Foreign body aspiration is a very serious and life-threatening emergency. Swallowing of foreign bodies is most common among paediatric patients, as the elderlies are also at risk. Presence of aerodigestive foreign body may be observed in all age groups [1]. Taking into account the risk of infection and perforation, it often requires removal under conditions of maximal safety and minimal trauma, especially for short-blunt and sharp-pointed objects [2,3]. An infinite variety of foreign bodies may be inhaled or swallowed.
Humans can accidently ingest it either while removing spikelets from clothes or with food and water containing bhurut seeds. Due to its sharp spines, it gets stuck in the upper aerodigestive tract and seldom reaches the oesophagus. As the available literature related to Indian sandbur is limited, the objective of this retrospective study was to describe a case series of unusual foreign body bhurut in western Rajasthan.
Materials and Methods
This retrospective study was conducted at the Department of ENT at Pandit Deendayal Upadhyay Medical College, Churu, Rajasthan, India from 1 January 2020 to 31 December 2020. Ethical concerns were addressed and all the patient data were kept anonymous.
Inclusion criteria: Patients of any age and sex presenting with a foreign body in the upper aerodigestive tract with documentation of bhurut as a foreign body.
Exclusion criteria: Patients presenting with any other foreign body except bhurut in the upper aerodigestive tract (as reported in the case file) and patients presenting with a foreign body in the trachea, bronchus and lower oesophagous were included in the study.
As indicated, patients were subjected to rigid endoscopic assessment and forceps removal of the foreign bodies. The techniques that were used for the removal of foreign bodies were the following:
OPD procedure: The removal of foreign bodies lodged in the faucial tonsils, the base of the tongue and valeculla was performed in the OPD setup. It was done under local anaesthesia using lignocaine 10% spray. A Hartmann’s forceps/straight Blakesley forcep was used to remove the foreign body.
Direct laryngoscopy and forceps removal: This procedure was done under GA. All patients were observed postoperatively for 24 hours and antibiotics were given for seven days along with analgesics.
The medical records of the patients were analysed and data were collected using a structured questionnaire. The questionnaire included information such as age, sex, anatomical lodgement of foreign body, signs and symptoms, duration of lodgement before confirmation and removal.
Statistical Analysis
The data were entered and analysed using a Microsoft Excel sheet. The qualitative variables were presented as numbers and percentages, whereas quantitative variables were presented as mean and standard deviation.
Results
During the period of study, a total of 21 patients with established foreign body (bhurut) in the airway were studied. There was a male predominance {14 (66.66%)}. Most patients {15 (71.42%)} of bhurut ingestion were above 20 years of age and range from 6 to 65 years [Table/Fig-1]. The distribution of patients according to the place of residence showed that the maximum number of patients belonged to the rural area {18 (85.71%)}.
Socio-demographic profile of cases.
| Variables | No. of patients | Percentage (%) |
|---|
| Age groups (years) |
| <20 | 6 | 28.57 |
| 20-30 | 3 | 14.28 |
| 31-40 | 3 | 14.28 |
| 41-50 | 6 | 28.57 |
| >50 | 3 | 14.28 |
| Sex |
| Male | 14 | 66.66 |
| Female | 7 | 33.33 |
| Area |
| Rural | 18 | 85.71 |
| Urban | 3 | 14.28 |
Bhurut was found in the pharynx in 13 (61.90%) patients and larynx in 8 (38.09%) patients [Table/Fig-2,3]. In pharynx bhurut was present in 11 (52.38%) patients in the oropharynx and 2 (9.53%) in hypopharynx.
Site of impaction of foreign body.
| Site of impaction | No. of patients | Percentage (%) |
|---|
| Oropharynx |
| Tonsil | 2 | 9.52 |
| Base of tongue | 4 | 19.04 |
| Vallecula | 5 | 23.80 |
| Larynx |
| Vocal cord | 7 | 33.33 |
| Aryepiglottic fold | 1 | 4.76 |
| Hypopharynx |
| Pyriform fossa | 1 | 4.76 |
| Cricopharynx | 1 | 4.76 |
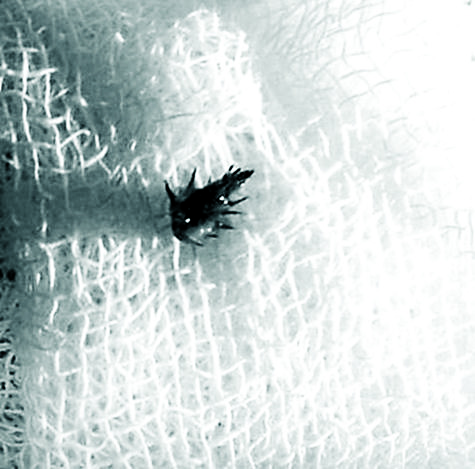
Endoscopic image showing bhurut on left vocal cord.

The time of presentation in patients with bhurut in the aerodigestive tract varied from three hours to five days. In 18 (85.71%) cases, the diagnosis was formulated within three to six hours after the ingestion, and in the remaining three (14.28 %) cases delay of more than 24 hours was reported. Among the patients, the most common symptom was foreign body sensation (100%) [Table/Fig-4].
| Clinical presentation | No. of patients | Percentage of patients |
|---|
| Hoarseness of voice | 7 | 33.33 |
| Odyanophagia | 12 | 57.14 |
| Drooling of saliva | 2 | 9.52 |
| Foreign body sensation | 21 | 100 |
The mode of management in 11 (52.38%) patients with a foreign body in the oropharynx was Tilleys forcep or straight Blakesley forcep under local anaesthesia while for 10 patients (47.61%) with a foreign body in hypopharynx and larynx was direct laryngoscopy with forcep removal, under GA.
Bhurut was successfully removed in all the patients [Table/Fig-5]. There were no postoperative complications in 18 (91.89%) cases, the remaining three (8.11 %) patients had persistence of hoarseness of voice due to oedema of the vocal cord, at the first follow-up visit after seven days.
Showing bhurut removed from vocal cord.
Discussion
Delayed diagnosis and treatment of an aspirated foreign body is associated with serious or even fatal complications [6,7]. Carelessness of parents (in the case of children), poor vision, drug addiction and rapid eating are some of the factors responsible for this. Psychological factors like mental retardation, behavioural disorders, anxiety neurosis, and hyperkinetic syndrome also can compound the problem [8].
The age of patients ranged from six years to 65 years. The maximum number of patients of bhurut ingestion belonged to rural area 18 (85.71%). People working in fields in rural areas are more prone to bhurut ingestion. Bhurut is inhaled or swallowed accidentally while drinking water or taking food. Bhurut gets attached to the body and clothes of people and they try to remove bhurut by catching it with their teeth and while doing so it is accidentally inhaled [4]. In this study, the most common site of bhurut impaction was vocal cords in seven patients (33.33%). Chhangani DL and Agarwal KK, also reported that the most common site of bhurut impaction was the vocal cord, while other sites were valleculae and the pyriform sinus [4].
The signs and symptoms of bhurut ingestion depend on the site of lodgement. The first symptoms can be Foreign body sensation and localised pain [9]. In some studies, on the pharyngeal foreign body, the sensation of the presence of a foreign body is the only symptom found to correlate with the site of impaction [10,11]. Symptoms range from mild odynophagia, dysphagia, drooling of saliva, foreign body sensation in throat and hoarseness of voice [12]. These symptoms are caused due to irritation by spikelets of bhurut. In this study, the most common symptom was foreign body sensation in the throat of all patients (100%). In other studies, the symptoms of oesophageal foreign body diseases are foreign body sensation, sore throat, dysphagia, odynophagia, retrosternal pain, retching, and vomiting [13-16].
Most of the patients {18 (85.71%)} came within three to six hours of foreign body ingestion. Three patients (14.28%) came 24 hours after foreign body ingestion. The main reason for late presentation could be low socio-economic status and lack of awareness among patients.
Bhurut was removed successfully in 18 patients without any complication. The three patients with delayed presentation had persistence of hoarseness of voice after the removal of foreign body. Sharp foreign bodies have a higher risk of severe complications if the treatment is delayed beyond 24 hours [17] and a high frequency of bleeding compared to other foreign body diseases [18]. As reported in the present study, bhurut ingestion is common in desert areas. Thus, it should be considered an important clinical diagnosis in patients of foreign body ingestion from similar areas and areas where Cenchrus biflorus is commonly found.
Limitation(s)
As the findings of the study are based on the experience of the single institute, the results cannot be generalised to other regions.
Conclusion(s)
Clinicians should suspect bhurut ingestion in patients presenting with foreign body ingestion from the desert region. The removal of the bhurut under local or GA achieves good results. Awareness in the community regarding proper handling and avoiding exposure to bhurut will help in reducing the incidence of the problem. Community awareness is necessary to seek early medical attention and timely removal of the foreign body to avoid complications like vocal cord oedema leading to hoarseness of voice and respiratory distress if left unattended.