Recurrent Multinodular Pleomorphic Adenoma of Parotid Gland- A Case Report
Priya Kanagamuthu1, Swetha Thirumurthi2, S Rajasekaran3, S Prabakaran4, RB Namasivaya Navin5
1 Professor, Department of ENT, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
2 Junior Resident, Department of ENT, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
3 Professor and Head, Department of ENT, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
4 Assistant Professor, Department of ENT, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
5 Assistant Professor, Department of ENT, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Priya Kanagamuthu, No. A6, Staff Villa Ground Floor, Chettinad Health City, Kelambakkam, Chennai, Tamil Nadu, India.
E-mail: catchpriya.29@gmail.com
Pleomorphic adenoma or benign salivary gland tumours predominantly affects the superficial lobe of parotid gland. It is a slow growing swelling with or without facial nerve involvement with female predilection in third and fifth decade of life. The origin of the tumour is both epithelial and connective tissue and hence it is of pleomorphic nature. After surgery, its recurrence rate varies considerably and seems to depend more on the surgical technique used. A 49-year-old male patient presented with complaints of swelling in front of right ear and right parotid region for past eight years. He gave previous history of similar swelling in the right parotid region and history of previous surgery done elsewhere in 2009. Right superficial parotidectomy was done following which he was asymptomatic for two years. On examination of right parotid- a multilobulated irregular swelling was present in right parotid region and the swelling extended till the right ear lobule. The swelling hid previous surgical scar. Facial nerve was clinically intact. Fine Needle Aspiration Cytology (FNAC) was suggestive of Pleomorphic Adenoma. Magnetic Resonance Imaging (MRI) with contrast revealed that the lesions were arising from superficial lobe of the parotid gland. Right superficial parotidectomy was planned. Mass was excised and sent for histopathological examination and was reported to be Pleomorphic Adenoma. Patient is still on follow-up and no recurrence has been noted. The rate of recurrence depends on tumour spillage, intra-surgical rupture, or any histopathological feature. There is significant risk for local recurrence if the microscopic finger like formation (pseudopodia) of tumour tissue extends beyond the main mass.
Benign tumour, Nodular swelling, Parotidectomy, Salivary gland tumours
Case Report
A 49-year-old male patient presented to the Ear Nose Throat (ENT) Outpatient Department (OPD) with complaints of swelling in front of the right ear and right parotid region for the past eight years, which was initially small, gradually progressed and attained the present size. History of similar swelling in the right parotid region in the past was given. Patient gave previous history of surgery done elsewhere in the right parotid region in 2009 following which he was asymptomatic for two years. Patient did not give any history of associated pain, trauma, or relevant ENT symptoms. He wasn’t a known case of diabetes mellitus, hypertension, bronchial asthma, and tuberculosis. There was no relevant personal and family history present.
On general examination, vitals were found to be normal. Local examination of the ear, nose, and throat was found to be normal with facial asymmetry on the right side. Local examination of the right parotid region revealed a multilobulated irregular swelling of size approximately 6×5 cm of variable consistency indurating the right ear lobule and also extending below the lobule of size 4×3 cm [Table/Fig-1]. The skin over the swelling appeared stretched and the colour of the skin was normal. The swelling hid the previous surgical scar. No warmth or tenderness was present with respect to the swelling. Clinically, no facial nerve involvement was seen.
Preoperative picture of the Right parotid region.

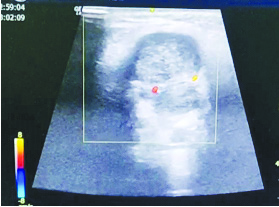
With the above history and clinical examination, the patient was investigated further with ultrasound parotid region, FNAC, MRI parotid region. Ultrasound parotid region showed a large heteroechoic lesion in right preauricular area arising from the right parotid gland [Table/Fig-2]. Malignant aetiology was more likely than benign and hence FNAC was suggested. Features suggestive of pleomorphic adenoma were seen in FNAC.
Ultrasound image of Right parotid.
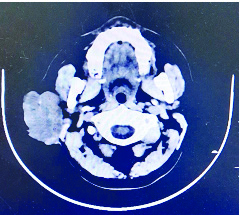
MRI of the parotid region with contrast revealed an exophytic lesion involving right masticator/parotid spaces, arising from the superficial lobe of the parotid gland/connective tissue [Table/Fig-3].
MRI with contrast image of Right parotid region.
With the above investigation, clinical history, and clinical examination, a diagnosis of pleomorphic adenoma of the parotid gland was made and surgery was planned. Further investigations such as necessary blood and radiological investigations were done and fitness was obtained for general anaesthesia.
Operative Procedure
Surgery was done under general anaesthesia with orotracheal intubation. The patient was in supine position with head turned to the left, parts painted and draped. Local infiltration was given. Incision was placed over the swelling extending 1 cm away from the right preauricular region and 1 cm down below the right ear lobule.
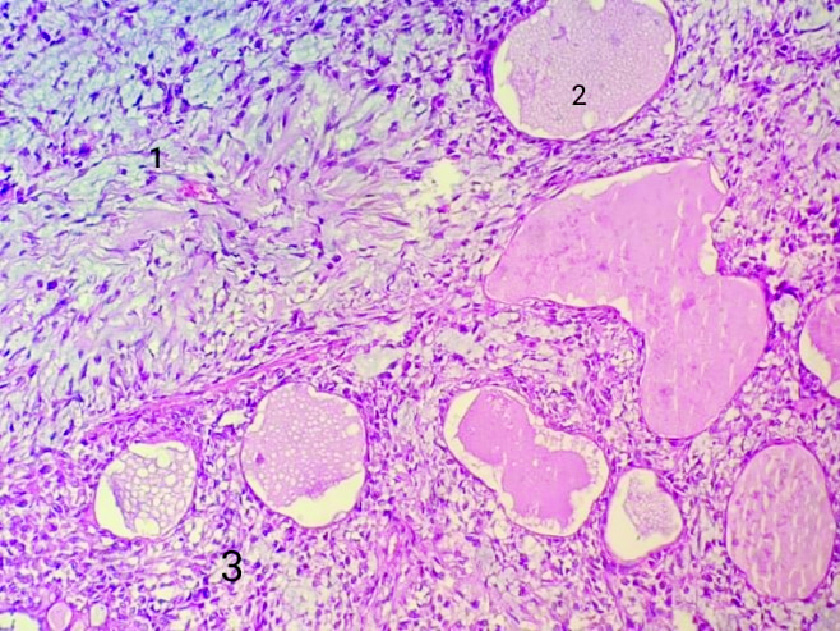
Skin, subcutaneous tissue, Superficial Musculo Aponeurotic System (SMAS) layer was identified and dissected. Skin flap was elevated. Mastoid tip, tympanosquamous suture line, tragal pointer were identified. Meticulous dissection was done [Table/Fig-4]. The Facial nerve was identified and preserved. A bit of the specimen was removed and sent for histopathological examination- Frozen section, which was suggestive of pleomorphic adenoma. The mass was dissected and removed in total [Table/Fig-5]. Specimen was sent for histopathological examination. A drain was placed in the surgical site. Incision was sutured with 3-0 ethilon and haemostasis was obtained. Sterile dressing was applied and the patient was given adequate antibiotics. On histopathological examination, it was observed that the tumour arranged in a glandular and trabecular pattern with chondromyxoid stroma [Table/Fig-6]. Cystic spaces were present. Hypercellular area was also seen. Focally the cells showed atypical features with enlarged nuclei. But no atypical mitosis or necrosis was seen. Suture removal was done on the tenth postoperative day and the patient was discharged. The wound appeared to be healthy [Table/Fig-7].
Intraoperative image of the lesion.

Specimen of Right parotid gland.

Hematoxyline and eosin stained histopathological picture of Pleomorphic adenoma arranged in a glandular (2) and trabecular (3) pattern with chondromyxoid stroma (1) under X200 magnification.
Postoperative picture of the Right Parotid region.

Follow-up: Patient is still on follow-up once in a period of six months and no recurrence has been noted.
Discussion
Pleomorphic adenoma more commonly affects the superficial lobe of the parotid gland. They can also arise from accessory parotid tissue along the line of the duct, minor salivary gland (10%), and submandibular gland (5%). It is a slow growing swelling with or without facial nerve involvement with female predilection in the third and fifth decade of life. The Pleomorphic nature of the tumour can be explained based on its epithelial and connective tissue origin [1].
Pleomorphic adenoma is the most common tumour of salivary gland. Due to its dual origin from connective tissue and epithelial elements, it is known as benign mixed tumour. It is the most common of all salivary gland tumours constituting up to 2/3rd of all such tumours. Although, the incidence has been increasing in the last two decades, its aetiology remains unknown [2]. It is slightly more common in females than in males with 1.2:1 ratio [3]. Seifert criteria for classification of pleomorphic adenoma into four types based on histological subtype are: 30% to 50% of myxoid stroma, 80% of myxoid stroma, 30% of myxoid stroma and 30% of myxoid stroma with plasmocytoid cells [4].
After surgery, the recurrence rate for pleomorphic adenoma varies considerably and seems to depend more on the surgical technique used [5]. Intra-surgical rupture, tumour spillage, or any histopathological feature might have an impact on the rate of recurrence [6].
Johns ME and Goldsmith MM, reported that the occurrence of pseudopodia-microscopic finger-like formations of tumour tissue that extends beyond the main lump of the tumour is a significant risk factor for local recurrence [7]. In a review by Phillips PP and Olsen KD, the rate of recurrence varied between 20%-45% after simple enucleation and 2%-5% after lateral lobectomy of the parotid gland, but it was only 0-0.4% when the more radical total parotidectomy technique was used [8].
The rate of recurrence depends on tumour spillage due to intra-surgical rupture of pseudo capsule. [9]. Inadvertent tumour spillage and pseudo capsular tear may cause multinodular recurrence. The prognosis of this tumour is highly variable depending on histological finding and tumour extent [10].
Differential diagnosis include Warthin’s tumour, Mucoepidermoid carcinoma, Myoepithelioma, Adenoid cystic carcinoma, Parotid nodal metastasis, Parotid non-Hodgkin’s lymphoma, and Intra parotid facial nerve schwannoma [8]. Treatment for pleomorphic adenoma is complete surgical resection with negative margin forms the mainstay of the treatment [11]. In this case, the patient was thoroughly followed-up to date and no signs of recurrence were observed during the follow-up.
Conclusion(s)
For most patients with benign well-circumscribed tumours, prognosis is excellent after surgical resection, however, recurrence is common with pleomorphic adenomas especially those occurring in the parotid gland. Confirmatory diagnosis of pleomorphic adenoma is by FNAC and biopsy. Treatment for pleomorphic adenoma is complete surgical excision of the tumour.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 18, 2021
Manual Googling: Apr 14, 2021
iThenticate Software: Apr 24, 2021 (6%)
[1]. Koral K, Sayre J, Bhuta S, Abemayor E, Lufkin R, Recurrent pleomorphic adenoma of the parotid gland in pediatric and adult patients: Value of multiple lesions as a diagnostic indicatorAm J Roentgenol 2003 180(4):1171-74.10.2214/ajr.180.4.180117112646477 [Google Scholar] [CrossRef] [PubMed]
[2]. Kato H, Kawaguchi M, Ando T, Mizuta K, Aoki M, Matsuo M, Pleomorphic adenoma of salivary glands: Common and uncommon CT and MR imaging featuresJapanese Journal of Radiology 2018 36(8):463-71.10.1007/s11604-018-0747-y29845358 [Google Scholar] [CrossRef] [PubMed]
[3]. Wu YC, Wang YP, Cheng SJ, Chen HM, Sun A, Chang JY, Clinicopathological study of 74 palatal pleomorphic adenomasJournal of the Formosan Medical Association 2016 115(1):25-30.10.1016/j.jfma.2015.09.00826776759 [Google Scholar] [CrossRef] [PubMed]
[4]. de Sousa Lopes ML, Barroso KM, Henriques ÁC, Dos Santos JN, Martins MD, de Souza LB, Pleomorphic adenomas of the salivary glands: Retrospective multicentric study of 130 cases with emphasis on histopathological featuresEuropean Archives of Oto-Rhino-Laryngology 2017 274(1):543-51.10.1007/s00405-016-4253-527520570 [Google Scholar] [CrossRef] [PubMed]
[5]. Dulguerov P, Todic J, Pusztaszeri M, Alotaibi NH, Why do parotid pleomorphic adenomas recur? A systematic review of pathological and surgical variablesFrontiers in Surgery 2017 4:2610.3389/fsurg.2017.0002628555187 [Google Scholar] [CrossRef] [PubMed]
[6]. Henriksson G, Westrin KM, Carlsöö B, Silfverswärd C, Recurrent primary pleomorphic adenomas of salivary gland origin: Intrasurgical rupture, histopathologic features, and pseudopodiaCancer: Interdisciplinary International Journal of the American Cancer Society 1998 82(4):617-20.10.1002/(SICI)1097-0142(19980215)82:4<617::AID-CNCR1>3.0.CO;2-I [Google Scholar] [CrossRef]
[7]. Johns ME, Goldsmith MM, Incidence, diagnosis, and classification of salivary gland tumours. Part 1Oncology (Williston Park, NY) 1989 3(2):47-56. [Google Scholar]
[8]. Phillips PP, Olsen KD, Recurrent pleomorphic adenoma of the parotid gland: Report of 126 cases and a review of the literatureAnnals of Otology, Rhinology & Laryngology 1995 104(2):100-04.10.1177/0003489495104002037857010 [Google Scholar] [CrossRef] [PubMed]
[9]. Colella G, Cannavale R, Chiodini P, Meta-analysis of surgical approaches to the treatment of parotid pleomorphic adenomas and recurrence ratesJournal of Cranio-Maxillofacial Surgery 2015 43(6):738-45.10.1016/j.jcms.2015.03.01725982213 [Google Scholar] [CrossRef] [PubMed]
[10]. Mc Loughlin L, Gillanders SL, Smith S, Young O, The role of adjuvant radiotherapy in management of recurrent pleomorphic adenoma of the parotid gland: A systematic reviewEuropean Archives of Oto-Rhino-Laryngology 2019 276(2):283-95.10.1007/s00405-018-5205-z30426229 [Google Scholar] [CrossRef] [PubMed]
[11]. Jain S, Hasan S, Vyas N, Shah N, Dalal S, Pleomorphic adenoma of the parotid gland: Report of a case with review of literatureEthiopian Journal of Health Sciences 2015 25(2):189-94.10.4314/ejhs.v25i2.1326124628 [Google Scholar] [CrossRef] [PubMed]