Introduction
The word ‘Disaster’ is derived from Middle French désastre and that from Old Italian disastro, coming from the Greek pejorative prefix δυσ-, (dus-) “bad”+ αστήρ (aster), “star”. The genesis of this word belongs to the astrological theme in which the destruction or deconstruction of a star used to be considered a disaster. A disaster can be defined as a sudden, calamitous event that seriously disrupts the functioning of a community or society and causes human, material, and economic or environmental losses that exceed the community’s or society’s ability to cope using its resources. The combination of hazards, vulnerability and inability to reduce the potential negative consequences of risk results in disaster.
Magnitude of Disaster: Global and India Level
In the second half of the 20th century, around 200 natural disasters struck different parts of the world and claimed the lives of around 1.4 million people. However, the losses due to natural disasters were around 20 times greater in developing countries than in developed countries [1]. Asia being the biggest continent tops the list of deaths due to natural disasters. India is vulnerable, in varying degrees, to a large number of natural as well as man-made disasters. A 58.6% of the landmass is prone to earthquakes of moderate to very high intensity; over 40 million hectares (12% of land) is prone to floods and river erosion; of the 7,516 km long coastline, close to 5,700 km is prone to cyclones and tsunamis; 68% of the cultivable area is vulnerable to drought and hilly areas are at risk from landslides and avalanches [2]. Vulnerability to disasters/emergencies of Chemical, Biological, Radiological and Nuclear (CBRN) origin also exists. Heightened vulnerabilities to disaster risks can be related to expanding population, urbanisation and industrialisation, development within high-risk zones, environmental degradation and climate change.
Disaster Management: Global Level and India Level
The first major development at global level in this direction was the Yokohama Strategy for a Safer World: Guidelines for Natural Disaster Prevention, Preparedness and Mitigation and its Plan of Action [3], which was adopted in 1994. Followed by it was the Hyogo Framework for Action 2005-2015 [4], which emphasised on Building the Resilience of Nations and Communities to Disasters. The Sendai Framework for Disaster Risk Reduction (2015–2030) [5] was adopted in 2015 in the Third United Nations (UN) World Conference on Disaster Risk Reduction, held in Sendai, Miyagi, Japan. These action frameworks had representation from States Members of the UN in partnership with Non Governmental Organisations (NGO), International Organisations, the scientific community, business, industry, and the media. India is a signatory in this framework and works closely with United Nations International Strategy for Disaster Reduction (UNISDR) to implement the priority areas of these frameworks.
After the UN General Assembly declared the1990s decade as ‘International Decade for Natural Disaster Reduction’, a disaster management cell was established in India under the Ministry of Agriculture. After 9 years i.e., in 1999, a High-Powered Committee (HPC) was constituted to review the existing arrangement for preparedness and mitigation of natural disasters. In 2002, the disaster management division which was established under the Ministry of Agriculture was shifted to the Ministry of Home Affairs. The HPC submitted its report on the aforementioned matter in October 2001. Following this report of HPC, the Government of India enacted the Disaster Management Act on 23rd December 2005 [6].
Hospital Safety and Quality
The Pan American Health Organisation (PAHO) and the World Health Organisation (WHO) have defined: “a safe hospital as one that will not collapse in disasters, killing patients and staff; can continue to function and provide its services as a critical community facility when it is most needed; and, is organised, with contingency plans in place and health workforce trained to keep the network operational [7]". A multi-specialty and well-equipped hospital holds an enormous amount of investment. Its destruction during disaster poses a major economic burden for the affected society. Making hospitals safe from natural disasters requires the multidisciplinary expertise of a variety of experts, from engineers to architects to administrators and others.
Quality refers to the medical care quality and the non medical aspects of service delivery to the consumer. For example like infection control practices comprise of medical quality while reducing waiting time for patients, staff communication and attitude comprise of non medical aspects. According to Joseph Juran it means “fitness for use”, Philip Crosby called it “conformance to requirements.” The parent body for quality management in India is the Quality Council of India (QCI). It was created as an autonomous non profit organisation through other supporting associations, like ASSOCHAM, CII and FICCI, registered under the Societies Registration Act of 1860. Its main purpose was to establish an accreditation structure in the country and to spread quality movement in India by undertaking a National Quality Campaign [8]. The various areas of accreditation include environment, food safety, healthcare, and education. Healthcare providers and NABH is a constituent board of QCI, which was established in 2006 with the purpose to establish and operate accreditation programme for healthcare organisations in India and abroad. It guides the hospital regarding the provision of a safe and secure environment for patients, their families, staff, and visitors. The standards ask the organisation to take steps to ensure this, including proactive risk mitigation measures like conducting regular facility inspection rounds, mock drills for fire and non fire emergencies. A comparative study of three NABH Accredited and three non-NABH Accredited Hospitals in Jaipur was conducted in 2015. The study concluded that “NABH Accreditation” has emerged as an effective tool to improve the efficiency and effectiveness of hospital services and facilities [9].
Rationale for the Study
The NABH discusses (chapter 8) structural, non structural and functional elements related to hospital infrastructure, building conditions, construction guidelines, provision of support services, policies and procedures for hospital safety committee and safety plans for various types of emergencies. Their implementation ensures that the hospital is imparting training and conducting drills with the hospital staff to sensitise and prepare them for the disaster situation. Kapurkar KS et al., conducted a study to assess the effectiveness of the plan teaching programme on NABH guidelines among newly recruited staff nurses at Krishna Hospital, Karad, Maharashtra, India. The study concluded that the majority of the newly recruited nursing staff had 19.38% average knowledge and 17.85% had average practice towards NABH guidelines [10]. The study also found that the difference in Knowledge and Practice scores of newly recruited nursing staff between the pretest and post-test was highly significant.
The hospital has to demonstrate its preparedness through documented policies and procedures, by having patient and staff safety measures in place all around the hospital. Very few and scattered evaluative studies are conducted till now to identify the effectiveness of Standard Operating Procedure (SOPs) in the management of Mass Casualty Incidents (MCIs). One such was conducted in 2007 in 22 hospitals of Israel by Adini B et al., [11]. NABH assessment does not speak about the practices of hospital staff towards disaster preparedness and response e.g., admission process, discharge, treatment, billing, clinical assessment, etc. Measuring disaster preparedness of hospitals is not undertaken by the NABH assessment. The assessment team only provides suggestions as per the evidence-based, best practices to improve safety in total and make the hospitals disaster resilience.
By measuring disaster preparedness the ultimate benefit will be for the patient, hospital staff, and community in the primary and tertiary catchment area. In case the said hospital is a referral centre, it will benefit the patients even in the tertiary catchment area of the hospital. It will provide moral and psychological support to the population it serves will be huge benefit for the investors, Public Sector Undertakings (PSUs), and government who have made a capital investment in developing the hospital. A considerable amount of research studies is available to understand the effect of disaster and the various factors related to its management by the healthcare staff. But there are no studies that present evidence of the effect of accreditation on disaster management.
This research has analysed the hospital infrastructure and processes, as well as the structural and non structural elements of the hospital. These aspects were studied in the light of the hazards faced by the hospitals owing to their geographical and socio-political location. The research helped in understanding how NABH accreditation affects practices of medical staff towards disaster preparedness and response and what was the level of disaster preparedness and response of NABH accredited hospitals of north India. The study objective was to assess the influence of NABH accreditation on disaster preparedness and response of accredited hospitals of north India.
Materials and Methods
It was a quantitative, cross-sectional, ex-post-facto study. The study was conducted in a hospital located in north India, six north Indian states including the National Capital Territory (NCT) of Delhi. The states included Haryana, Himachal Pradesh (HP), Uttarakhand, Uttar Pradesh (UP) and Punjab. These states are affected by common types of natural disaster like earthquakes, landslides, floods and drought and have numerous NABH accredited multispeciality hospitals.
The approximate number of hospitals that had NABH accreditation as of April 2016 in north India was 113. The research study was approved by Institutional review board and ethics committee of IIHMR University, Jaipur, Rajasthan, India (with registration number IORG0007355) on 29th July 2017. The study period was August 2017 to March 2018 and duration of the study was nine months.
Informed consent was obtained from the participants after explaining the risks and benefits of the study. Information of the participants was kept confidential by assigning alphabetic coding to them.
Inclusion and Exclusion criteria: The hospitals varied in characteristic like bed strength, speciality offered (broad/super speciality), level of care, the scope of services offered, etc. Therefore, to maintain homogeneity of sample hospitals, the following criteria were established for selecting the hospitals:
Hospitals with more than 100 beds were selected for the study.
Hospitals with a single super speciality like Oncology, Cardiology, Liver and Biliary, Orthopaedics and Spine, etc., were excluded.
Hospitals with more than 18 months (one surveillance audit) of NABH accreditation were included
A homogenous group of 39 hospitals was drawn based on the above-mentioned inclusion and exclusion criteria. The study sample population were admitted to these hospitals. A 20% of hospitals (rounded off to 10 hospitals) were selected to draw the study sample from the target population. The researchers could collect data from nine hospitals in this study due to no participation from the state of Punjab. Participation in the study was voluntary and non remunerative, and participants were free to withdraw or refuse to provide information at any point of time without any hesitation or fear. A survey instrument was used for capturing the hazard profile and preparedness of the sample. The hazard faced by the hospitals were recorded in terms of No Hazard (N), Low Hazard (L), Average Hazard (A) and High Hazard (H). A three-point scale (low, average and high) was used to rate the hospital preparedness on predefined criteria. The numerical rating was given, where low was equivalent to 0, average was 1 and high level of preparedness was given a score of 2. For a hospital to be highly prepared they must score 2 in all the criteria.
Statistical Analysis
Statistical Package for the Social Sciences (SPSS) Version 22.0 was used for statistical analysis purpose.
Results
The state-wise participation in the study was three from the state of Delhi, two from Haryana, two from UP, one each from Uttarakhand and Himachal Pradesh. The bed strength of hospitals varied from 162 to 400 with average bed occupancy of 77%. The hospital from UP had the lowest bed occupancy of 45-50% while that of Delhi and Haryana reported the highest occupancy of 85% per annum. As per the best practices all hospitals should prepare themselves to expand up to 10% of the functional bed capacity. This expandable number of beds is called the surge capacity of any hospital. It includes the beds in the medicine and surgical wards, as well as in Intensive Care Units (ICUs). At any given point of time, an emergency Operation Theatre (OT) should also be available to cater to the needs of patients requiring immediate surgical intervention. [Table/Fig-1] depicts the demographic details of the participating hospitals.
Demographic details of the participating hospitals.
| Variables/States | Haryana | UP | UP | Delhi | Delhi | Delhi | HP | Uttarakhand | Haryana |
|---|
| Year of establishment | 2000 | 1969 | 2016 | 2007 | 2005 | 1991 | 2012 | 2012 | 2007 |
| No. of beds | 300 | 300 | 250 | 162 | 200 | 400 | 100 | 205 | 400 |
| Occupancy | 75% | 45-50% | 40-50% | 80% | 80% | 85% | 65% | 70% | 85% |
| Hospital capacity | 30 | 15 | 13 | 10 | 20 | 40 | 8 | 20 | 40 |
| Medicine specialities | 15 | 8 | 6 | 5 | 12 | 28 | 4 | 12 | 30 |
| Surgical specialities | 12 | 4 | 4 | 3 | 6 | 8 | 2 | 6 | 6 |
| Intensive care | 3 | 3 | 3 | 2 | 2 | 4 | 2 | 2 | 4 |
| OTs | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Surge capacity | 30 | 15 | 13 | 10 | 20 | 40 | 8 | 20 | 40 |
The hazard profiling of north Indian states was carried out using a standardised tool. The number of hazard elements in each hazard category is presented in [Table/Fig-2] for the north Indian states. Facility visit and interview of stakeholders was done along with a review of state hazard profiles.
Hazard profile of the participating hospitals in north Indian states.
| Hazard score/States | Haryana | UP | UP | Delhi | Delhi | Delhi | HP | Uttarakhand | Haryana |
|---|
| No hazard (n) | 9 | 11 | 14 | 14 | 14 | 14 | 4 | 3 | 11 |
| Low hazard (n) | 8 | 9 | 7 | 7 | 7 | 7 | 6 | 5 | 3 |
| Ave. hazard (n) | 6 | 3 | 2 | 2 | 2 | 2 | 8 | 4 | 9 |
| High hazard (n) | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 11 | 0 |
| Total | 23 | 23 | 23 | 23 | 23 | 23 | 23 | 23 | 23 |
n=number of hazard elements
The hospitals of Haryana, UP and Delhi have categorised the potential hazards in the category of low [8] and average [6] hazards only, which include earthquakes, draught and heatstroke. The average hazard type includes fire, explosion, epidemic, contamination, population gathering and hazardous material spillage. However, the hospitals in the state of HP and Uttarakhand have categorised the potential hazards in the high hazard [11] category also, besides the other categories, which include earthquakes, landslides, unstable slopes, torrential rains etc. These hospitals have categorised displaced population, epidemics, explosions, population gathering and hazardous material spillage in the low hazard [5] category, while contamination, infestations, torrential rains and fires are categorised as average [4] category hazards for these two states.
The [Table/Fig-3] presents the safety levels of participating hospitals along with the safety percentages. One hospital in UP was found lowest in criteria requiring high preparedness reported it at 12%. The attributable factors were the age of the hospital i.e., the hospital was established in 1969 and had old and aging infrastructure, equipment and facilities.
Safety levels among hospitals.
| Variables/States | Haryana | UP | UP | Delhi | Delhi | Delhi | HP | Uttarakhand | Haryana |
|---|
| Hospital codes | A | B | C | D | E | F | G | H | I |
| Year of establishment | 2000 | 1969 | 2016 | 2007 | 2005 | 1991 | 2012 | 2012 | 2007 |
| Safety level low% | 2 | 36.9 | 4.6 | 3.2 | 1.6 | 1.6 | 12.3 | 1.5 | 1.5 |
| Safety level average% | 46 | 50.8 | 38.2 | 26.4 | 14.0 | 4.6 | 56.9 | 10.8 | 6.2 |
| Safety level high% | 52 | 12.3 | 57.2 | 70.4 | 84.4 | 93.8 | 30.8 | 87.7 | 92.3 |
Analysis of Hospital Preparedness
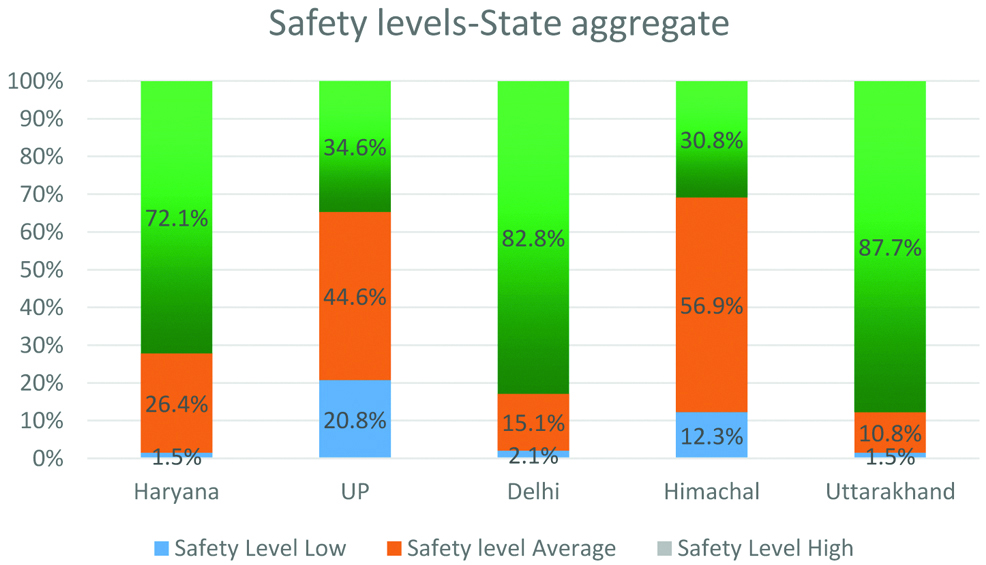
A structured, pretested questionnaire was used for measuring the state-wise preparedness. [Table/Fig-4] presents the state-wise safety levels. The state with the highest preparedness was reported by hospitals in the state of Uttarakhand, followed by Haryana and Delhi. The state of Himachal Pradesh reported average preparedness followed by the state of UP.
State-wise safety levels.
The preparedness of the healthcare organisations was studied under two categories which had elements related to the following:
Procedural preparedness elements related categories include:
Organisation of the Hospital Disaster Committee and the Emergency Operations Centre
Operational plan for internal or external disasters
Contingency plans for medical treatment in disasters
Plans for the operation, preventive maintenance, and restoration of critical services
Availability of medicines, supplies, instruments, and other equipment for use in emergency
Structural and non structural elements related categories include:
Prior events affecting hospital safety
Safety of the structural system and type of materials used in the building
Elements of non structural safety of the building.
Architectural elements
The organisations in the state of Haryana, Delhi and Uttarakhand were found highly prepared in the elements related to functional and effective disaster management committee along with effective emergency operation centre in the hospital premises (92%). However, the hospital of Himachal Pradesh was found to have an average level of preparedness in this section (15-92%). The main reason behind this is the age of the hospital. The UP hospital that has scored less on preparedness was commissioned in the year 1969 and hence its infrastructure-related preparedness was not as per the latest standards which are used for measurement. The second hospital of UP was commissioned in 2016 and had its infrastructural elements built-in consonance with the latest guidelines related to safety standards.
The hospitals were evaluated with respect to an operational plan for internal or external disasters, and one hospital of Haryana was found to have a 93% score of preparedness in the category related to the operational plan for internal or external disasters. The hospitals of Delhi at 89% and Uttarakhand at 82% also reported high preparedness. Both the hospitals of UP, one hospital of Delhi and one hospital of Himachal Pradesh reported an average level of preparedness at 47%, 57% and 71% each. This category had 31 elements and included information related to hospital disaster plans for different types of disaster situations, type of disaster codes, conducting mock drill and variations observed in mock drills, special administrative procedures followed in the event of disaster especially related to expansion of space and beds in emergency and critical care units, the safety of personnel and medical records, conducting the facility inspection rounds and issues pending with the facility team, etc.
The hospitals need to have a contingency plan for medical treatment for managing disaster situations. There were eight elements in this category of internal and external disaster plans for landslides, fire, explosion, social conflict, terrorism, chemical accidents, ionising radiations etc., and issues related to Hospital-Acquired Infection (HAI) control, psycho social treatment of patients afflicted to these disaster situations. One hospital of Delhi was found at 100%, followed by a hospital of Uttarakhand at 83%. The hospitals in all other states like Haryana were at 67% and Himachal Pradesh was at 50%. The preparedness was reported at an average and low level in this category in the hospitals of UP at 50% and 17%.
The critical services in a hospital include services like electric power supply and back-up generators, communication system, drinking water supply, fuel reserve, medical gases, waste management system including solid waste and maintenance of these systems. These elements measure the level of availability, accessibility, and relevance of documents that are essential when responding to an emergency in the organisation. And all the hospitals were found to have 100% preparedness in these elements, except one hospital of UP and that of HP which were found to have 50% and 75% of preparedness.
Availability of medicines, treatment items, instruments, medical gases, electro-medical equipment, life support, Personal Protective Equipment (PPE) and crash cart supplies up to 72 hours for use in an emergency was also evaluated. A high level of preparedness was found in one hospital of Uttarakhand and Delhi (100%), followed by the other two hospitals of Delhi at 90% and 80%, respectively. The Delhi hospital with a 100% preparedness level possessed accreditation from Joint Commission International also. Both the hospitals of UP and one hospital of HP and Delhi were found to have 70% of preparedness in the items.
Columns, beams, walls, floor slabs, etc., are structural elements that form part of the load-bearing system of the building. In this section details about prior structural damage to the building followed by details about remodelling and restructuring of the building were collected. The hospital of HP had reported prior structural damages in terms of crevices in the wall and basement due to earthquakes. The preparedness was found to be 100% in all other hospitals in this section. The condition of a building, including structural detailing about connections, foundation and any irregularities in the height of the building comprises of the structural system. One hospital of UP was found to be 50% prepared owing to its old structure and lack of information about the depth of the its foundation. All the other hospitals were found to have a 100% preparedness level owing to their construction from the year 2000 onwards except for one hospital in Delhi which was commissioned in the year 1991.
The non structural elements do not form part of the load-bearing system of the building. They include architectural components, equipment, and systems that are necessary for the operation of the building. This includes critical systems like the electrical system, telecommunication, water supply, fuel storage, medical gases, Heating, Ventilation, and Air Conditioning (HVAC), and office furnishings. In this category all the hospitals except one hospital of UP were found to have a high level of preparedness ranging from 87% to 98%. The hospital of UP was found to have average preparedness at 35% in these components.
The architectural elements encompass the condition and safety of doors, entrances, windows, shutters, building envelope, roofing, false or suspended ceiling, parapets, stairways, floor coverings, internal walls, partitions, internal and external lighting systems etc. All the hospitals were found to have a 100% preparedness level except the one, the old hospital of UP. The construction of this hospital was in the year 1960s and it was commissioned in 1969.
Discussion
As per the United Nations Development Programme (UNDP) (2004) report, between the year 1980 and 2000, approximately 75% of the world’s population lived in the areas affected at least once by disaster events like earthquakes, tropical cyclones, floods or droughts. During the last two decades of the 20th century (1982-2001), natural disasters in India had claimed a total death toll of around 1,07,813 lives (on an average more than 5,390 deaths every year) and economic losses accounted for 2% of the GDP due to disasters as per the study of the World Bank [12]. The inception of the quality management standards and disaster management act is recent and dates back to 2005. These concepts are new to Indian healthcare systems and need a forecasting and visionary approach. The Comptroller and Auditor General of India (CAG) conducted a performance audit of the disaster preparedness intending to assess the level of preparation in the country to manage disasters. It was conducted from May 2012 to September 2012 and tabled in the Parliament on 23rd April 2013. The Audit had found that despite considerable progress in setting up institutions and creating funding arrangements, there were critical gaps in the preparedness level for various disasters. It was concluded that the system, which came into effect post the disaster management act 2005, is yet to achieve its desired impact. Implementation of accreditation standards is demanding for organisations, however in the developing nations, accreditation is frequently used by a hospital to guarantee quality and patient safety. The empirical literature on the benefits of accreditation is sparse but Devkaran S and O’Farrell PN conducted an empirical, interrupted time series analysis to examine the impact of healthcare accreditation on hospital quality measures in a 150-bed multispecialty hospital in Abu Dhabi, the United Arab Emirates in 2015 [13]. The study concluded that there was a transient drop in performance immediately after the survey. It also showed that the improvement achieved from accreditation was maintained during the three-year accreditation cycle. A comparative study of NABH accredited and non NABH accredited hospitals in Jaipur, was conducted in 2015. In this study, three NABH accredited private hospitals and three non NABH accredited private hospitals were compared and over 1260 responses were collected. The study concluded that “NABH accreditation” had emerged as an effective tool to improve the efficiency and effectiveness of hospital services and facilities [9]. It has uniformly improved quality in all areas of hospital services and promoted a hospital culture that meets patient’s needs of quality. Its effective implementation has helped to improve hospital performance and increased patient satisfaction. It has given a competitive advantage in the healthcare industry and strengthened the community confidence in service quality and patient safety.
The preparedness of hospitals is not limited to manpower but also includes structural and non structural elements related to infrastructure and processes. This study revealed strong relation between the implementation of accreditation standards and disaster preparedness of hospitals. It helps keep hospitals functional during a disaster situation leading to uninterrupted services to disaster victims. This study highlights the importance of disaster preparedness according to the disaster profile of the region and signifies specific needs as per the same. The variation in the preparedness of hospitals from one state to another also indicates subjectivity in the interpretation of accreditation standards and implementation. Secondly, the preparation specific to the hazards faced by the hospitals was also not found to be upto the mark, which implies that training and sensitisation of key stakeholders in disaster specific preparedness were lacking in the accredited hospitals. The study may be further used as a baseline for comparison of hospital disaster preparedness with other geographical regions of India and a comparative study may be conducted with non accredited hospitals to find out the effect of accreditation on disaster preparedness.
Limitation(s)
The limitations of this research include the restriction of the study to private NABH hospitals and could not include the government medical colleges that have achieved pre-entry level of NABH accreditation, due to the lengthy process of obtaining permission from state governments. Secondly, the staff was hesitant in giving their employee identification, educational qualification details and name of their department, due to fear of revealing identity and linking of their performance in the study with their appraisals. Thirdly, there was no participation from the hospitals of Punjab due to which a major portion of hazard and preparedness was missed out in the study.
Conclusion(s)
The research concludes that NABH standards guide the hospital regarding the provision of a safe and secure environment for patients, their families, staff, and visitors. The standards ask the organisation to take steps to ensure this, including proactive risk mitigation measures like conducting regular facility inspection rounds, and mock drills for fire and non fire emergencies. The study reveals that hospitals have earmarked their expansion capacity for disaster management. They have reserved approximately 10% of their operational beds for use during disaster and these beds were allocated to both medicine and surgical specialities. Similarly, the hospitals had one OT also for use during the disaster event. Despite of the age of the hospitals and diverse hazard profiles, the minimum level of preparedness was observed in all the accredited hospitals. Their willingness to participate in such a study also indicates their evolutionary nature and adaptability to new systems for patient and staff safety. Even though measurement of disaster preparedness of hospitals is not undertaken by the NABH assessment and the team only provides suggestions as per the evidenced-based, best practices to improve safety in total and make the hospitals disaster resilience we can say that accreditation standards become the best way to prepare hospitals for disaster management.
n=number of hazard elements