):38-40. [Google Scholar]
[7]. Audouin J, Comperat E, Le Tourneau A, Camilleri-Broet S, Adida C, Molina T, Myeloid sarcoma: Clinical and morphologic criteria useful for diagnosisInt J Surg Pathol 2003 1(1):271-82.10.1177/10668969030110040414615822 [Google Scholar] [CrossRef] [PubMed]
[8]. Wijesinghe HD, Asanthi NJ, Sooriyaarachchi SANT, Dissanayake K, Fernando J, Monoblasticsarcoma- A rare variant of myeloid sarcoma presenting as a supra orbital mass in an infantJournal of Diagnostic Pathology 2016 11:38-41.10.4038/jdp.v11i1.7694 [Google Scholar] [CrossRef]
[9]. Bakst RL, Tallman MS, Douer D, Yahalom J, How I treat extramedullary acute myeloid leukemiaBlood 2011 118:3785-93.10.1182/blood-2011-04-34722921795742 [Google Scholar] [CrossRef] [PubMed]
[10]. Zhang PJ, Barcos M, Stewart CC, Block AW, Sait S, Brooks JJ, Immunoreactivity of MIC2 (CD99) in acute myelogenous leukemia and related diseaseMod Pathol 2000 13:452-58.10.1038/modpathol.388007710786814 [Google Scholar] [CrossRef] [PubMed]
[11]. Magdy M, Abdel Karim N, Eldessouki I, Gaber O, Rahouma M, Ghareeb M, Myeloid SarcomaOncol Res Treat 2019 42(4):224-29.10.1159/00049721030840960 [Google Scholar] [CrossRef] [PubMed]