A Case Series of Lung Sequelae and Aspergillus Antigenemia: A Hidden Entity in Post-COVID-19 Critically ill Patients
Sonali Banwait1, Poonam Gupta2
1 Associate Professor, Department of Anaesthesia and Critical Care, VMMC and Safdarjung Hospital, New Delhi, India.
2 Consultant and Professor, Department of Anaesthesia and Critical Care, VMMC and Safdarjung Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sonali Banwait, A-701, Delhi State Society, Plot No. 1, Sector-19, Dwarka, New Delhi, India.
E-mail: sonalibanwait@gmail.com
Coronavirus Disease-2019 Associated Invasive Aspergillosis (CAPA) is a known entity with significant mortality. There is paucity of literature with secondary aspergillosis infection in post-COVID-19 patients. Serum galactomannan is a highly sensitive test for screening patients for Aspergillus antigenemia. Here, authors reported five post-COVID-19 patients with High Resolution Computed Tomography (HRCT) features and associated high risk factors for opportunistic aspergillosis (55-years-old-male, 46-years-old-male, 75-years-old-female, 55-years-old-female and 27-years-old-male) like prolonged intensive care stay, Acute Respiratory Distress Syndrome (ARDS), corticosteroid and broad spectrum antibiotic therapy like Meropenem, Colistin and Targocid etc.
Acute respiratory distress syndromes, Coronavirus disease-2019, Galactomannan
Introduction
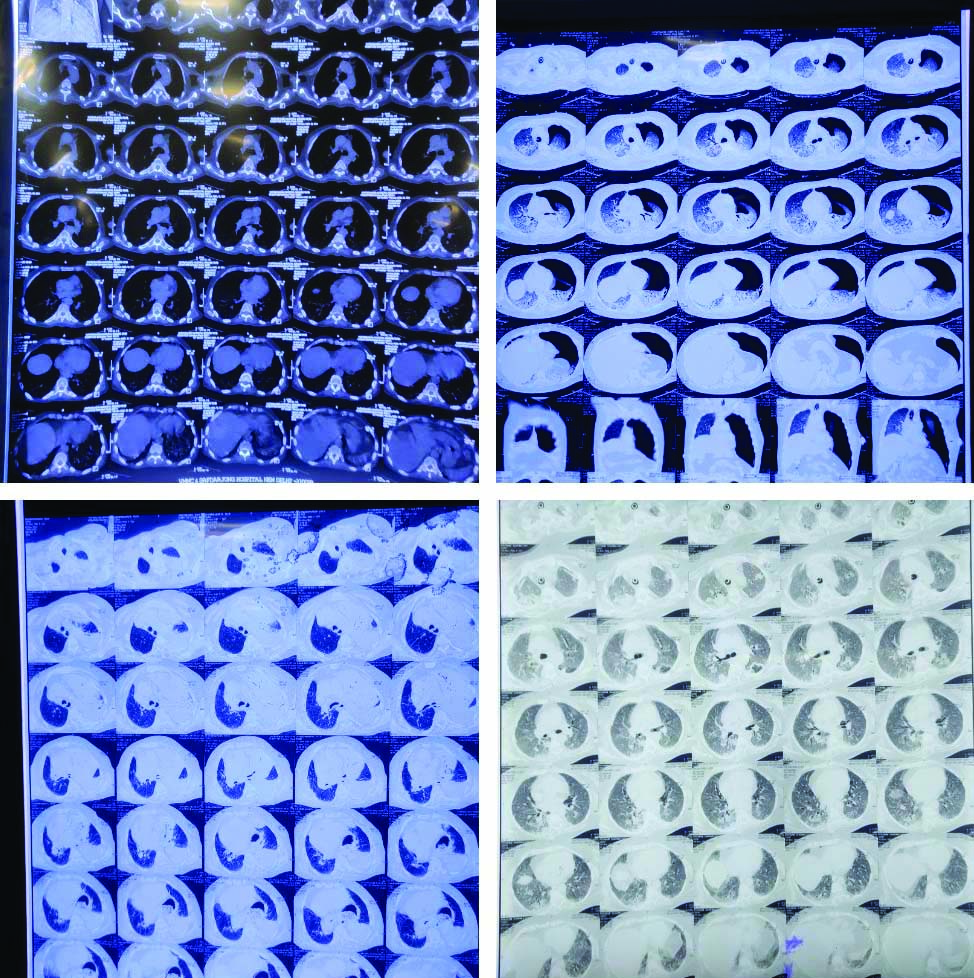
Novel Coronavirus Severe Acute Respiratory Syndrome Coronavirus-2 (SARS CoV-2) is causing mayhem all over the world. Indian data reports 9.75 million infections with 1,43,355 deaths with 5 percent patients critically ill requiring prolonged stay in Intensive Care Unit (ICU) [1,2]. Most of the critically ill post-COVID-19 patients have reported respiratory epithelial damage due to cytokine storm in the active phase of the disease which initially manifests as ARDS [3]. HRCT findings like ground glass opacities, consolidation, crazy paving pattern, air crescent and reverse halo sign, fibrosis and pleural thickening have been reported in patients of CAPA [4-6]. In this case series also, HRCT findings were presented by all the cases [Table/Fig-1]. ARDS, broad-spectrum antibiotics, corticosteroid therapy and ICU stay, all predispose these patients to opportunistic fungal infections especially Aspergillosis [5].
HRCT findings of patient 1,2,3,4.
HRCT: High resolution computed tomography
CAPA is a rapidly emerging entity worldwide with cases reported from China and rest of the world [6-9]. It is associated with significant mortality of around 33 percent [5]. However, there is paucity of data of aspergillosis in post-COVID-19 patients. Authors hereby highlight the clinical features including host factors and radiological imaging along with serum galactomannan testing in five post-COVID-19 patients.
Case Series
Case 1
A 55-year-old male patient, diagnosed case of COVID-19 having no co-morbidities with COVID ICU stay of 33 days was transferred to non-COVID ICU for further management. On admission, his Horowitz index was less than 250 on Non-Rebreathing Mask (NRBM) at the rate 15/L min with Acute Physiology and Chronic Health Evaluation (APACHE) Score of 11. Treatment included Remdesivir 200 mg loading followed by 100 mg OD for four days, methylprednisolone 40 mg BD and clexane 0.4 mL subcutaneous BD for COVID-19. HRCT chest showed bilateral asymmetrical patchy as well as confluent ground glass opacities with inter-lobular septal thickening with mild bronchiectasis and mild pneumomediastinum. His serum galactomannan was positive with Optical Density Index (ODI) as 5.12. His oxygen requirement gradually increased resulting in type I respiratory failure requiring mechanical ventilation.
Case 2
A 46-year-old male patient, diagnosed case of epiglottitis and diabetes mellitus with COVID-19 positive 10 days back. He was transferred to non-COVID ICU on NRBM at the rate 15/min. His Horowitz score was less than 200 and APACHE score was 8. Ultrasound chest revealed significant bilateral pleural fluid. Intercostal Drain (ICD) insertion lead to empyema drainage. Patient dramatically improved with tapering oxygen requirement. HRCT showed bilateral ground glass opacities with interlobular thickening. Serum galactomannan was positive with ODI calculated as 0.85701.
Case 3
This was a case of 75-year-old female patient, recovered from COVID-19, 15 days back. She was admitted with fever, bowel and bladder incontinence. Her Horowitz index was less than 100 with APACHE 17 and she required oxygen therapy with NRBM at the rate 10 L/min. HRCT revealed consolidation in left upper lung lobe, lingual and right lower lung lobe with mediastinal lymphadenopathy along with herniation of stomach in lower thorax through oesophageal hiatus. Serum galactomannan test was positive with ODI as 1.52.
Case 4
A 55-year-old female patient stayed in COVID ICU for 12 days and then was shifted to non-COVID ICU in view of high ventilatory support. HRCT revealed bilateral ground glass opacities with crazy pave appearance. Her Horowitz index was less than 100 and APACHE score was 8. Serum galactomannan test done was positive with ODI as 3.78.
Case 5
A 27-year-old young male patient previously diagnosed with COVID-19 having 30 day COVID-ICU stay was transferred to non-COVID-ICU intubated on mechanical ventilation in view of recent left pneumothorax with intercoastal drainage in-situ. His Horowitz score less than 100 with APACHE 9. His previous sputum culture revealed klebsiella pneumonia and tracheal culture had Candida parapilosis. HRCT chest revealed left gross pneumothorax with consolidation in right upper and bilateral lower lobes. Bilateral lung fields showed ground glass opacities with diffuse interlobular thickening. Serum galactomannan was positive with ODI calculated as 0.65. Demographic, clinical details and Lab investigation of all cases are mentioned in [Table/Fig-2].
Demographic details, clinical details, medications and prognostic details of the patients.
| Patient | Age/Gender | APACHE | Co-morbidities | Post-COVID-19 ICU stay (days) | Steroid | HRCT | Galactomannan | Antibiotics | Outcome |
|---|
| 1 | 55/M | 11 | Recent onset depression | 12 | Methylprednisolone 40 mg BD | Bilateral asymmetrical patchy as well as confluent ground glass opacities with interlobular septal thickening with mild bronchiectasis and mild pneumomediastinum | Positive | Meropenem, colistin | Dead |
| 2 | 46/M | 8 | Diabetes mellitus | 7 | Dexamethasone 8 mg OD | Bilateral ground glass opacities with interlobular thickening | Positive | Meropenem | Alive |
| 3 | 75/F | 17 | None | 10 | Dexamethasone 4 mg OD | Consolidation in left upper lung lobe, lingual and right lower lung lobe with mediastinal lymphadenopathy along with herniation of stomach in lower thorax through oesophageal hiatus | Positive | Meropenem | Dead |
| 4 | 55/F | 8 | Diabetes | 20 | Methylprednisolone 40 mg BD | Bilateral ground glass opacities with crazy pave appearance | Positive | Targocid Meropenem | Dead |
| 5 | 27/M | 9 | None | 7 | Methylprednisolone 60 mg BD | Bilateral lung fields had ground glass opacities with diffuse interlobular thickening with left gross pneumothorax with consolidation in right upper and bilateral lower lobes. | Positive | Meropenem, Colistin | Dead |
APACHE: Acute physiology and chronic health evaluation; COVID-19: Coronavirus-2019; ICU: Intensive care unit; HRCT: High resolution computed tomography; M: Male; F: Female
Discussion
COVID-19 burden of disease has overwhelmed the healthcare system worldwide with a mortality rate of 1.4% in India with increasing number of patients requiring intensive care [1]. CAPA has emerged as a new entity, reported from most countries but it has limited Indian data due to scarce testing. COVID-19 patients are difficult to cover in the ambit of Revised European Organisation for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) criteria as most of them neither have neutropenia nor fulfill the radiological and host factors for invasive aspergillosis [10]. AspIcu algorithm which includes various clinical, biochemical and serological factors is more appropriate in diagnosing invasive aspergillosis in COVID-19 patients [11]. In the patients of this case series, clinical factors like fever, dyspnoea, worsening respiratory function along with radiological factors of abnormal lung imaging with HRCT findings and positive serum galactomannan was present. In addition, there was prolonged use of corticosteroids.
Ground glass opacities in lung are hallmark of HRCT of COVID-19 patients and manifests as ARDS [3]. This damage to respiratory epithelium predisposes to opportunistic fungal infections especially aspergillosis. All the patients had these findings in HRCT [Table/Fig-2] with loss of lung parenchyma and continuing fibrosis, thus requiring prolonged oxygen therapy or mechanical ventilation. In present cases, patients received corticosteroids therapy, the cornerstone of COVID-19 therapy predisposing to immunosuppression. The chances of opportunistic fungal infection are increased by respiratory endothelial damage and use of broad-spectrum antibiotics and corticosteroids. The diagnostic modalities for Aspergillosis include galactomannan testing and growth of aspergillus in culture media from serum, tracheal aspirate and bronchoalveolar lavage samples [12].
Galactomannan, a polysaccharide present in aspergillus cell wall is released during active infection and can be detected in serum for one to eight weeks. In contrast to fungal culture, serum galactomannan has high sensitivity in diagnosing aspergillosis and is measured as ODI. An ODI of >0.5 is the diagnostic threshold for aspergillus infection [13]. After institution of anti-fungal therapy there is a progressive decrease of ODI [12].
None of the present patients were administered with Piperacillin Tazobactam since it could have resulted in false positive result. Bronchoalveolar lavage specimens were not collected due to risk of aerosolisation. All of the patients discussed here had clinical features and associated high risk factors with HRCT findings and serum galctomannan positivity with a high probabiltiy suggestive of aspergillosis. Although, as fungal cultures or autopsy biopsy were not performed to isolate aspergillus due to logistic reasons proven, diagnosis of Aspergillosis cannot be confirmed.
Conclusion(s)
This case series provides ground to screen critically ill post-COVID-19 patients for aspergillosis. Though could not be done due to logistic reasons, serum galactomannan and bronchoscopy should idealy be done to assess the burden of disease. This would lead to early initiation of antifungal treatment and mitigate mortality associated with it.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 16, 2021
Manual Googling: Mar 17, 2021
iThenticate Software: Mar 20, 2021 (5%)
[1]. COVID-19 update COVID-19 INDIA. Ministry of Health and Family Welfare. MOHFW; (2020) [Google Scholar]
[2]. Wu Z, McGoogan JM, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and PreventionJAMA 2020 323(13):123910.1001/jama.2020.264832091533 [Google Scholar] [CrossRef] [PubMed]
[3]. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Pathological findings of COVID-19 associated with acute respiratory distress syndromeLancet Respir Med 2020 8(4):420-22.10.1016/S2213-2600(20)30076-X [Google Scholar] [CrossRef]
[4]. Liu D, Zhang W, Pan F, Li L, Yang L, Zheng D, The pulmonary sequalae in discharged patients with COVID-19: A short-term observational studyRespir Res 2020 21:12510.1186/s12931-020-01385-132448391 [Google Scholar] [CrossRef] [PubMed]
[5]. White PL, Dhillon R, Cordey A, Hughes H, Faggian F, Soni S, A national strategy to diagnose COVID-19 associated invasive fungal disease in the ICUClin Infect Dis 2020 :ciaa129810.1093/cid/ciaa129832860682 [Google Scholar] [CrossRef] [PubMed]
[6]. Wang J, Yang Q, Zhang P, Sheng J, Zhou J, Qu T, Clinical characteristics of invasive pulmonary aspergillosis in patients with COVID-19 in Zhejiang, China: a retrospective case seriesCrit Care 2020 24:29910.1186/s13054-020-03046-732503617 [Google Scholar] [CrossRef] [PubMed]
[7]. Blaize M, Mayaux J, Nabet C, Lampros A, Marcelin AG, Thellier M, Fatal invasive aspergillosis and coronavirus disease in an immunocompetent patientEmerg Infect Dis 2020 26(7):1636-37.10.3201/eid2607.20160332343223 [Google Scholar] [CrossRef] [PubMed]
[8]. Antinori S, Rech R, Galimberti L, Castelli A, Angeli E, Fossali T, Invasive pulmonary aspergillosis complicating SARS-CoV-2 pneumonia: A diagnostic challengeTravel Med Infect Dis 2020 2020:10175210.1016/j.tmaid.2020.10175232470620 [Google Scholar] [CrossRef] [PubMed]
[9]. Sharma A, Hofmeyr A, Bansal A, Thakkar D, Lam L, Harrington Z, COVID-19 associated pulmonary aspergillosis (CAPA): An Australian case reportMed Mycol. Case Rep 2020 31:06-10.10.1016/j.mmcr.2020.06.00232837878 [Google Scholar] [CrossRef] [PubMed]
[10]. Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE, Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortiumClin Infect Dis 2019 71(6):1367-76.10.1093/cid/ciz100831802125 [Google Scholar] [CrossRef] [PubMed]
[11]. Blot SI, Taccone FS, Van den Abeele AM, Bulpa P, Meersseman W, Brusselaers N, A clinical algorithm to diagnose invasive pulmonary aspergillosis in critically ill patientsAm J Respir Crit Care Med 2012 186(1):56-64.10.1164/rccm.201111-1978OC22517788 [Google Scholar] [CrossRef] [PubMed]
[12]. Ullmann AJ, Aguado JM, Arikan-Akdagli S, Denning DW, Groll AH, Lagrou K, Diagnosis and management of Aspergillus diseases: Executive summary of the 2017 ESCMID-ECMM-ERS guidelineClin Microbiol Infect 2018 24(Suppl 1):e1-e38.10.1016/j.cmi.2018.01.00229544767 [Google Scholar] [CrossRef] [PubMed]
[13]. Zhou W, Li H, Zhang Y, Huang M, He Q, Li P, Diagnostic value of galactomannan antigen test in serum and bronchoalveolar lavage fluid samples from patients with nonneutropenic invasive pulmonary aspergillosisJ Clin Microbiol 2017 55(7):2153-61.10.1128/JCM.00345-1728446576 [Google Scholar] [CrossRef] [PubMed]