Lower abdominal oncological surgeries include a wide variety of surgical procedures such as surgeries for colorectal cancers, gynaecological malignancies, debulking of tumours and radical pelvic surgeries. These lead to significant postoperative pain, if uncontrolled produces a wide range of detrimental effects. Control of pathophysiological process associated with acute postoperative pain has shown to attenuate the stress response, thus causing improvement in postoperative morbidity, mortality and patient related outcomes [1,2].
In postoperative multimodal approach, epidural analgesia is an integral part because of superior analgesia and physiological benefits [3]. It benefits by obtunding the stress response and providing pain relief thus improving the quality of patient recovery and reducing the incidence of adverse outcomes [4]. Lumbar epidural has found to be effective in major abdominal surgeries [5]. As the spinal cord typically terminates at L1 level, lumbar epidural catheter can be safely placed [6].
Analgesia delivered through an indwelling epidural catheter is a safe and effective method for management of acute postoperative pain. Intraoperative use of the epidural catheter as part of a combined epidural-general anaesthesia technique results in less pain and faster patient recovery immediately after surgery [3]. Ropivacaine is a long-acting regional anaesthetic that is structurally related to Bupivacaine. It is a pure S(-) enantiomer, unlike Bupivacaine, which is a racemate, developed for the purpose of reducing potential toxicity and improving relative sensory and motor block profiles [7].
A randomised double blinded study done by Sawhney KY et al., compared the efficacy of bupivacaine, ropivacaine with or without fentanyl as epidural infusions in lower limb surgeries and concluded that ropivacaine offers superior analgesia than other groups [8].
However, this study was aimed to compare pain relief and patient comfort in patients undergoing lower abdominal oncological surgeries. Primary outcome measured was rescue analgesic requirement in first 24 hours of postoperative period whereas pain scores and changes in haemodynamic parameters were the secondary outcomes measured.
Materials and Methods
After obtaining approval from Institutional Ethics Committee (Ref. no: KMIO/MEC/019/23.March.2017), this randomised clinical trial was conducted from September 2016 to May 2018 in the Department of Anaesthesiology in Kidwai Cancer Institute, Bengaluru, Karnataka, India.
Inclusion and Exclusion criteria: Patient of ASA grade I and II of age group between 18-70 years with BMI between 18-30 kg/m2 were included in the study. Patients with coagulopathy, localised infection at the proposed site, inability to comprehend the scoring systems, known allergy to drugs used, opioid dependence, renal, hepatic or cardiorespiratory impairment or any neurological disorder were excluded.
Sample size calculation: The sample size was calculated keeping the power of study at 80%, confidence interval of 95% and an alpha error of 0.05. Accordingly total sample size calculated was 70, which was divided into two groups of 35 patients each.
A random number table for 70 patients was divided into two groups based on computer generated randomisation table. The changes in haemodynamic variable as well as Visual Analogue Scale (VAS) score was recorded in both intraoperative and postoperative period. The description of VAS score was explained to the patient prior to giving the block.
The two groups were as follows:
Group R: Patients who received 0.2% Ropivacaine (n=35) at 5 mL/hour as epidural infusion in postoperative period.
Group RF: Patients who received 0.2% Ropivacaine with 2 mcg/mL fentanyl (n=35) at 5 mL/hour as epidural infusion in postoperative period.
Study Procedure
Seventy patients posted for elective lower abdominal oncological surgeries were enrolled for the study after obtaining a written consent from them. A detailed history, comprehensive general and systemic examination were carried out and documented. As per the institutional protocol, the patients were explained about the epidural technique, simultaneously patients were familiarised with a 10 cm VAS for pain intensity assessment and to request for rescue analgesics [9].
Epidural catheter was secured at T12-L1/L1-L2 prior to administration of general anaesthesia. General anaesthesia was administered as per institutional protocol. Before surgical incision the patients were administered epidural 8 mL of either 0.2% Ropivacaine or 0.2% Ropivacaine with fentanyl 2 μg/mL according to the randomisation table. Haemodynamic parameters were noted at 0, 5, 10, 15 and at every 30 minutes interval till the end of surgery. If the surgery lasted for more than 2 hours, patients were given additional 4 mL of the study drug epidurally. Upon arrival in SICU, patients were asked to rate their pain severity on the VAS for baseline VAS scores. Irrespective of the VAS score, patients were started on epidural infusion with study drug group that they belonged to at a rate of 5 mL/hr. The VAS scores and haemodynamic parameters were reassessed at 1, 2, 4, 6, 12, 18 and 24 hours of postoperative period. Patients with VAS score >4 were given 8 mL of epidural bolus as rescue analgesic. Patients with VAS score >6 were also given Inj. Paracetamol 1 gm IV along with the bolus dose. Number of rescue analgesics received was noted.
Statistical Analysis
Descriptive and Inferential statistical analysis has been carried out in the present study. Significance is assessed at 5% level of significance. Student t-test (two-tailed, independent), Leven’s test, Chi-square/Fisher-Exact test, Nonparametric tests were used according to the group variables. The p-value <0.05 was considered to be significant. The Statistical software Statistical Package for the Social Sciences (SPSS) 18.0 and R environment version 3.2.2 were used for the data analysis.
Results
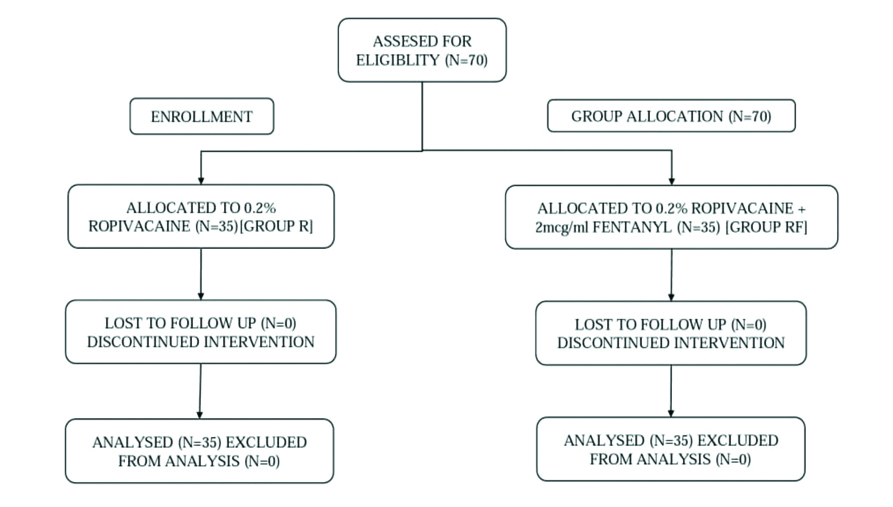
The study population comprised of 70 patients posted for elective lower abdominal oncosurgeries and was allocated into two groups of 35 patients each as shown in [Table/Fig-1].
Enrollment of patients in groups.
The two groups were similar with regard to demographic characteristics like age, BMI, and ASA physical grade [Table/Fig-2]
Demographic characteristics and operative data.
| Characteristics | Group R | Group RF | p-value |
|---|
| Age (Years) (Mean±SD) | 50.91±10.94 | 47.34±10.72 | 0.172 |
| BMI (kg/m2) (Mean±SD) | 21.86±1.48 | 22.23±2.35 | 0.424 |
| ASA (I:II) | 6:29 | 10:25 | 0.255 |
BMI: Body mass index; SD: Standard deviation; p-value <0.05 significant; ASA: American society of anaesthesiologists
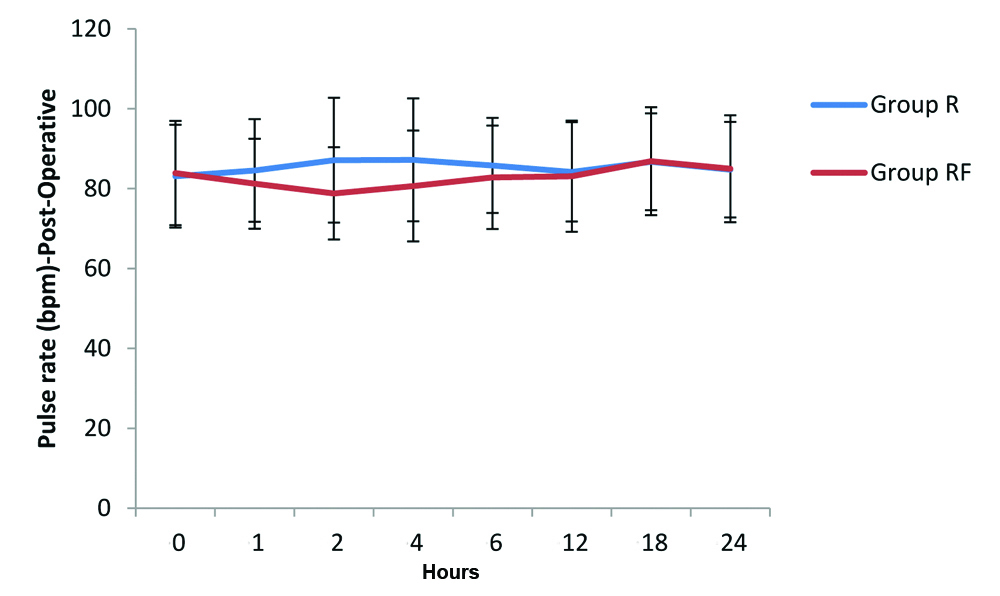
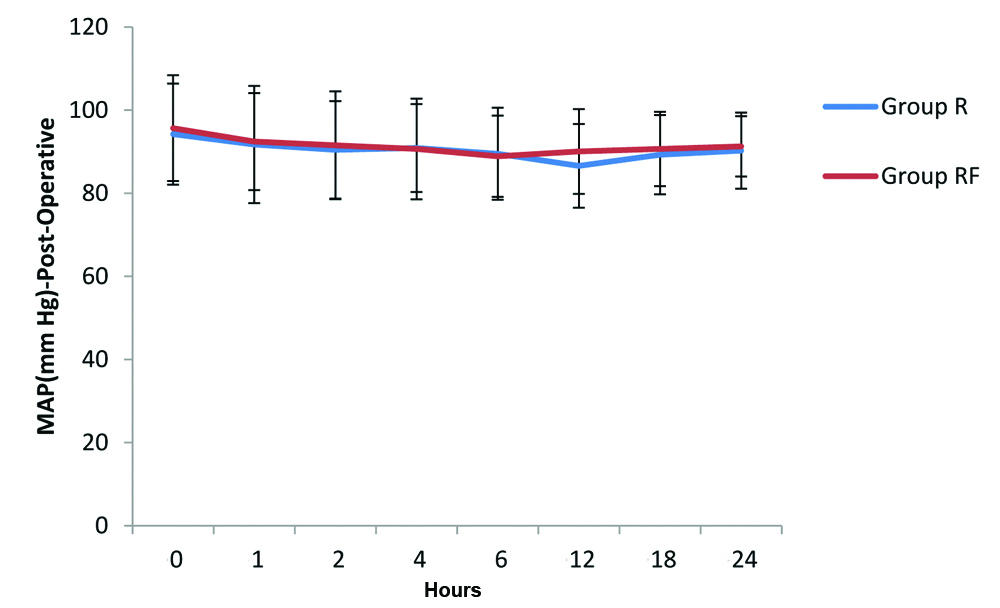
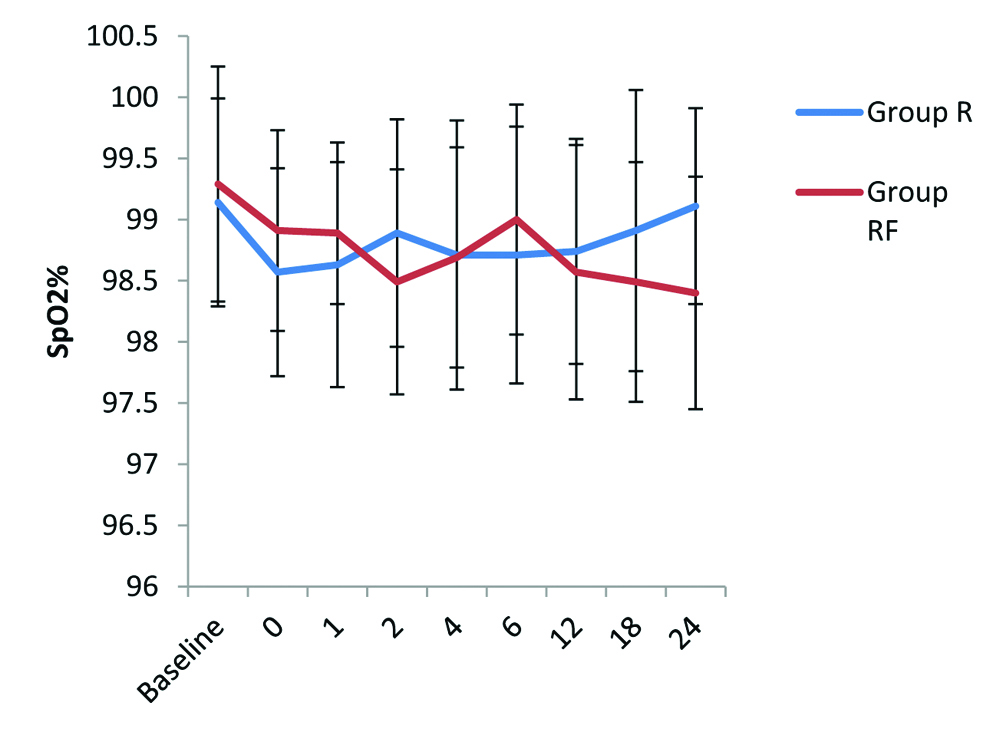
Haemodynamic parameters such as Pulse Rate (PR), Mean Arterial Pressure (MAP) and Oxygen Saturation (SpO2) postoperatively were comparable among the two groups at 0, 1, 2, 4, 6, 12, 18 and 24 hours of postoperative period.
[Table/Fig-3] shows the comparison of PR (beats/minute) among the groups at 0, 1, 2, 4, 6, 12, 18 and 24 hours of postoperative period. The analysis of variance showed that there was no significant (p-value >0.05) difference in HR among the groups at all the time periods.
Comparison of PR (beats/minute) among the groups.
[Table/Fig-4] shows the comparison of MAP among the groups at 0, 1, 2, 4, 6, 12, 18 and 24 hours of postoperative period. The analysis of variance showed that there was no significant (p-value >0.05) difference in MAP among the groups at all the time periods.
MAP (mmHg)- Comparison in two groups.
The baseline SpO2% between the groups R and RF was not statistically significant (p>0.05). The SpO2% found to be more in group R at 24th hour postoperatively compared to SpO2% of group RF with significant p-value (p<0.05). However, above finding is clinically insignificant [Table/Fig-5].
Comparison of SpO2 among the groups.
The mean VAS scores were higher in group R compared to group RF at 0,2,4,12,18 and 24 hours but the observed difference in both the groups was not statistically significant (p>0.05) except at 1 and 6 hours [Table/Fig-6].
VAS SCORE- Comparison in two groups of patients studied.
| Postoperative period (In hours) | VAS score | p-value# |
|---|
| Group R | Group RF |
|---|
| 0 | 5.14 | 5.4 | 0.601 |
| 1 | 4.26 | 3.09 | 0.016 |
| 2 | 3.6 | 3.2 | 0.223 |
| 4 | 3.63 | 3.43 | 0.518 |
| 6 | 4.03 | 3.31 | 0.024 |
| 12 | 3.43 | 3.14 | 0.353 |
| 18 | 3.77 | 3.66 | 0.766 |
| 24 | 3.26 | 3 | 0.217 |
#Student t-test (two tailed, independent)
All patients in group R required epidural boluses as rescue analgesics whereas 5.7% patients in group RF did not require any epidural boluses as rescue analgesics in the study period. The difference between Group R and Group RF in requirement of epidural boluses as rescue analgesic was statistically significant (p=0.007).
In Group R, 20% and in group RF 42.9% of patients did not required Inj. Paracetamol as additional rescue analgesics in the study period. The number of patients requiring epidural boluses and additional Inj. Paracetamol as rescue analgesics were higher in group R compared to group RF which was statistically significant (p=0.022) [Table/Fig-7].
Comparison for requirement of rescue analgesics.
| Variable | Group R | Group RF | p-value$ |
|---|
| No. of epidural bolus |
| 0 | 0 (0%) | 2 (5.7%) | 0.007 |
| 1 | 9 (25.7%) | 10 (28.6%) |
| 2 | 14 (40%) | 21 (60%) |
| 3 | 11 (31.4%) | 1 (2.9%) |
| 4 | 1 (2.9%) | 1 (2.9%) |
| No. of PCT+epidural bolus |
| 0 | 7 (20%) | 15 (42.9%) | 0.022 |
| 1 | 21 (60%) | 19 (54.3%) |
| 2 | 7 (20%) | 1 (2.9%) |
$Fisher-exact test; PCT: Paracetamol
Discussion
Overall, patients in Group R had higher VAS scores compared to patients in Group RF. Patients in group R required more number of rescue analgesics in the form of epidural boluses and Inj. Paracetamol in comparison with group RF which was statistically significant (p<0.05). In this study, group R and group RF were comparable with respect to PR, MAP and SpO2. Similar findings were observed in the study conducted by Khanna A et al., [10].
Parate LH et al., compared the effect of addition of low dose fentanyl to epidural 0.5% bupivacaine in 70 patients undergoing elective caesarian section [11]. The pain assessment was done using VAS and it was found that addition of fentanyl to epidural bupivacaine significantly reduces the VAS scores and prolongs the duration of postoperative analgesia.
Another study done by Kampe S et al., showed similar results where epidural infusion of 0.1% Ropivacaine with and without Sufentanyl 1 mcg/mL in patients undergoing elective total hip replacement under general anaesthesia [12]. Patients receiving Ropivacaine with Sufentanyl required six times less rescue analgesics over 48 hour infusion period.
In a study conducted by Suzuki A et al., 30 patients undergoing thoracic surgery were evaluated for effectiveness of 0.2% Ropivacaine and 1.67 mcg/mL Fentanyl [13]. It was concluded that patients receiving epidural infusion 0.2% Ropivacaine and 1.67 mcg/mL Fentanyl had decreased postoperative pain with stable vital signs which was similar to the present study.
A randomised double blinded study done by Sawhney KY et al., compared the efficacy of bupivacaine, ropivacaine with or without fentanyl as epidural infusions in lower limb surgeries and concluded that ropivacaine offers superior analgesia than other groups [8]. Similar results were observed in this study as ropivacaine with fentanyl is superior compared to ropiovacaine alone for postoperative analgesia.
Another randomised study done by Tomaszek L et al., comparing Ropivacaine with fentanyl and Bupivacaine with fentanyl for pain control in children after thoracic surgery found no difference in pain scores between two groups [14]. The results of this study differ with ropivacaine in addition to fentanyl is better compared to ropivacaine for adult patients undergoing elective gynaecological oncosurgeries.
The principle site of action for neuraxial blockade is believed to be the nerve root. Local anaesthetic is injected into the epidural space containing nerve root. Larger volumes and quantities of local anaesthetic molecules are needed for epidural block [15]. Blockade of neural transmission in the posterior nerve root fibers interrupts somatic and visceral sensation, whereas blockade of anterior nerve root fibers prevents efferent motor and autonomic outflow [6].
The dose of ropivacaine for postoperative analgesia was selected according to potency ratio and the recommendation in the literature which was 0.2% ropivacaine [16]. It was observed that the addition of fentanyl had a stronger effect than the local anaesthetic alone. The benefit and sparing effect of local anaesthetic by the use of fentanyl is well known [17]. Addition of opioids to improve the quality of postoperative epidural analgesia with ropivacaine, as found in the present study [18].
Limitation(s)
This study was not double blinded and was not designed for cost analysis. Study was limited only to ASA I and ASA II grade.
Conclusion(s)
It can be concluded that when 0.2% Ropivacaine and 0.2% Ropivacaine with 2 mcg/mL Fentanyl are administered in equal volumes epidurally for lower abdominal oncological surgeries, 0.2% Ropivacaine with 2 mcg/mL Fentanyl has good postoperative analgesia and less requirement of rescue analgesics compared to 0.2% Ropivacaine.
BMI: Body mass index; SD: Standard deviation; p-value <0.05 significant; ASA: American society of anaesthesiologists
#Student t-test (two tailed, independent)
$Fisher-exact test; PCT: Paracetamol