The EPN is a serious life threatening, necrotising infection which can affect renal parenchyma, collecting system and nearby tissue with presence of gas within the renal system [1,2]. A case of gas-forming necrotising renal infection with pneumaturia was described by Kelly HA and MacCullum WG in 1898 [3]. EPN is usually related to condition causing immunodeficiency like diabetes mellitus [4], and patients with obstructed renal system with infective nidus [5]. Most commonly involved microorganism is Escherichia coli. Other microorganism like Klebsiella, Proteus, Pseudomonas, Clostridium, Streptococcus, Candida, Cryptococcus and aspergillus can also cause EPN [6,7].
The pathogenesis of EPN is multi-factorial. EPN can be associated with diabetes in about 90% of cases and urinary tract obstruction in about 20% [8]. Management of EPN may range from conservative approaches like vigorous resuscitation, antibiotic treatment and glycaemic control to adequate urinary drainage (Double J stenting/Percutaneous nephrostomy/Percutaneous Drainage) and nephrectomy in refractory cases. There are a few articles that compared the emergency nephrectomy, Percutaneous Drainage (PCD) and medical management and there are few studies in which medical management alone was associated with a significantly lower mortality rate [8,9]. There are quite a few case series and studies from India that emphasises on clinical spectrum, pathogenesis, management and outcome of EPN and most of them are retrospective in nature [5,8].
The aim of this study was to check likelihood of kidney salvagibility by minimally invasive approaches in EPN and to evaluate the prognostic factors that support kidney salvagibility in EPN.
Materials and Methods
This was a cross-sectional study conducted during October 2018 to June 2020 on 30 patients who were admitted in Department of Urology, Srirama Chandra Bhanja Medical College and Hospital Medical College, Cuttack, Odisha, India with features of EPN. Institutional Ethical committee clearance was taken in accordance with the Declaration of Helsinki (Letter no. 56). A written informed consent was obtained from all patients before the study. Sample size was calculated, based on previous similar study [10] and considering power of study at 80% with 5% significance level.
Inclusion criteria: Patients admitted based on clinical features and documentation of gas within the renal system on CT scan abdomen (Huang-Tseng) classification [11].
Exclusion criteria: Any fistula between the bowel and urinary tract, history of urinary catheterisation, recent urinary trauma were excluded from the study.
All patients’ detailed clinical, laboratory, radiological, and microbiological findings were noted and evaluated. EPN severity was graded on the basis of Huang classification on CT scan [11].
Class 1- EPN-gas in the renal collecting system only,
Class 2- Gas in renal parenchyma with no extension to the extra-renal space,
Class 3A- Extension of gas or abscess to the perinephric space,
Class 3B- Extension of gas or abscess to the pararenal space,
Class 4- Bilateral EPN or EPN in a solitary kidney.
There are few factors that have been associated with poor outcome in EPN; which include shock, altered mental status, raised serum creatinine, platelet count <120000/cumm, severe proteinuria [11]. These prognostic factors were applied to all EPN patients to evaluate whether these factors are associated with conservative management failure.
Conservative management of EPN was defined as medical treatment alone or a combination of medical treatment and Percutaneous catheter drainage/Percutaneous nephrostomy/Double J stenting (PCD/PCN/ DJ stenting). Conservative treatment was defined successful on clinical improvement of patient and disappearance/decrease in gas on follow-up imaging during hospitalisation and after discharge from hospital.
Treatment protocol for EPN management included, fluid resuscitation, good glycaemic control using insulin infusion, close clinical and biochemical monitoring, electrolyte management, empirical antibiotics covering both as Gram-negative and Gram-positive bacteria. Culture specific antibiotics were started after culture-sensitivity report of urine or blood culture. Piperacillin-tazobactum was started as an empirical therapy and aminoglycosides were added if renal function was normal. Plan for PCD or DJ stent insertion was dependent on radiological and clinical extent of disease.
Presence of internal echoes or debris in pelvis and calyces with obstruction of urinary system was managed by insertion of malecotor pigtail catheter. Deterioration in clinical parameter on this protocol led to consideration for nephrectomy. Patients who were managed conservatively were included in good outcome group while the patients who required nephrectomy were included in poor outcome group. Patients in good outcome group (conservatively managed) were followed-up for six months; during follow-up clinical examination, urine analysis, plain film, ultrasound of abdomen and pelvis was done.
Statistical Analysis
Continuous variables were analysed with the Unpaired t-test and categorical variables were analysed with Fisher-Exact test and multiple logistic regression test. Results were considered statistical significance when p-value <0.05. The data was analysed using EpiInfo software.
Results
The mean age of the population was 53±7.84 years. Male to female ratio was 1:1.5. Left side was involved in total 21 (70%) patients. All baseline characteristics of the 30 study subjects are shown in [Table/Fig-1].
Clinical and laboratory findings of EPN.
| Clinical presentation | Present | Absent |
|---|
| Fever | 24 (80%) | 6 (20%) |
| Flank and abdominal pain | 21 (70%) | 9 (30%) |
| Nausea and vomiting | 6 (21%) | 24 (79%) |
| Diabetes mellitus | 24 (80%) | 6 (20%) |
| Altered mental status | 7 (23.33%) | 23 (76.66%) |
| Shock | 10 (33.33%) | 20 (66.66%) |
| Laboratory finding |
| HbA1C | | - |
| >7.5%<7.5% | 21 (70%)9 (30%) | - |
| Total Leucocyte Count (TLC) |
| >12×109/L<12×109/L | 20 (66.66%)10 (33.3%) | |
| Platelet Count (PC) |
| <12×109/L>12×109/L | 13 (43.33%)17 (56.66%) | |
| Serum creatinine |
| >2.5 mg/dL<2.5 mg/dL | 9 (30%)21 (70%) | |
| Urine analysis |
| HaematuriaProteinuriaPyuria | 3 (10%)7 (23.33%)24 (80%) | 27 (90%)23 (76.66%)6 (20%) |
| Urine culture |
| E.coliKlebsiellaProteus | 27 (90%)22 (81.48%)5 (18.51%) | 3 (10%)8 (26.6%)25 (83.3%) |
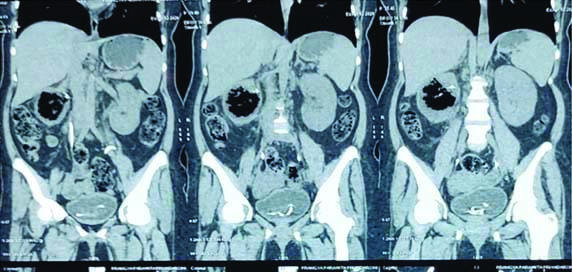
Majority of the patients (53.33%) belonged to the Class 1 of the Huang-Tseng classification. According to CT scan classification class 1 was associated with good outcome which was statistically significant p-value <0.05. Urine culture identified organism in 90% (n=27) of cases [Table/Fig-2,3].
Radiological CT (Huang-Tseng) classification [11].
| CT classification (variables) | Total 30 | Good outcome (N=21) | Poor outcome (N=9) | p-value (Chi-squared test) |
|---|
| Class 1 | 16 | 16 (76.19%) | 0 | 0.0002 |
| Class 2 | 3 | 2 (9.52%) | 1 (11.11%) | 0.89 |
| Class 3a | 5 | 2 (9.52%) | 3 (33.33%) | 0.114 |
| Class 3b | 6 | 1 (4.7%) | 5 (55.55%) | 0.0017 |
| Class 4 | 0 | 0 | 0 | 0 |
(p-value <0.05 considered to be significant)
Radiological images of EPN showing gas in pelvicaleceal system of right kidney.
There was no statistically significant difference noted in HbA1c level, urinary tract obstruction at the time of presentation, sign symptom duration.
Reduced platelet count (p-value=0.0143), altered mental status (p-value=0.0073), severe proteinuria (p-value=0.0213), renal function impairment (p-value=0.0493), increased age (p-value<0.05) and shock (p-value=0.0127) were statistically significant according to multiple logistic regression test and associated with poor outcome [Table/Fig-4]. A 76% (n=21) cases were classified as good outcome group and 24% (n=9) cases classified as poor outcome group for which nephrectomy was done. There was no significant difference noted for Hb1Ac, urinary tract obstruction. Renal function impairment, thrombocytopenia, altered mental status at presentation and shock was associated with poor outcome.
Factors associated with good outcome vs poor outcome.
| Factors | Good outcome (N=21) | Poor outcome (N=9) | p-value (t-test) |
|---|
| HbA1C >7.5% | 15 (71.42%) | 6 (66.66%) | 0.7977 |
| Urinary tract obstruction | 5 (23.8%) | 3 (33.33%) | 0.5948 |
| Mean Age (years) | 50±6.32 | 60±6.65 | 0.0005 |
| Duration of sign and symptoms (days) | 8 | 6.1 | - |
| Proteinuria (3 mg/dL) | 3 (14.28%) | 5 (55.55%) | 0.0213 |
| Platelet count <12×109/L | 6 (28.57%) | 7 (77.77%) | 0.0143 |
| Renal function impairment (serum creatinine >2.5 mg/dL) | 4 (19.04%) | 5 (55.55%) | 0.0493 |
| Altered mental status | 2 (9.56%) | 5 (55.55%) | 0.0073 |
| Shock | 4 (19.04%) | 6 (66.66%) | 0 .0127 |
Antibiotics were given to all patients out of which 5 (16.66%) responded clinically and biochemically. Urinary tract obstruction was present at the time of admission along with EPN in 6 (20%) cases which were drained immediately by either DJ stent or pigtail catheter insertion. The 70% (n=21) patients had HbA1C more than 7.5%. All patients who did not respond clinically, biochemically and radiological characteristics by antibiotics required PCD/PCN/DJ stent placement [Table/Fig-5]. Nine patients who had significant renal or perirenal collections with rising serum creatinine, and uncontrolled sepsis after 72 hour of conservative treatment warranted nephrectomy. Patient who was managed conservatively included in good outcome group while those requiring nephrectomy were included in poor outcome group [Table/Fig-6].
| Management outcome | Good outcome | Poor outcome | p-value |
|---|
| Antibiotics only | 5 (16.66%) | 0 | 0.0206 |
| PCD | 18 (60%) | 7 (23.33%) | 0.0043 |
| PCD with DJ stenting | 4 (13.33%) | 2 (6.66%) | 0.3931 |
| DJ stenting | 3 (10%) | 0 | 0.0780 |
| Nephrectomy | 0 | 9 (30%) | 0.0013 |
PCD: Percutaneous catheter drainage; (p-value <0.05 considered to be significant)

Discussion
The EPN has been defined as a necrotising infection of the renal parenchyma and its surrounding areas that result in the presence of gas in the renal parenchyma, collecting system, or perinephric tissue [11]. This study was aimed to check likelihood of kidney salvagibility by minimally invasive approaches in EPN and to evaluate the prognostic factors that support kidney salvagibility in EPN.
Mean age of the population in the study was 53±7.84 years and EPN was more common in females (66.66%) while similar study conducted by Aswathaman K et al., and Sokhal AK et al., showed 46.34% and 62.16% females had EPN, respectively [8,12].
Poor outcome group had higher mean age which was statistically significant (p-value<0.05) when compared to the good outcome group. The clinical features of EPN in patients were pain in flank (70%) and fever (80%) being the predominant symptom which was similar to the study conducted by Ahmed R et al., [13]. DM was most common comorbidity which was present in 80% of patients that correlates well with the studies of Shokeir AA et al., and Jain A et al., [14,15].
In the present study, reduced platelet count (p-value=0.0143), altered mental status (p-value=0.0073), severe proteinuria (p-value=0.0213), renal function impairment (p-value=0.0493), increased age (p-value <0.05) and shock (p-value=0.0127) were statistically significant and associated with poor outcome. Similar outcome was reported by Jain A at el., in which comorbidities (p-value <0.001), high TLC (p-value=0.036), low BMI (p-value=0.015), thrombocytopenia (p-value=0.046), and hypoalbuminemia (p-value=0.001) were significantly associated with poor outcome [15]. In a similar study conducted by Kapoor R et al., presence of an altered mental status, thrombocytopenia, renal failure and severe hyponatremia at presentation were associated with higher mortality rates, and severe renal parenchymal destruction is associated with the need for nephrectomy [16]. In the present study 80% patient had diabetes, 16.66% had hypertension and 3.33% patient had hypothyroidism. Similar data were found by Jain A et al., in which 86% patient had diabetes mellitus, 7% patient had hypertension and 2.71 % patients had hypothyroidism [15].
In the present study, most common organisms cultured from urine were E.coli. In a similar study, published by Mohammad IA et al., in which E.coli was grown in the urine of 80% of patients and 25% had E.coli in blood cultures [17].
CT abdomen is best investigation to diagnose and demonstrate gas, presence, extent, and prognosis of the disease. Based on CT abdomen classification (Huang) findings of patients were divided in following classes: Class 1 (16), Class 2 (3), Class 3a and 3b (5 and 6) and Class 4 (0). In this study, 100% of patients in class 1(1/1) had a good outcome while 1 patient in class 2, 3 patients with class 3a and 5 patients in class 3b was associated with poor outcome (nephrectomy). In a study conducted by Sokhal AK et al., they had Class 1 (51%), Class 2 (10%), Class 3a and 3b (16% and 19%) and Class 4 (4%) [12]. Disease extent on CT scan correlated with clinical outcome. All class 1 patients responded well with a favourable outcome which was similar to their study. EPN extending to perinephric and pararenal tissue seen in 84% of the patients in the non-responder group had a poor outcome [12].
In the present study, all good outcome patients were managed conservatively with the use of antibiotics, PCN, Percutaneous Catheter Drainage (PCD) with DJ stenting while, nephrectomy was done in total 9 (30%) cases in poor outcome group. There was no mortality seen in the study. Study by Huang JJ and Tseng CC and Sokhal AK et al., was associated with mortality in 18.8% patient and 8% patients, respectively [11,12].
Limitation(s)
The major limitations of the present study was the lesser duration of follow-up.
Conclusion(s)
There is a definite possibility of renal salvagibility by minimally invasive approaches in EPN in properly selected patients of EPN. Shock, altered mental status, raised serum creatinine platelet count <120000/cumm and severe proteinuria is poor outcome factors which can lead to nephrectomy in conservatively managed cases of EPN.
(p-value <0.05 considered to be significant)
PCD: Percutaneous catheter drainage; (p-value <0.05 considered to be significant)