A Rare Case of Isolated Internuclear Ophthalmoparesis following Head Injury
Teena Mariet Mendonca1, Gladys R Rodrigues2, Sreelakshmi Salim3
1 Assistant Professor, Department of Ophthalmology, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Mangalore, Karnataka, India.
2 Assistant Professor, Department of Ophthalmology, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Mangalore, Karnataka, India.
3 Junior Resident, Department of Ophthalmology, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Teena Mariet Mendonca, Attavar, Mangalore, Karnataka, India.
E-mail: tmendonca87@gmail.com
Cranial neuropathies, Internuclear ophthalmoplegia, Neurotrauma, Ocular motility
This draft is about a 46-year-old man, referred to the tertiary eye care center for limitation of eye movements in the right eye following head trauma. The patient had sustained head trauma due to a road traffic accident two days prior to the presentation. He had history of loss of consciousness for a few minutes and was under neurosurgical observation. He had no visual complaints, diplopia or vertigo on presentation.
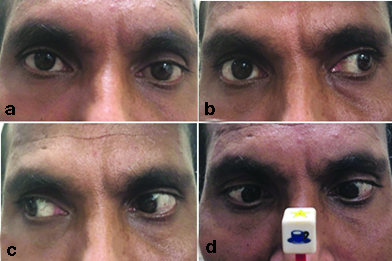
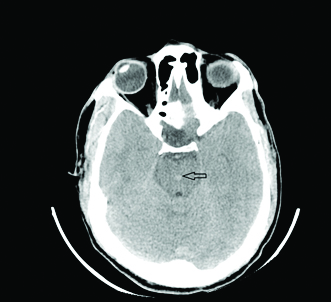
On examination, his best-corrected visual acuity of 20/20 in both eyes. The pupillary reactions were normal in both eyes. The patient was orthotropic in primary gaze position. Ocular motility examination showed adduction deficit in the right eye (-2 limitation) and jerky nystagmus in the left eye on left gaze. Range of ocular motility in left eye was normal. Convergence was found to be normal [Table/Fig-1]. Fundus examination was normal in both eyes. Non-enhanced CT scan of brain showed petechial haemorrhage in central midbrain with surrounding diffuse oedema [Table/Fig-2]. The patient was diagnosed with right Internuclear Ophthalmoparesis (INO). The patient showed spontaneous improvement in four weeks.
Clinical photograph of the patient showing orthophoria in primary gaze (a), Adduction limitation of the right eye in left gaze (b), Normal right gaze (c), and Normal convergence (d).
Computed tomography- (axial section) of the midbrain at the level of inferior colliculus showing petechial haemorrhage at the central midbrain (black arrow).
The INO is a type of gaze abnormality characterised by limited adduction of affected eye with abduction nystagmus of contralateral eye in lateral gaze. INO localises the lesion to Medial Longitudinal Fasciculus (MLF) in region of midbrain or pons [1]. INO can present as unilateral or bilateral gaze abnormality. Horizontal gaze centre is located at Pontine Paramedian Reticular Formation (PPRF) in the midbrain. The MLF pathway is an internuclear neuronal pathway, which connects abducent nucleus in pons to the medial rectus sub-nucleus of the contralateral oculomotor nucleus in midbrain. MLF is a white matter fiber tract located close to midline just ventral to the cerebral aqueduct and the fourth ventricle [1]. Convergence is usually spared in posterior lesions, which involve lesions caudal to oculomotor nucleus. Intact convergence can help differentiate INO from pupil, sparing partial third nerve palsy.
Various causes of INO include multiple sclerosis, cerebrovascular accidents, encephalitis, hydrocephalus, tuberculoma, tumours with trauma being less common. Multiple sclerosis and cerebrovascular accidents constitute 70% of the cases of INO. Multiple sclerosis and other demyelinating disorders are considered as the most common causes of bilateral INO. Ischemic stroke is found to be the most common cause of unilateral INO [2-4].
INO is considered to be a rare entity after a blunt head injury [2,5,6]. Although pathophysiologic mechanism of post traumatic INO is unclear, traumatic displacement of brainstem and subsequent development of shearing forces within white matter tract is hypothesised to cause injury to MLF. Anterior portion of the brainstem is relatively better fixated by small perforating branches of basilar artery compared to posterior segment. Relative free movement of posterior portion of brainstem may cause shearing forces leading to tearing or stretching of the cerebral tissue [1,7].
In this patient, petechial haemorrhage which was seen in the central midbrain on CT scan, along with surrounding vasogenic oedema can explain the constellation of findings. Since convergence was found to be intact in the patient, site of injury appeared to be caudal to oculomotor nucleus. Absence of diplopia in this patient could be due to orthophoria in primary gaze.
Magnetic Resonance Imaging (MRI) is a better imaging modality for axonal injuries with haemorrhage being more easily detected on T1 and susceptibility weighted imaging sequences. The prognosis of traumatic INO is usually good and these may resolve spontaneously [6,7]. In this case, the patient improved spontaneously within four weeks with conservative management.
A comprehensive examination of ocular motility in a patient with head trauma can be very useful to understand the nature and impact of the trauma.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 26, 2020
Manual Googling: Mar 10, 2021
iThenticate Software: Apr 27, 2021 (14%)
[1]. Lee SH, Nam TK, Park YS, Kwon JT, A case of traumatic unilateral internuclear ophthalmoplegia: Clinical significance of susceptibility-weighted imagingKorean J Neurotrauma 2016 12(2):140-43.10.13004/kjnt.2016.12.2.14027857923 [Google Scholar] [CrossRef] [PubMed]
[2]. Keane JR, Internuclear ophthalmoplegia: Unusual causes in 114 of 410 patientsArch Neurol 2005 62(5):714-17.10.1001/archneur.62.5.71415883257 [Google Scholar] [CrossRef] [PubMed]
[3]. Shetty NU, Shpilko M, Internuclear ophthalmoplegia as a sole presentation of acute ischemic stroke involving the midbrain with an NIH stroke scale of oneJ Biol Med Sci 2017 1(2):104 [Google Scholar]
[4]. Serra A, Skelly MM, Jacobs JB, Walker MF, Cohen JA, Improvement of internuclear ophthalmoparesis in multiple sclerosis with dalfampridineNeurology 2014 83(2):192-94.10.1212/WNL.000000000000056724907233 [Google Scholar] [CrossRef] [PubMed]
[5]. Hai S, Elkbuli A, Kinslow K, McKenney M, Boneva D, When “looks” can be deceiving-Internuclear ophthalmoplegia after mild traumatic brain injury: Case report and literature reviewInternational Journal of Surgery Case Reports 2019 63:19-22.10.1016/j.ijscr.2019.08.03231539826 [Google Scholar] [CrossRef] [PubMed]
[6]. Jinmann C, Kim M, Bilateral internuclear ophthalmoplegia following head traumaIndian J Ophthalmol 2017 65(3):246-47.10.4103/ijo.IJO_236_1728440256 [Google Scholar] [CrossRef] [PubMed]
[7]. Doe JW 4th, Jay WM, Traumatic unilateral internuclear ophthalmoplegiaSemin Ophthalmol 2006 21(4):245-53.10.1080/0882053060098746217182412 [Google Scholar] [CrossRef] [PubMed]