Introduction
Several factors have been identified to influence concussion. Migraine has been identified as a common symptom reported after concussion which has been related to a worse prognosis. Concussion is a common brain injury that affects physical and cognitive performance. While several studies indicated that adolescents are more likely to develop concussion, in the last decade concussion has been mainly explored in adults.
Aim
To investigate the effect of migraine on functional performance and self-reported symptoms in children with concussion.
Materials and Methods
This cross-sectional study involved 35 symptomatic children with concussion aged 9-17 years recruited within one year from their concussion injury at a tertiary care centre in Pittsburgh, PA, Unites States of America. Participants’ symptoms and functional performance were assessed using the Postconcussion Symptoms Scale (PCSS) and the Functional Gait Assessment (FGA) respectively. Statistical Package for the Social Sciences (SPSS) Statistics for Windows (version 22; IBM Corp, Armonk, NY) was used for all statistical analysis.
Results
Mann-Whitney U test showed that concussed children with migraine had significantly worse symptoms of fatigue and visual problems (p<0.05). The participants had a mean age of 14.03±2.47 years and 66% were females.
Conclusion
Although concussed children with and without migraine did not show any differences on functional performance, worse fatigue and visual symptoms were found in concussed children with migraine.
Introduction
Concussion is one of the most common acquired brain injuries that may lead to health consequences affecting the patient’s health on several domains including physical and cognitive performance [1,2]. Awareness of concussion has increased in the medical community and scientific research in the last decade and has been mainly explored in adults [3-5]. Several studies indicate that adolescents are more likely to develop concussion compared to adults [6,7]. Previous studies found that concussion injuries affect several functional domains, including cognitive, balance, and mobility, and that these affected domains recover after concussion at different rates [8-11]. Utilising a comprehensive examination to assess concussion in different domains enables clinicians to determine the impact of the injury and assist in monitoring recovery [12,13].
Not all hits to the head cause a concussion. Studies of athletes’ head acceleration and deceleration showed that the amount of force exerted to the head that led to a concussion injury varies greatly [14,15].
Most concussion injuries resolve within a few weeks. However, patients with concussion are being seen in concussion clinics several months after their injury. In an effort to understand risk factors of acquiring a concussion, multiple studies identified preinjury and postinjury factors that influence concussion severity and recovery. Several symptoms and factors have been tied to prolonged recovery and worse prognosis of a concussion including dizziness, headache, migraine, prior concussion, female gender, and younger age [13,16-21].
Migraine has been identified as a common disorder reported after concussion which has been related to a worse prognosis after concussion [17,22]. Migraine is a headache associated with light and/or noise discomfort and should be diagnosed based on the International Headache Society criteria [23]. Migraine was described as one of the risk factors of concussion [24]. Eckner JT et al., 2017 suggest that athletes with concussion should have a modified care plan when they present with migraine headache [25].
This study had two main objectives first was to compare the functional performance of children with concussion between migraineurs and non-migraineurs, second was to compare severity of symptoms of children with concussion between migraineurs and non-migraineurs. Hence, this study aimed to investigate and compare the effect of migraine between functional performance and self-reported symptoms in children with concussion.
Materials and Methods
This cross-sectional study involved a convenience sample of 40 symptomatic children (23 females) with concussion in which all children visiting the concussion clinic were screened for eligibility and approached for recruitment over a recruitment period of eight months. Children with concussion were recruited from a tertiary balance centre at the University of Pittsburgh Medical Centre, Pittsburgh, United States of America. This study was approved by the Institutional Review Board at University of Pittsburgh (Irb approval number: PrO11100023).
Inclusion criteria: Children were included in the study if they met the inclusion criteria of having a clinical diagnosis of concussion (within the past one year) based on a complete neurologic and neuro-otologic examination performed by a licensed neurotologist. The participants were children attending a mainstream school.
Exclusion criteria: Children with central nervous system involvement other than migraine or concussion, significant learning difficulties, and/or an orthopaedic deficit affecting their balance or gait were excluded. Following the exclusion and inclusion criteria 35 participants were consented and finally included in study. All data collection was conducted by a physical therapist with expertise in examining and treating children with concussion. The inclusion and exclusion criteria as well as the study procedures and aims were explained to the physicians at the balance centre. Physicians explained the study briefly and instructed the patients and their guardians to see the researcher if they were interested in learning more about the study. The methodology of the study was fully explained to the eligible children and their parents before participating in the study, and the participants signed informed consent.
Sample size calculation: Sample size was estimated using G Power software [26] using PCSS values reported from a previous study of 84 children (mean age=15.7, SD=1.6 years) with and without migraine. The analysis revealed that a sample of 16 participants (8 participants in each group) is needed to capture difference on PCSS between 2 independent groups with alpha level of 0.05 and a power of 0.80 for an effect size of 1.6 that was calculated from the previous study [22].
After consenting, participants’ demographics including age, gender, height, weight, Body Mass Index (BMI), migraine, number of previous concussions, and the date of the concussion injury were collected by the investigator. Participants’ functional performance was assessed using the FGA, which was performed by a trained physical therapist in the same session shortly after completing the PCSS. The FGA is a 10 item performance based test that includes nine walking tasks under different conditions, in addition to stair climbing. The tasks of the FGA include normal gait, gait with change in speed, gait with horizontal and vertical head turns, gait with a quick pivot turn, gait with stepping over obstacles, walking heel to toe, gait with eyes closed, walking backwards, and climbing and descending steps. The FGA has a score range of 0 to 30 with each task rated from 0 to 3. A lower FGA score indicates worse performance [27].
Participants were contacted by mail after the gait data were collected and were asked to provide consent for retrieval of the PCSS from their patient chart. Participants’ concussion symptoms were assessed using a computerised version of the PCSS. The PCSS is a self-reported symptoms assessment tool used in clinical settings to evaluate the severity of concussion symptoms. The PCSS includes 22 items with a score range of 0 to 132. The participants were asked to rate the intensity of their symptoms including drowsiness, dizziness, nausea, vomiting, headache, imbalance, visual problems, fatigue, sleeping less or more than usual, sensitivity to light and noise, emotional symptoms, nervousness, irritability, sadness, feeling foggy or slowed down, numbness, and difficulties with remembering and concentrating. Each item is rated by the participant on a 0 to 6 Likert scale. A higher score on PCSS indicates worse concussion symptoms [28]. The participants performed the PCSS on a computer in a private room to eliminate distractions. A trained staff member was available if the participant required any help completing the PCSS.
Statistical Analysis
The descriptive data were reported by their means and standard deviations. Independent samples t-test and independent samples Mann-Whitney U test were used as appropriate to test differences between children with and without migraine. Exact p-values were reported. The significance level was set at p-value <0.05. The SPSS Statistics for Windows (version 22; IBM Corp, Armonk, NY) was used for all statistical analysis.
Results
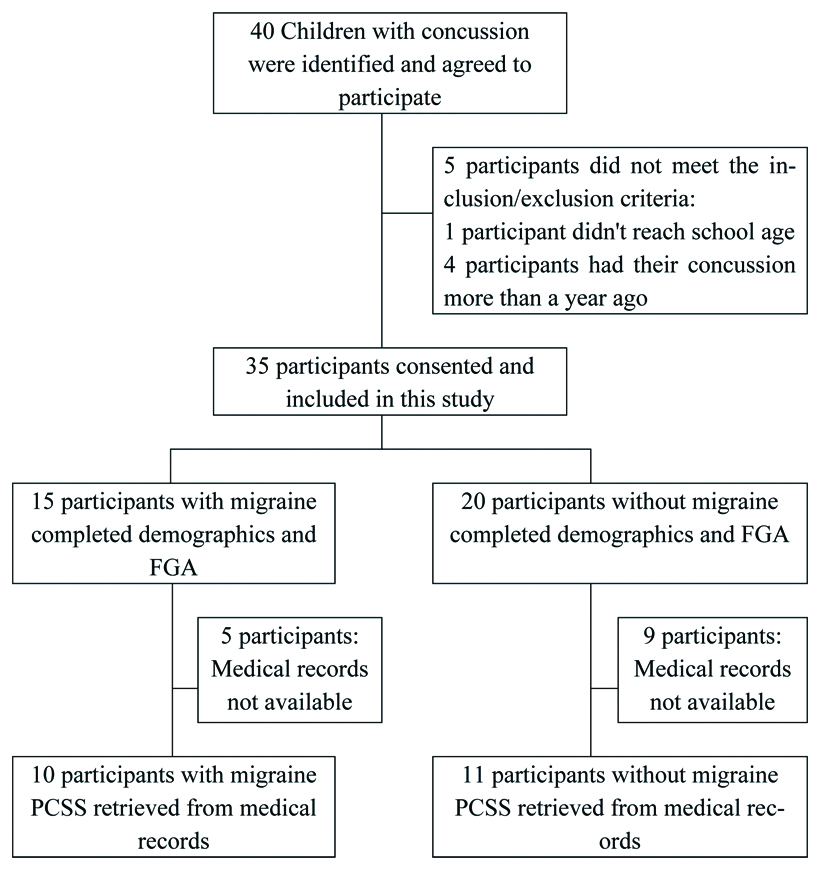
Forty children with concussion were invited to participate in the study with only 35 children meeting the inclusion and exclusion criteria of the study. All participants consented and completed demographics questionnaire and FGA testing. The PCSS results from clinical records were available from 21 participants [Table/Fig-1].
Flowchart of the participants.
The included participants had a mean age of 14.03±2.47 years and 66% were females. No significant differences were found between concussed children with and without migraine in demographic characteristics. Furthermore, no significant differences were found between concussed children with and without migraine in FGA scores [Table/Fig-2].
Demographic characteristics of the participants and comparisons between children with concussion with and without migraine on demographic characteristics and Functional Gait Assessment (FGA) scores.
| Variable | All n=35 | Migraine n=15 | No migraine n=20 | p-value |
|---|
| Mean | SD | Mean | SD | Mean | SD |
|---|
| Age (years) | 14.03 | 2.47 | 14.13 | 2.10 | 13.95 | 2.76 | 0.831 |
| Gender |
| Female n (%) | 23 | 66% | 12 | 34% | 11 | 31% | 0.123 |
| Male n (%) | 12 | 34% | 3 | 9% | 9 | 26% |
| Height (m) | 1.59 | 0.14 | 1.59 | 0.12 | 1.60 | 0.15 | 0.794 |
| Weight (kg) | 54.60 | 15.73 | 53.22 | 11.63 | 55.70 | 18.59 | 0.656 |
| Body mass index (kg/m2) | 21.12 | 3.60 | 20.94 | 2.74 | 21.27 | 4.23 | 0.793 |
| Number of previous concussions | 1.53 | 0.81 | 1.64 | 0.81 | 1.47 | 0.83 | 0.608 |
| Time since concussion (days) | 77.85 | 60.97 | 98.42 | 70.57 | 61.40 | 48.36 | 0.119 |
| Functional gait assessment | 26.91 | 2.88 | 26.87 | 2.61 | 26.95 | 3.14 | 0.934 |
p-value for all variable use independent samples t-test; for gender Chi-square test used; m=meter; kg=kilogram
Concussed children with migraine showed a trend of increased symptoms compared to concussed children without migraine on all items of the PCSS as well as the total PCSS score except for two items, the vomiting and the sleeping more than usual. Although most symptoms were worse in children with migraine, only few reached statistical significance. In fatigue symptoms concussed children with migraine showed significantly (p=0.043) increased symptoms (mean=2.00, SD=1.89) than concussed children without migraine (mean=0.45, SD=0.93). Concussed children with migraine reported significantly (p=0.024) worse visual problems (mean=2.10, SD=1.97) than concussed children without migraine (mean=0.36, SD=0.92) [Table/Fig-3].
Comparisons between children with concussion with and without migraine on the PCSS and the individual items of PCSS.
| Variable | All n=21 | Migraine n=10 | No migraine n=11 | p-value |
|---|
| Mean | SD | Mean | SD | Mean | SD |
|---|
| PCSS (Total) | 23.52 | 23.28 | 32.60 | 27.71 | 15.27 | 15.37 | 0.114 |
| Headache | 2.35 | 1.73 | 2.70 | 1.77 | 2.00 | 1.70 | 0.393 |
| Nausea | 0.57 | 1.25 | 0.70 | 1.34 | 0.45 | 1.21 | 0.654 |
| Vomiting | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | |
| Balance Problems | 1.10 | 1.41 | 1.5 | 1.58 | 0.73 | 1.19 | 0.282 |
| Dizziness | 1.29 | 1.45 | 1.5 | 1.65 | 1.09 | 1.30 | 0.654 |
| Fatigue | 1.19 | 1.63 | 2.00 | 1.89 | 0.45 | 0.93 | 0.043* |
| Trouble falling asleep | 1.29 | 2.15 | 2.10 | 2.77 | 0.55 | 1.04 | 0.387 |
| Sleeping more than usual | 0.38 | 1.12 | 0.30 | 0.48 | 0.45 | 1.51 | 0.512 |
| Sleeping less than usual | 1.05 | 2.09 | 2.00 | 2.71 | 0.18 | 0.60 | 0.197 |
| Drowsiness | 1.24 | 1.55 | 1.80 | 1.87 | 0.73 | 1.01 | 0.197 |
| Sensitivity to light | 1.81 | 1.57 | 2.00 | 1.41 | 1.64 | 1.75 | 0.468 |
| Sensitivity to noise | 1.81 | 1.57 | 2.2 | 1.55 | 1.45 | 1.57 | 0.251 |
| Irritability | 1.24 | 1.79 | 1.8 | 2.35 | 0.73 | 0.90 | 0.654 |
| Sadness | 0.48 | 1.36 | 0.60 | 1.90 | 0.36 | 0.67 | 0.605 |
| Nervousness | 0.38 | 0.80 | 0.70 | 1.06 | 0.09 | 0.30 | 0.223 |
| Feeling more emotional | 0.76 | 1.64 | 1.00 | 2.16 | 0.55 | 1.04 | >0.999 |
| Numbness or tingling | 0.19 | 0.68 | 0.40 | 0.97 | 0.00 | 0.00 | 0.468 |
| Feeling slowed down | 1.05 | 1.43 | 1.50 | 1.72 | 0.64 | 1.03 | 0.349 |
| Feeling mentally foggy | 1.38 | 1.63 | 1.90 | 1.91 | 0.91 | 1.22 | 0.223 |
| Difficulty concentrating | 2.05 | 1.60 | 2.80 | 1.69 | 1.36 | 1.21 | 0.061 |
| Difficulty remembering | 0.86 | 1.46 | 1.00 | 1.89 | 0.73 | 1.01 | 0.756 |
| Visual problems | 1.19 | 1.72 | 2.10 | 1.97 | 0.36 | 0.92 | 0.024* |
p-value obtained from Independent samples Mann-Whitney U Test. No participants reported vomiting symptoms. *significant p-value <0.05
Discussion
This study aimed to investigate the effect of migraine on gait and balance plus self-reported symptoms in children with concussion. Concussed children with migraine experienced worse concussion symptoms than concussed children without migraine. However, concussed children with and without migraine performed similarly on walking tasks. Our findings support previous literature indicating that migraine symptoms are related to worse concussion recovery [17,22,29,30]. The FGA was not able to identify differences between those with and without migraine in children. In a cohort study of 600 male and female children aged 5-18 years. Rosenbaum PE et al., found that regardless of gender, concussed children with migraine delayed recovery compared to concussed children without migraine [31].
The FGA and PCSS test different domains affected by concussion and recovery may occur at different rates [8,32]. The results suggest that reported symptoms and functional performance tests are independent from each other in children with chronic concussion.
Participants with a wide range of concussion onset which was up to one year after injury were recruited, possibly affecting their gait and PCSS scores. Evidence suggests that balance may return to normal levels within few weeks [33,34]. A more acute sample may show differences between concussed children with and without migraine on the FGA. Others have more recently suggested that dual task walking may be more sensitive to identifying balance deficits in children postconcussion when utilising sensors [35,36].
Forty three percent of children with concussion reported migraine which is higher than percentages reported by previous studies that reported that 36% of children and young adults had migraine [25,37]. This difference can be explained by the ratio of male and female participants. In this study, female participants accounted for 66% of the sample while in other studies female participants were approximately one third of their samples [25,37]. The increased percentage of migraine in our sample can be explained by that fact that migraines are more common in females than males [38]. In the current study, the presence of migraine was assessed by asking the participant and/or their guardians. Furthermore, the migraine was not specified if it was acquired before or after the concussion injury. Future studies should use a confirmed diagnosis of migraine and document if migraine was acquired before or after concussion. Other factors has shown to influence migraine effects on concussed children such as familial history [22] and should also be considered in future studies. A main strength point of this study was the incorporation of an objective measure of functional performance using the FGA test and the subjective measure of symptoms severity using PCSS which allows for comparing between the patient’s complain and his/her functional impairments.
Because only 60% of the subjects completing the PCSS in the study, it may have decreased the ability to capture differences between the concussed children with and without migraine. Furthermore, the variability of the time since injury may have resulted in a heterogenic sample which further decreases the ability to find significant differences between groups.
Limitation(s)
Limitations of this study included the cross-sectional design that did not allow the study to assess differences of concussion recovery trajectory between concussed children with and without migraine. Another limitation is the small number of participants in the study that may have reduced the power of the study to detect significant differences between the groups. Furthermore, reduction in number of participants completing the PCSS test further decreased the power of this study.
Conclusion(s)
Although migraine symptoms did not show differences on gait performance, migraineur’s had worse fatigue and visual symptoms in children postconcussion. Gait and subjective symptoms appear to be testing two separate domains after concussion in children. Special considerations should be given when managing concussed children with migraine as they may show worse symptoms than concussed children without migraine.
p-value for all variable use independent samples t-test; for gender Chi-square test used; m=meter; kg=kilogram
p-value obtained from Independent samples Mann-Whitney U Test. No participants reported vomiting symptoms. *significant p-value <0.05
[1]. Langlois JA, Rutland-Brown W, Wald MM, The epidemiology and impact of traumatic brain injury: A brief overviewJournal of Head Trauma Rehabilitation 2006 21:375-78.10.1097/00001199-200609000-0000116983222 [Google Scholar] [CrossRef] [PubMed]
[2]. Mannix R, O’Brien MJ, Meehan WP, The epidemiology of outpatient visits for minor head injury: 2005 to 2009Neurosurgery 2013 73(1):129-34.10.1227/01.neu.0000429846.14579.4123615100 [Google Scholar] [CrossRef] [PubMed]
[3]. Lumba-Brown A, Yeates KO, Sarmiento K, Breiding MJ, Haegerich TM, Gioia GA, Centers for Disease Control and Prevention Guideline on the diagnosis and management of mild traumatic brain injury among childrenJAMA Pediatrics 2018 :172 [Google Scholar]
[4]. Broglio SP, Collins MW, Williams RM, Mucha A, Kontos AP, Current and emerging rehabilitation for concussion. A Review of the evidenceClin Sports Med [Internet] 2015 34(2):213-31.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2581871010.1016/j.csm.2014.12.00525818710 [Google Scholar] [CrossRef] [PubMed]
[5]. Kontos AP, Deitrick JMA, Collins MW, Mucha A, Review of vestibular and oculomotor screening and concussion rehabilitationJournal of Athletic Training 2017 52:256-61.10.4085/1062-6050-51.11.0528387548 [Google Scholar] [CrossRef] [PubMed]
[6]. Baldwin GT, Breiding MJ, Dawn Comstock R, Epidemiology of sports concussion in the United StatesIn: Handbook of Clinical Neurology 2018 :63-74.10.1016/B978-0-444-63954-7.00007-030482376 [Google Scholar] [CrossRef] [PubMed]
[7]. Zhang AL, Sing DC, Rugg CM, Feeley BT, Senter C, The rise of concussions in the adolescent populationOrthop J Sport Med [Internet] 2016 4(8):232596711666245Available from: http://journals.sagepub.com/doi/10.1177/232596711666245810.1177/232596711666245827579334 [Google Scholar] [CrossRef] [PubMed]
[8]. Iverson GL, Gardner AJ, Terry DP, Ponsford JL, Sills AK, Broshek DK, Predictors of clinical recovery from concussion: A systematic reviewBritish Journal of Sports Medicine 2017 51:941-48.10.1136/bjsports-2017-09772928566342 [Google Scholar] [CrossRef] [PubMed]
[9]. Alsalaheen BA, Whitney SL, Marchetti GF, Furman JM, Kontos AP, Collins MW, Relationship between cognitive assessment and balance measures in adolescents referred for vestibular physical therapy after concussionClin J Sport Med 2016 26(1):46-52.10.1097/JSM.000000000000018525706663 [Google Scholar] [CrossRef] [PubMed]
[10]. Reed N, Murphy J, Dick T, Mah K, Paniccia M, Verweel L, A multi-modal approach to assessing recovery in youth athletes following concussionJ Vis Exp [Internet] 2014 (91)Available from: http://www.jove.com/video/51892/a-multi-modal-approach-to-assessing-recovery-youth-athletes-following10.3791/5189225285728 [Google Scholar] [CrossRef] [PubMed]
[11]. Kelly KC, Jordan EM, Joyner AB, Burdette GT, Buckley TA, National Collegiate Athletic Association Division I athletic trainers’ concussion-management practice patternsJ Athl Train 2014 49(5):665-73.10.4085/1062-6050-49.3.2525188315 [Google Scholar] [CrossRef] [PubMed]
[12]. Sherry NS, Fazio-Sumrok V, Sufrinko A, Collins MW, Kontos AP, Multimodal assessment of sport-related concussionClin J Sport Med [Internet] 2019 Mar 18 Publish Ah. Available from: https://journals.lww.com/00042752-900000000-9906410.1097/JSM.000000000000074030908330 [Google Scholar] [CrossRef] [PubMed]
[13]. Henry LC, Elbin RJ, Collins MW, Marchetti G, Kontos AP, Examining recovery trajectories after sport-related concussion with a multimodal clinical assessment approachNeurosurgery [Internet] 2016 78(2):232-40.Available from: https://academic.oup.com/neurosurgery/article/78/2/232/245365810.1227/NEU.000000000000104126445375 [Google Scholar] [CrossRef] [PubMed]
[14]. O’Connor KL, Rowson S, Duma SM, Broglio SP, Head-impact-measurement devices: A systematic reviewJournal of Athletic Training 2017 52:206-27.10.4085/1062-6050.52.2.0528387553 [Google Scholar] [CrossRef] [PubMed]
[15]. O’Connor KL, Peeters T, Szymanski S, Broglio SP, Individual impact magnitude vs. cumulative magnitude for estimating concussion oddsAnn Biomed Eng 2017 45(8):1985-92.10.1007/s10439-017-1843-328455786 [Google Scholar] [CrossRef] [PubMed]
[16]. Mihalik JP, Register-Mihalik J, Kerr ZY, Marshall SW, McCrea MC, Guskiewicz KM, Recovery of posttraumatic migraine characteristics in patients after mild traumatic brain injuryAm J Sports Med 2013 41(7):1490-96.10.1177/036354651348798223696213 [Google Scholar] [CrossRef] [PubMed]
[17]. Kontos AP, Elbin RJ, Lau B, Simensky S, Freund B, French J, Posttraumatic migraine as a predictor of recovery and cognitive impairment after sport-related concussionAm J Sports Med [Internet] 2013 41(7):1497-504.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2369838910.1177/036354651348875123698389 [Google Scholar] [CrossRef] [PubMed]
[18]. Covassin T, Elbin RJ, Larson E, Kontos AP, Sex and age differences in depression and baseline sport-related concussion neurocognitive performance and symptomsClin J Sport Med 2012 22(2):98-104.10.1097/JSM.0b013e31823403d222246342 [Google Scholar] [CrossRef] [PubMed]
[19]. Nelson LD, Guskiewicz KM, Barr WB, Hammeke TA, Randolph C, Ahn KW, Age differences in recovery after sport-related concussion: A comparison of high school and collegiate athletesJ Athl Train 2016 51(2):142-52.10.4085/1062-6050-51.4.0426974186 [Google Scholar] [CrossRef] [PubMed]
[20]. Dougan BK, Horswill MS, Geffen GM, Athletes’ age, sex, and years of education moderate the acute neuropsychological impact of sports-related concussion: A meta-analysisJ Int Neuropsychol Soc 2014 20(1):64-80.10.1017/S135561771200146423375058 [Google Scholar] [CrossRef] [PubMed]
[21]. Covassin T, Schatz P, Swanik CB, Sex differences in neuropsychological function and postconcussion symptoms of concussed collegiate athletesNeurosurgery [Internet] 2007 61(2):345-50.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1776274710.1227/01.NEU.0000279972.95060.CB17762747 [Google Scholar] [CrossRef] [PubMed]
[22]. Sufrinko A, McAllister-Deitrick J, Elbin R, Collins MW, Kontos AP, Family history of migraine associated with posttraumatic migraine symptoms following sport-related concussionJ Head Trauma Rehabil [Internet] 2018 [cited 2020 Dec 31] 33(1):07-14.Available from: http://journals.lww.com/00001199-201801000-0000210.1097/HTR.000000000000031528520665 [Google Scholar] [CrossRef] [PubMed]
[23]. Olesen J, Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd editionCephalalgia [Internet] 2018 38(1):01-211.Available from: http://journals.sagepub.com/doi/10.1177/033310241773820210.1177/0333102417738202 [Google Scholar] [CrossRef]
[24]. Gordon KE, Dooley JM, Wood EP, Is migraine a risk factor for the development of concussion?British Journal of Sports Medicine 2006 40:184-85.10.1136/bjsm.2005.02225116432009 [Google Scholar] [CrossRef] [PubMed]
[25]. Eckner JT, Seifert T, Pescovitz A, Zeiger M, Kutcher JS, Is migraine headache associated with concussion in athletes? A case-control studyClin J Sport Med 2017 27(3):266-70.10.1097/JSM.000000000000034627428679 [Google Scholar] [CrossRef] [PubMed]
[26]. Faul F, Erdfelder E, Lang AG, Buchner A, Faul F, Erdfelder E, G*Power 3: A flexible statistical power analysis program for the social, behavioral, and social, behavioral, and biomedical sciencesJ Mater Environ Sci 2007 39(2):175-91.10.3758/BF0319314617695343 [Google Scholar] [CrossRef] [PubMed]
[27]. Wrisley DM, Marchetti GF, Kuharsky DK, Whitney SL, Reliability, internal consistency, and validity of data obtained with the functional gait assessmentPhys Ther [Internet] 2004 84(10):906-18.Available from: https://academic.oup.com/ptj/article/84/10/906/285751810.1093/ptj/84.10.90615449976 [Google Scholar] [CrossRef] [PubMed]
[28]. Iverson GL, Lovell MR, Collins MW, Interpreting change on impact following sport concussionClin Neuropsychol [Internet] 2003 17(4):460-67.Available from: http://www.ncbi.nlm.nih.gov/pubmed/1516891110.1076/clin.17.4.460.2793415168911 [Google Scholar] [CrossRef] [PubMed]
[29]. Mihalik JP, Stump JE, Collins MW, Lovell MR, Field M, Maroon JC, Posttraumatic migraine characteristics in athletes following sports-related concussionJ Neurosurg 2005 102(5):850-55.10.3171/jns.2005.102.5.085015926709 [Google Scholar] [CrossRef] [PubMed]
[30]. Heyer GL, Young JA, Rose SC, McNally KA, Fischer AN, Post-traumatic headaches correlate with migraine symptoms in youth with concussionCephalalgia [Internet] 2015 36(4):309-16.Available from: http://journals.sagepub.com/doi/10.1177/033310241559024010.1177/033310241559024026054363 [Google Scholar] [CrossRef] [PubMed]
[31]. Rosenbaum PE, Locandro C, Chrisman SPD, Choe MC, Richards R, Pacchia C, Characteristics of pediatric mild traumatic brain injury and recovery in a concussion clinic populationJAMA Netw open 2020 3(11):e202146310.1001/jamanetworkopen.2020.2146333196804 [Google Scholar] [CrossRef] [PubMed]
[32]. Kamins J, Bigler E, Covassin T, Henry L, Kemp S, Leddy JJ, What is the physiological time to recovery after concussion? A systematic reviewBr J Sports Med [Internet] 2017 51(12):935-40.Available from: https://bjsm.bmj.com/lookup/doi/10.1136/bjsports-2016-09746410.1136/bjsports-2016-09746428455363 [Google Scholar] [CrossRef] [PubMed]
[33]. Purkayastha S, Adair H, Woodruff A, Ryan LJ, Williams B, James E, Balance testing following concussion: Postural sway versus complexity indexPM R 2019 11(11):1184-92.10.1002/pmrj.1212930729729 [Google Scholar] [CrossRef] [PubMed]
[34]. Teel EF, Marshall SW, Shankar V, McCrea M, Guskiewicz KM, Predicting recovery patterns after sport-related concussionJ Athl Train 2017 52(3):288-98.10.4085/1062-6050-52.1.1228387552 [Google Scholar] [CrossRef] [PubMed]
[35]. Howell DR, Mayer AR, Master CL, Leddy J, Zemek R, Meier TB, Prognosis for persistent post concussion symptoms using a multifaceted objective gait and balance assessment approachGait Posture [Internet] 2020 79:53-59.Available from: http://www.ncbi.nlm.nih.gov/pubmed/3236112510.1016/j.gaitpost.2020.04.01332361125 [Google Scholar] [CrossRef] [PubMed]
[36]. Howell DR, Bonnette S, Diekfuss JA, Grooms DR, Myer GD, Wilson JC, Dual-task gait stability after concussion and subsequent injury: An exploratory investigationSensors (Switzerland) 2020 20(21):01-13.10.3390/s2021629733167407 [Google Scholar] [CrossRef] [PubMed]
[37]. Seifert T, Sufrinko A, Cowan R, Scott Black W, Watson D, Edwards B, Comprehensive headache experience in collegiate student-athletes: An initial report from the NCAA headache task forceHeadache 2017 57(6):877-86.10.1111/head.1310428480575 [Google Scholar] [CrossRef] [PubMed]
[38]. Vetvik KG, MacGregor EA, Sex differences in the epidemiology, clinical features, and pathophysiology of migraineLancet Neurol [Internet] 2017 16(1):76Available from: https://linkinghub.elsevier.com/retrieve/pii/S147444221630293910.1016/S1474-4422(16)30293-9 [Google Scholar] [CrossRef]