Haemorrhagic Retinopathy Associated with Zieve Syndrome
Sadafnaz Sabah1, Abdul Waris2, Mohd Rameez Reza3, Syed Asghar Rizvi4
1 Junior Resident, Department of Ophthalmology, Jawaharlal Nehru Medical College and Hospital, AMU, Aligarh, Uttar Pradesh, India.
2 Assistant Professor, Department of Ophthalmology, Jawaharlal Nehru Medical College and Hospital, AMU, Aligarh, Uttar Pradesh, India.
3 IOL Fellow, Department of Ophthalmology, Shroff Charity Eye Hospital, Kishanganj, Bihar, India.
4 Junior Resident, Department of Ophthalmology, Jawaharlal Nehru Medical College and Hospital, AMU, Aligarh, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abdul Waris, Assistant Professor, Department of Ophthalmology, Aligarh Muslim University, Institute of Ophthalmology, Jawaharlal Nehru Medical College and Hospital, Aligarh-202002, Uttar Pradesh, India.
E-mail: awaris.io@amu.ac.in
Zieve syndrome, a rarely reported case is a triad of jaundice, haemolytic anaemia and hyperlipidaemia that develops secondary to alcohol-induced liver injury. Here in, a case of a 23-year-old young male with history of steatohepatitis is reported who presented with diminution of vision in both eyes. On fundoscopy, there were extensive retinal haemorrhages involving fovea. Workup was consistent with haemolytic anaemia with no source of active bleeding. The patient was managed with supportive treatment. No specific ocular treatment was given. However, the vision gradually improved during follow-up. A rare association of Zieve syndrome with haemorrhagic retinopathy is described here. Moreover, Zieve syndrome has been described in the literature, mostly in non-English language case studies and is still under-recognised and under-reported. Diagnosis should be made quickly to avoid unnecessary invasive diagnostic interventions.
Anaemia, Haemolytic anaemia, Hyperlipidaemia
Case Report
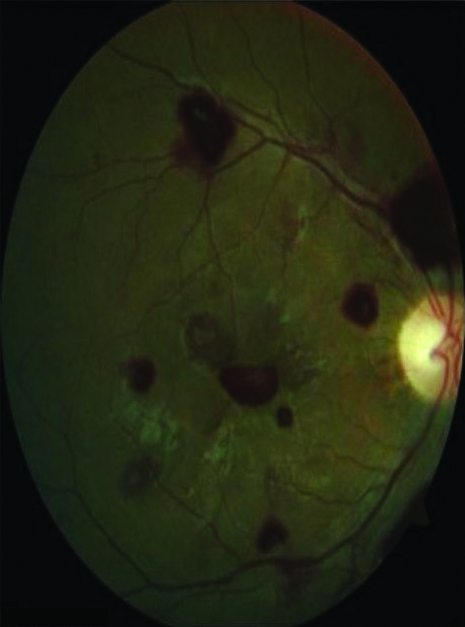
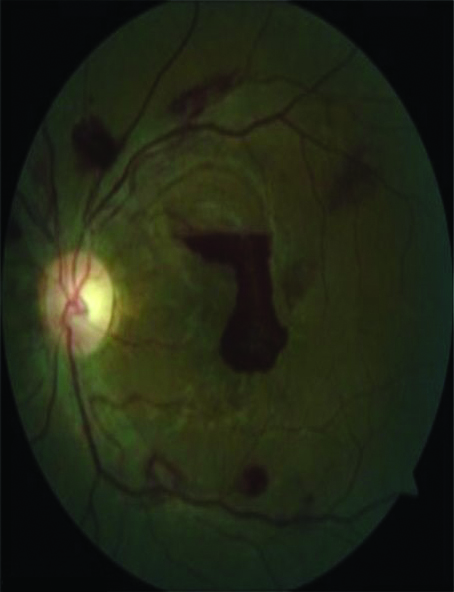
A 23-year-old young boy presented with sudden painless diminution of vision in both eyes. At the time of presentation, his visual acuity was 6/12 in Oculus Dextrus (OD) and 6/60 in Oculus Sinister (OS) [Table/Fig-1,2]. The anterior segment findings were normal in both eyes. However, dilated fundoscopy showed numerous preretinal haemorrhages extending from posterior pole to mid-peripheral retina involving fovea in OD [Table/Fig-1] and OS [Table/Fig-2]. The patient has been a heavy drinker for the past ten years, consuming about 60-80 mL of alcohol every day. He examined earlier in the day by his primary care physician for steatohepatitis as he had been suffering from nausea and vomiting constantly. Other associated symptoms included mild fever and jaundice for which he consulted private practitioner and investigations were done which revealed anaemia. The therapy consisted of two units of packed red blood cells. No other pathological history of interest was elicited such as metabolic disease, spectacle usage, radiation exposure, ocular surgery, head trauma, drug intake, headache, nausea, chills, rigour, weight loss, lymphadenopathy, itching, melena, haematemesis or any other medical conditions such as leukaemia. There was no such complaints in other family members.
Dilated fundoscopy at the time of presentation (OD).
OD: Oculus dextrus
Dilated fundoscopy at the time of presentation (OS).
OS: Oculus sinister
Lab examination was noted for hyperbilirubinaemia (3.8 mg/dL; reference range 0.1-1.2), with increased activity of liver enzymes: alanine tranaminase- 88 IU/L (reference range: 10-28 IU/L); aspartate transaminase- 140 IU/L (reference range: 9-36 IU/L); alkaline phosphatase- 319 IU/L (reference range: 40-141 IU/L); gamma glutamyl transpeptidase level was increased {346 IU/L (reference range: 9-48 IU/L)}. The lipid panel was significant for triglycerides of 428 mg/dL (normal <150 mg/dL) and total cholesterol of 320 mg/dL (normal <170 mg/dL). Abdominal ultrasound showed hepatomegaly. The prothrombin and activated partial prothrombin times and international normalised ratio were impaired. Also, there was decreased haemoglobin level (3.8 gm/dL), thrombocytopaenia (80,000/microlitre of blood). Blood picture revealed reticulocytosis {14% (reference range: 0.5-1.5%)} and anisocytosis with tear drop cells and few fragmented red blood cells. Mean corpuscular volume was 92 fL per cell; (reference range: 80-96 fL per cell). Serum lactate dehydrogenase was increased (440 IU/L). Coomb test was negative.
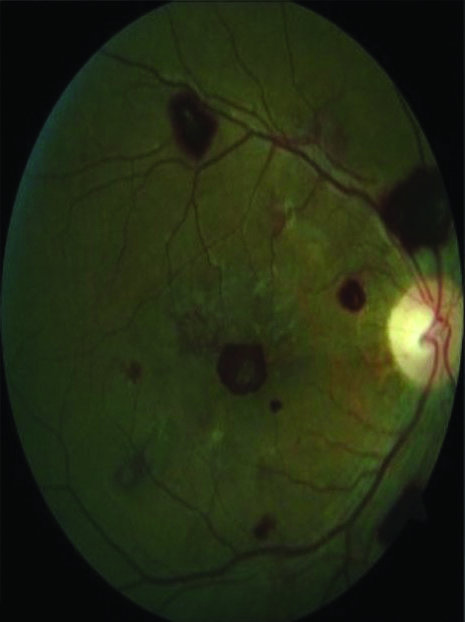
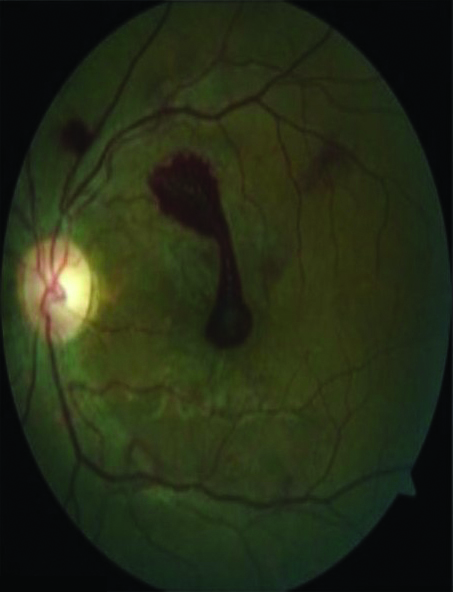
The patient was managed conservatively. No specific treatment was given except for steatohepatitis and denial for alcohol intake. Coagulopathy, anaemia, hyperbilirubinaemia improved rapidly during the treatment. The follow-up examination after two weeks revealed improvement in vision i.e., 6/12 in OD and 6/36 in OS. However, the fundoscopy still showed extensive haemorrhages involving fovea in OD [Table/Fig-3] and OS [Table/Fig-4] but had decreased from before.
Dilated fundoscopy after two weeks of follow-up (OD).
Dilated fundoscopy after two weeks of follow-up (OS).
Discussion
Zieve syndrome, a rarely reported case is characterised by haemolytic anaemia in conjunction with secondary hyperlipidaemia in a patient suffering from alcohol-related toxic liver damage [1]. Hyperlipidaemia in Zieve syndrome can be transitory, as seen in our case. Possible explanations are an episode of massive mobilisation of fat to or from the fatty liver [1] and dysregulated blood lipids because of damaged pancreatic α cells [2], as it is already known, alcohol also damages the pancreas.
So far, no retinal haemorrhages have been reported due to Zieve syndrome in previous studies. In present case, the patient had a history of haemolytic anaemia, for which he had undergone blood transfusion. Patient investigations revealed increased bilirubin level, fragmented red blood cells, and increased lactate dehydrogenase. These were in favour of haemolytic anaemia, postblood transfusion but the coombs test was found to be negative. The patient had history of fever, anaemia. Post-malarial infection can be thought of. Absence of roth spots in fundus findings and other signs and symptoms of malaria like fever with rigours, bodyache, headache, diarrhoea ruled out the diagnosis. Zieve syndrome, consists of a triad of symptoms: haemolytic anaemia, cholestatic jaundice and transient hyperlipidaemia. As discussed in this case, the patient had history of alcohol intake for 10 years. The blood picture showed haemolytic anaemia and liver function test was found to be deranged. Ultrasound revealed steatohepatitis. As the hyperlipidaemia and anaemia improved, an improvement in vision was also seen. It might be an incidental finding as in any condition with retinal haemorrhages, vision improves with time but its association with cholestatic jaundice and transient hyperlipidaemia can be attributed to Zieve syndrome.
There are numerous complications of blood transfusion described in various literatures. Among all those complications, is ocular complication especially retinal haemorrhages which is really uncommon and least understood thus needs further investigations to determine their true relationship [3]. Sallmann L in 1925 mentioned that retinal haemorrhages may occur as a complication of blood transfusion [4]. In 1931, Messinger HC and Eckstein AW also reported a series of 60 cases in which fresh retinal haemorrhages were seen after 12 to 24 hours of blood transfusion in 10 cases, or we can say an incidence of 16 percent [5]. Further, Frey had noted the occurrence of massive retinal haemorrhages following blood transfusion in several cases of leukaemia and pernicious anaemia. Routine ophthalmoscopic examination had shown no haemorrhages before blood transfusion. He added that a large percentage of cases belonged to the blood dyscrasias and that the remaining ones were complicated by pronounced secondary anaemia. Thus, retinosis due to deficiency of erythrocytes is to be expected irrespective of transfusion, and this is validated by the frequent finding at the time of initial ophthalmoscopic examination before tranfusion. The possibility that the haemorrhage appears coincidentally is likely. In the view of this, one does not believe that a major aetiological role can be ascribed to the transfusion per se as haemorrhages were seen even before transfusion and only further investigations reveal whether a true aetiological relationship does exist or not. Previous studies have documented that impaired production of coagulation factors in cirrhosis and thrombocytopaenia may cause haemorrhages in ophthalmic structure [6]. However, in a large survey since retinopathy was not searched in cirrhotics, thrombocytopaenia pathophysiology involving retinopathy in cirrhosis is unknown. Shunts in retinal vasculature which resembles intrarenal and intrapulmonary shunts observed in hepatopulmonary syndrome may be operational in retinal ischaemia and cotton wool spots [7]. Further, increased hydrostatic pressure, hypoalbuminaemia in cirrhosis and resultant decreased oncotic pressure may also contribute to exudate formation via extravasation of plasma contents.
A study conducted by Dittmer K and colleagues supports this suggestion [8]. Moreover, alcohol-induced vitamin E deficiency, reduces polyunsaturated fatty acid levels and causes oxidation of reduced erythrocyte glutathione which leads to enzyme instability and erythrocyte haemolysis. Previous study reported that about forty percent of patients suffering from acute alcoholic hepatitis may progress to liver failure and even death, however alcohol abstinence would result in resolution of symptoms in case of Zieve syndrome [9]. Zieve syndrome is considered to be very rare, as there are approximately 200 case reports published in literature since 1958 [10]. Pathology of Zieve syndrome remains obscure. However, early recognition and prompt diagnosis of Zieve syndrome would avoid unnecessary interventions. Also, there is a need to report and increase the body of published English language medical literature describing Zieve syndrome, as most of the existing literature is written in non-English language.
Conclusion(s)
There are scarcely few studies about retinopathy associated with Zieve syndrome. As it is largely underrecognised and underreported, there is lack of awareness of this condition by physicians. Haemorrhagic retinopathy, and its rare association with Zieve syndrome has been discussed in our case. Intraretinal haemorrhages, exudates, cotton wool spots (retinal infarcts) may be seen on dilated fundoscopy which gets improved after improvement of anaemia, hyperlipidaemia and jaundice that is a triad of Zieve syndrome. These retinal findings may also lead to blindness. Thus, early recognition is important to avoid unnecessary diagnostic procedures.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 03, 2020
Manual Googling: Jan 5, 2021
iThenticate Software: Apr 10, 2021 (20%)
[1]. Melrose WD, Bell PA, Jupe DM, Baikie MJ, Alcohol-associated haemolysis in Zieve’s syndrome: A clinical and laboratory study of five casesClin Lab Haematol 1990 12:159-67.10.1111/ijlh.1990.12.2.1592208946 [Google Scholar] [CrossRef] [PubMed]
[2]. Zieve L, Jaundice, hyperlipidemia and hemolytic anaemia: A heretofore unrecognised syndrome associated with alcoholic fatty liver and cirrhosisAnn Intern Med 1958 48:471-96.10.7326/0003-4819-48-3-47113521581 [Google Scholar] [CrossRef] [PubMed]
[3]. Vinger PF, Sacha BA, Ocular manifestation of hyperlipoproteinaemiaAm J Ophthalmol 1970 70:563-72.10.1016/0002-9394(70)90890-1 [Google Scholar] [CrossRef]
[4]. Sallmann L, Ueber Makulablutungen nach Bluttransfusion bei pernizischer AnamieWiener Med Woch 1925 75:2554 [Google Scholar]
[5]. Messinger HC, Eckstein AW, Retinal hemorrhages after transfusion; 60 cases in which retinae were examined before and after transfusionRhode Island Med Jour 1931 14:171-75. [Google Scholar]
[6]. Shukla S, Sitrin M, Hemolysis in acute alcoholic hepatitis: Zieve’s syndromeACG Case Rep J 2015 2:250-51.10.14309/crj.2015.7526203455 [Google Scholar] [CrossRef] [PubMed]
[7]. Onder C, Bengur T, Selcuk D, Bulent S, Belkis U, Ahmet M, Relationship between retinopathy and cirrhosisWorld J Gastroenterol 2005 11(14):2193-96.10.3748/wjg.v11.i14.219315810092 [Google Scholar] [CrossRef] [PubMed]
[8]. Dittmer K, Nolte W, Tondrow M, Schwörer H, Pathologic fundus changes in advanced liver cirrhosis. Reduction of symptoms after portosystemic shuntOphthalmologe 1998 95:404-07.10.1007/s0034700502889703719 [Google Scholar] [CrossRef] [PubMed]
[9]. Liu MX, Wen XY, Leung YK, Zheng YJ, Jin MS, Jin QL, Hemolytic anemia in alcoholic liver disease: Zieve syndrome: A case report and literature reviewMedicine (Baltimore) 2017 96(47):e874210.1097/MD.000000000000874229381966 [Google Scholar] [CrossRef] [PubMed]
[10]. Piccini J, Haldar S, Jefferson B, Cases from the osler medical service at John Hopkins university. Zieve syndromeAm J Med 2003 115:729-31.10.1016/j.amjmed.2003.10.00514693326 [Google Scholar] [CrossRef] [PubMed]