A Comparison between Early and Delayed Arthroscopic Anterior Cruciate Ligament Reconstruction: A Prospective Cohort Study
Amarjeet Singh1, Manish Singh2, Simran Preet Singh3, Bhavna Sahni4
1 Senior Resident, Department of Orthopaedics, Government Medical College, Jammu and Kashmir, India.
2 Lecturer, Department of Orthopaedics, Government Medical College, Jammu and Kashmir, India.
3 Postgraduate Student, Department of Orthopaedics, Government Medical College, Jammu and Kashmir, India.
4 Associate Professor, Department of SPM, Preventive Social Medicine, Jammu and Kashmir, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Simran Preet Singh, H. No. 146, Sector 1, Channi Himmat, Jammu and Kashmir, India.
E-mail: simransingh2681@gmail.com
Introduction
A complete Anterior Cruciate Ligament (ACL) injury can result in a progressively increasing symptomatic knee instability, which can cause recurrent intra articular damage and eventually results in osteoarthritis if not treated on time.
Aim
To analyse the effects of delaying ACL reconstruction beyond a period of 12 weeks and compare the results with cases managed before that time period.
Materials and Methods
A prospective cohort study was conducted between July 2017 to October 2019 in Government Medical College, Jammu, India on two groups of patients divided into early (<12 weeks) and delayed (>12 weeks) on the basis of interval between the injury and definitive surgery. The ACL reconstruction was done using a quadrupled semitendinosus-gracilis graft. A standard rehabilitation protocol was followed and the results were compared. Patients were followed-up till one year postsurgery. Software used for statistical analysis was EpiInfo Version 3.0 and Statistical Package for the Social Sciences (SPSS).
Results
A total of 72 patients were included in the study. Forty patients were in the early group and 32 in delayed. Male patients outnumbered the females in both the groups and the incidence of injury was more on the right side. Sports injuries were the most common mode of injury, followed by falls and road traffic accidents in both the groups. The incidence of grade 3/4 medial and Lateral Meniscal (LM) tears was more in the delayed group and the association was statistically significant (p<0.05). There was significant thigh wasting in the delayed group (p<0.05). Two patients were lost to follow-up and were not included in the study.
Conclusion
Delay in ACL reconstruction surgery predisposes to higher grade meniscal lesions and significant thigh wasting and hence the surgery should be preferably done within the first 12 weeks after injury.
Arthroscopy, Lateral meniscal, Quadrupled semitendinosus-gracilis graft
Introduction
The ACL is one of the two cruciate ligaments which aid stabilisation of knee joint. It is made up of strong band of connective tissue and collagen fibres [1]. The ACL is the most commonly injured ligament in the knee. Most ACL tears occur in athletes by non contact mechanism such as rotational forces [2].
A complete ACL injury can result in a progressively increasing symptomatic knee instability, which inflicts recurrent intra-articular damage and eventually results in osteoarthritis if not treated on time [3,4]. Dunn KL et al., suggested that ACL reconstruction reduces the need for additional operations, especially in younger patients [5].
Even though reconstruction is the most common treatment for ACL rupture, but the optimal timing of surgery is still debatable [6]. Often the ACL injuries have been associated with primary meniscal and cartilage lesions. Therefore, the risk of developing secondary meniscal and cartilage lesions in ACL-deficient knees is greatly increased. Hence, the timing is of paramount importance [7].
The ACL reconstruction leads to improvement in instability, but the associated intra-articular injuries still have been a major cause of concern and important prognostic factor for long term results, as it may lead to osteoarthritis. Delay in ACL reconstruction has been eventually linked to increase in intra-articular injuries but the lack of consensus regarding optimal timing of reconstruction is still evident [8]. Early reconstruction may prevent increased instability of the knee and decrease the risk of meniscal and chondral injury. Higher prevalence of intra-articular injury with delayed reconstruction was seen in patients >22 years, whereas no such differences were seen in younger patients [9]. A prospective study by Tambe AD et al., showed that athletes who underwent surgery after 6 weeks of injury had better clinical outcome [10].
Hence, this study aims to highlight the repercussions of delayed arthroscopic ACL reconstruction and assess the functional outcome of delayed ACL reconstruction as compared to when done early based on Lysholm Tegner Scoring, thigh wasting and degree of associated injuries.
Materials and Methods
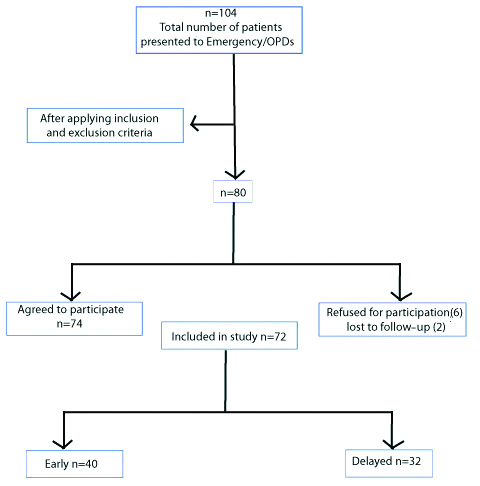
A prospective cohort study was done in Government Medical College, Jammu, India between July 2017 to October 2019 after seeking approval from Institutional Ethical Committee (IEC) clearance viz., no IEC/2017/475. The patients were followed-up for a period of one year postsurgery [Table/Fig-1].
Recruitment of study participants.
A detailed history and clinical examination was done. Diagnosis was confirmed with standard clinical tests and with the help of Magnetic Resonance Imaging (MRI). Patients were categorised into early <12 weeks and delayed >12 weeks groups depending on the time since injury.
Inclusion Criteria
Patients in age group 18-60 with isolated complete ACL tear.
Patients belonging to the age group of 18-60 years with ACL injury with associated:
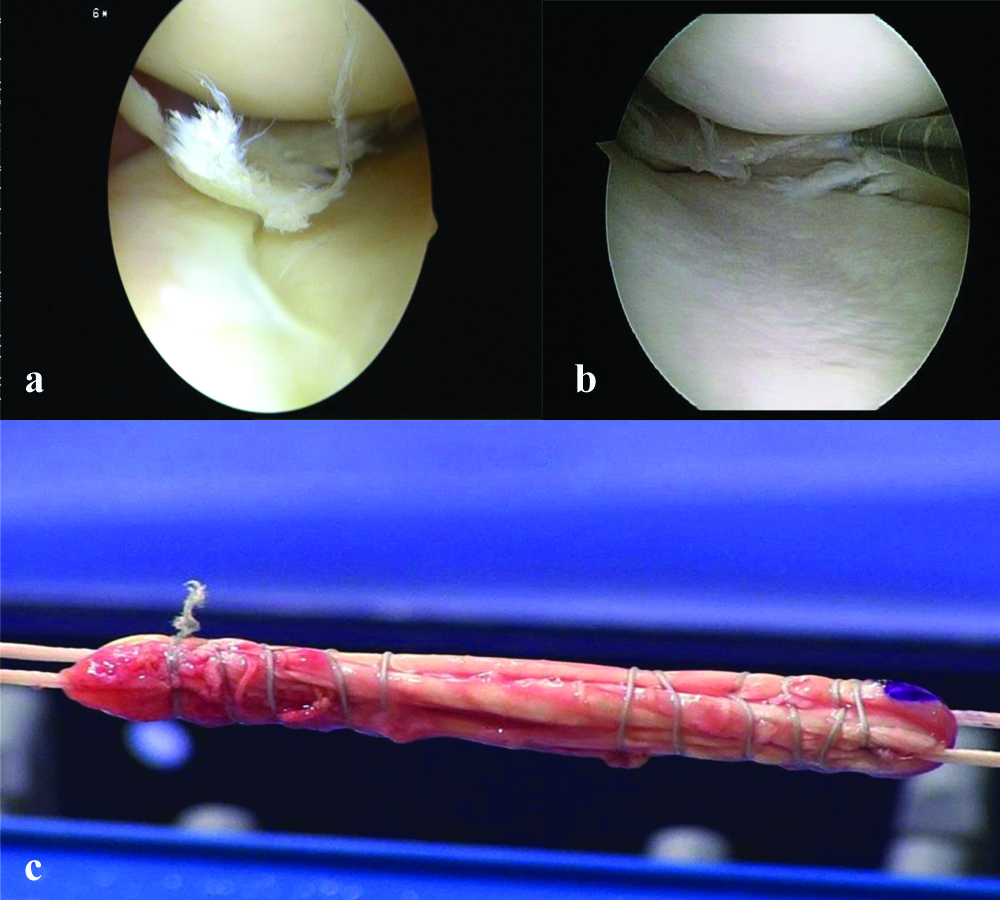
Meniscal injury [Table/Fig-2a]
Chondral Injuries
Medial/lateral collateral ligament sprains.
a) Medial Meniscal (MM) tear seen on diagnostic arthroscopy; b) Meniscal balancing being done using an arthroscopic shaver; c) Intraoperative semitendinosus-gracilis graft preparation.
Exclusion Criteria
Patients with associated Posterior Cruciate Ligament (PCL) injury.
Patients with ACL reinjury.
Patients with associated periarticular fracture.
Patients with associated ipsilateral lower limb fractures.
Patients with associated complete tears of medial or lateral collateral ligaments.
Pre-operative assessment was done using Lachman test, anterior drawer test, pivot shift, X-ray knee, MRI knee, and Lysholm-Tegner score. Functional assessment of patients was done post operatively with Lysholm-Tegner score. The scores of both groups were expressed as mean±SD. The groups were also compared on the basis of incidence of associated injuries and the degree of thigh wasting.
Statistical Analysis
The normality of the data was examined using appropriate tests (Shapiro Wilk test) and the scores were compared between pre and postoperative time points using tests (unpaired t-test and Fisher-exact test). All statistical analysis were considered significant at p<0.05 level of significance. Software used for statistical analysis was EpiInfo Version 3.0 and SPSS.
Surgical Technique
All cases were performed under regional anaesthesia (spinal) with the patient in supine position. Intravenous antibiotic prophylaxis was given. Diagnostic arthroscopy was performed to assess injuries. Meniscal injuries were addressed accordingly [Table/Fig-2b]. Hamstring tendons (semitendinosus and gracilis) were harvested and prepared via a small incision on the anteromedial aspect of tibia over the insertion of pes anserinus using a tendon stripper [Table/Fig-2c]. Tourniquet was used in all the cases.
Postoperative Rehabilitation
Standard Rehabilitation protocol was followed postsurgery. Gentle knee physiotherapy was started after 1st week of surgery and during subsequent weeks range of motion was increased to around 90 degrees at the end of 1st month [Table/Fig-3]. Open chain exercises were begun at six weeks followed by wall slides and lunges.
a) Postoperative knee flexion seen at 4 weeks; b) Visible thigh wasting is seen on right-side.

Results
Total number of patients at the beginning of our study was 74, two patients were lost to follow-up and 72 patients completed the study. A total of 40 (55.56%) were in the early group and 32 (44.44%) were in the delayed group. Patients ranged from 22-48 years in the early group (33.5±3.5 years) and from 20-45 years in the delayed group (32±3.3 years). Majority of the patients (62%) in the study were males (90% in the early and 81.25% in delayed).
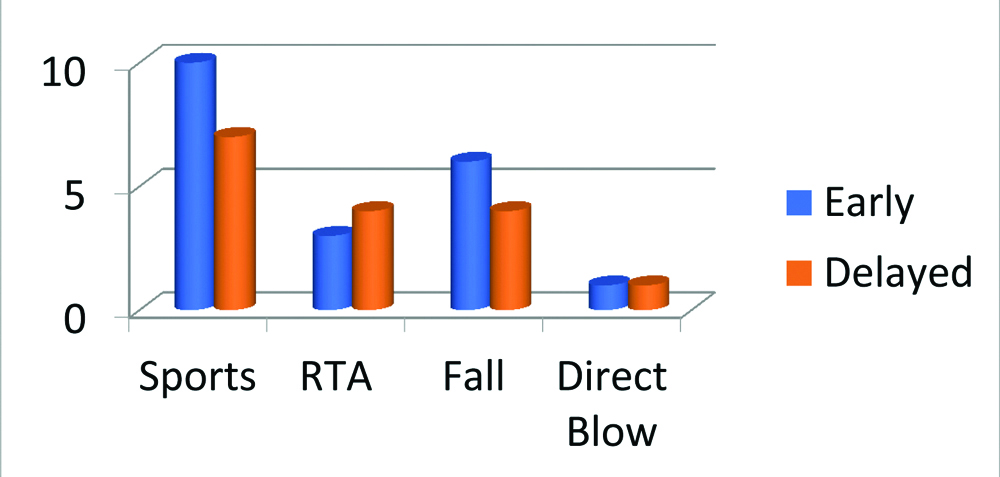
There was higher incidence of injury on the right side in both the groups. Sports injuries were the most common mode of injury, followed by falls and road traffic accidents in both the groups [Table/Fig-4].
Bar graph showing mechanism of injury.
Time since injury ranged from 2 to 12 weeks in the early group (2.19±0.585 months) and 12 weeks to 13 months (10.5±0.912 months) in the delayed group. In the early group, 6 (15%) out of the 40 patients had grade 3/4 Medial Meniscal (MM) tears, 14 (35%) patients had grade 1/2 MM tears, 4 (10%) patients had Lateral Meniscus (LM) grade 1/2 tears, 6 (15%) had bone contusions, 4 (10%) had an associated Medial Collateral Ligament (MCL) sprain and 2 (5%) patients had a synovial fistula. Four (10%) patients had no associated injuries. Comparison of MM injuries between the two groups was statistically significant (p<0.05) [Table/Fig-5]. The comparison of combined MM and LM injuries between the two groups was also statistically significant (p=0.01). There was no statistical association when comparing the other associated injuries between the two groups.
| Associated injury | Early n (%) | Delayed n (%) | p-value |
|---|
| MM Grade 3/4 | 6 (15) | 14 (43.75) | 0.006 |
| MM Grade 1/2 | 14 (35) | 2 (6.25) | 0.003 |
| Combined ML | 0 | 6 (18.75) | 0.01 |
| LM Grade 3/4 | 0 | 4 (12.5) | 0.07 |
| LM Grade 1/2 | 4 (10) | 2 (6.5) | 0.5 |
| Bone contusions | 6 (15) | 4 (12.5) | 0.7 |
| MCL sprain | 6 (15) | 0 | 0.06 |
| Nil | 4 (10) | 0 | 0.1 |
| Total | 40 (100) | 32 (100) | |
p<0.05 calculated by Chi-square test; p-value >0.05 was considered as statistically significant; MM: Medial meniscal; MCL: Medial collateral ligament; LM: Lateral meniscus
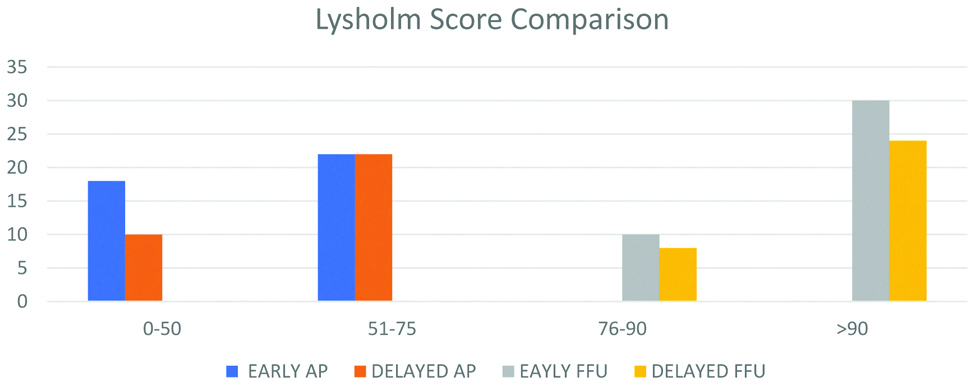
When comparing the pivot shift tests, Lachman tests, Lysholm-Tegner activity levels and single leg hop scores there was no significant statistical association at presentation or at final follow-up (p>0.05) [Table/Fig-6]. The mean thigh wasting at presentation in the early group was 1.65±0.57 cm and in the delayed group was 2.40±0.36 cm and the association between the two groups was statistically significant (p<0.05) [Table/Fig-7]. In comparison the mean thigh wasting at the final follow-up in the early group was 0.98±0.46 cm and at final follow-up was 1.21±0.30 cm and the association between the two groups was found to be statistically significant (p<0.05). In the early group, 16 patients complained of numbness, two of effusion and six had swelling while the remaining 16 did not have any complications whereas in the delayed group six patients had numbness, six had effusion, two each had swelling, pain and synovial fistula and the remaining 14 did not have any complications [Table/Fig-8]. The complications were compared between the two groups and did not have any statistical association. Mean time between injury and surgery in the early group was 2.19±0.585 months and in the delayed group was 10.5±0.912 months.
Bar graph showing the pattern of Lysholm scores At Presentation (AP) and at Final Follow-up (FFU) between the early and delayed group
Comparison of mean thigh wasting.
| Thigh wasting (Average) (in cm) | Early | Delayed | p-value |
|---|
| At presentation | 1.65 | 2.40 | 0.009 |
| Final follow-up | 0.98 | 1.21 | 0.01 |
| Complication | Early n (%) | Delayed n (%) | p-value |
|---|
| Numbness | 16 (40) | 6 (18.75) | 0.05 |
| Effusion | 2 (5) | 6 (18.75) | 0.06 |
| Swelling | 6 (15) | 2 (6.25) | 0.2 |
| Persistent pain | 0 | 2 (6.25) | 0.3 |
| Synovial fistula | 0 | 2 (6.25) | 0.3 |
| Nil | 16 (40) | 14 (43.75) | 0.9 |
| Total | 40 (100) | 32 (100) | |
The complications were compared between the two groups and did not have any statistical association
Discussion
This study was done on two groups, early <12 weeks and delayed >12 weeks and results were compared. A total of 74 patients were included at the beginning of the study, 2 patients were lost to follow-up and finally 72 patients completed the study. Forty (55.55%) patients were in the early group and 32 (44.44%) in the delayed group. Mean time between injury and surgery in the early group was 2.19±0.585 months and in the delayed group was 10.5±0.912 months. Different authors had different results on the time between injury and surgery and on the definition of early and delayed/late. In a study by Brambilla L et al., 80.16 % patients came to the hospital at less than 12 months after injury [11]. Gupta R et al., came to the conclusion that delay in ACL reconstruction lead to an increase in the incidence of associated meniscal and chondral injuries. The mean delay in surgery in their study was 78.91 weeks (range 1 week-18 years) [8]. Mansson O et al., observed associated intra-articular injuries in the long term follow-up of delayed ACL reconstruction [12]. Mean delay was eight months (range 4-9).
Comparison of MM and combined MM & LM injuries was statistically significant (p<0.05). There was no statistical association on comparing the other associated injuries. In the study by Mansson O et al., 18 (62.07%) out of the 29 patients had associated meniscal (medial+lateral) injuries, 2 (6.9%) patients had meniscal injuries along with chondral injuries, 1 (3.5%) patient had lateral collateral ligament sprain, 1 (3.5%) an associated fracture, 1 (3.5%) synovitis,1 (3.5%) pure chondral lesion,1 (3.5%) contralateral ACL injury and 4 (13.53%) had no associated injuries [12]. Krutsch W et al., concluded that associated MM tears (40.3%) were seen more frequently [7]. The MM tears were seen in 39.5% in the early group and in 46.9% patients of the delayed group. The LM tears were seen in 28.4% in the early group and 25% in the late group. Severe cartilage lesions i.e., grade 3/4 were seen in 39.9% in early and 31.3% in the late group. Gupta R et al., inferred that surgical delay beyond six months was associated with significant medial meniscus injuries (p=0.0001) [8]. Bernstein J et al., reached a conclusion that 23% in the early group and 35% in the delayed group required a menisectomy [13]. In the study by Magnussen RA et al., the delay in surgery beyond 12 weeks resulted in more medial compartment injuries {meniscal (p=0.013) and chondral (p<0.0005)}. However, there was no relation to LM injuries [9].
The mean thigh wasting at presentation in the early group was 1.65 cm and in the delayed group was 2.40 cm (p<0.05) [Table/Fig-7]. In comparison the mean thigh wasting at the final follow-up in the early group was 0.98 cm and at final follow-up was 1.21cm (p<0.05). Fowler PJ et al., did a retrospective analysis of 49 ACL deficient knees [14]. The data was analysed by retrieving thigh girth measurements at follow-up visits and significant thigh wasting was seen in 40 patients. Jarvinen M et al., in their study found out that there was significant thigh wasting in 30% of their patients who underwent reconstruction for chronic ACL injuries [15]. The mean thigh wasting at final follow-up for early and delayed intervention, as reported in the previous studies and the present study has been compared in [Table/Fig-9].
Comparison of various studies.
| Parameter | Our study | Fowler PJ and Regan WD, [14] | Jarvinen M et al., [15] | Brambilla L et al., [11] | Gupta R et al., [8] | Mansson O et al., [12] |
|---|
| Mean thigh wasting at final follow-up (in cm) | Early-0.98 Delayed-1.21 | 1.4 cm in Chronic ACL Insufficiency. | 1.29 cm in the delayed. group | | | |
| Time between surgery and injury (in months) | Early-2.19±0.585Delayed-10.5±0.912 | | | 80% of patients came less than 12 months post injury. | The mean delay in surgery was 19.7 months. | Mean Delay-8 months. |
Limitation(s)
Sample size taken for study was small and a future study with a larger sample size is desired. Most of the patients in the study were males so groups were not comparable on basis of gender. Most of the patients were army personnel so the results may not be generalisable.
Conclusion(s)
Delay in ACL reconstruction surgery predisposes to higher grade meniscal lesions and significant thigh wasting and hence the patients should be explained about these complications and counselled for surgical intervention.
p<0.05 calculated by Chi-square test; p-value >0.05 was considered as statistically significant; MM: Medial meniscal; MCL: Medial collateral ligament; LM: Lateral meniscus
The complications were compared between the two groups and did not have any statistical association
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 02, 2020
Manual Googling: Feb 10, 2021
iThenticate Software: Apr 10, 2021 (6%)
[1]. Gupta R, Malhotra A, Sood M, Masih GD, Is anterior cruciate ligament graft rupture (after successful anterior cruciate ligament reconstruction and return to sports) actually a graft failure or a re-injury?J Orthop Surg (Hong Kong) 2019 27(1):230949901982962510.1177/230949901982962530782075 [Google Scholar] [CrossRef] [PubMed]
[2]. Evans J, Nielson Jl, Anterior cruciate ligament knee injuries. [Updated 2020 Aug 10]In: StatPearls [Internet] 2020 Jan Treasure Island (FL)StatPearls Publishing [Google Scholar]
[3]. Casteleyn PP, Handelburg F, Non operative management of anterior cruciate ligament injuries in the general populationJ Bone Joint Surg Br 1996 78:446-51.10.1302/0301-620X.78B3.0780446 [Google Scholar] [CrossRef]
[4]. Daniel DM, Stone MI, Dobson BE, Fithian DC, Rossman DJ, Kaufmann Fate of the ACL injured patient: A prospective outcome studyAm J Sports Med 1994 22:632-44.10.1177/0363546594022005117810787 [Google Scholar] [CrossRef] [PubMed]
[5]. Dunn KL, Lam KC, Valovich McLeod TC, Early operative versus delayed or nonoperative treatment of anterior cruciate ligament injuries in pediatric patientsJ Athl Train 2016 51(5):425-27.10.4085/1062-6050.51.5.1127244126 [Google Scholar] [CrossRef] [PubMed]
[6]. Bottoni CR, Liddell TR, Trainor TJ, Freccero DM, Lindell KK, Postoperative range of motion following anterior cruciate ligament reconstruction using autograft hamstrings. A prospective, randomized clinical trial of early versus delayed reconstructionsAm J Sports Med 2008 4(36):656-62.10.1177/036354650731216418212347 [Google Scholar] [CrossRef] [PubMed]
[7]. Krutsch W, Zellner J, Baumann F, Pfeifer C, Nerlich M, Angele P, Timing of anterior cruciate ligament reconstruction within the first year trauma and its influence on treatment of cartilage and meniscus pathologyKnee Surg Sports Traumatol Arthrosc 2015 25(2):418-25.10.1007/s00167-015-3830-226475153 [Google Scholar] [CrossRef] [PubMed]
[8]. Gupta R, Masih GD, Chander G, Bachhal V, Delay in surgery predisposes to meniscal and chondral injuries in anterior cruciate ligament deficient kneesInd J Orthop 2016 50(5):492-98.10.4103/0019-5413.18960627746491 [Google Scholar] [CrossRef] [PubMed]
[9]. Magnussen RA, Pedroza AD, Donaldson CT, Flanigan DC, Kaeding CC, Time from ACL injury to reconstruction and the prevalence of additional intra-articular pathology: Is patient age an important factor?Knee Surg Sports Traumatol Arthrosc 2013 21(9):2029-34.10.1007/s00167-013-2380-823334624 [Google Scholar] [CrossRef] [PubMed]
[10]. Tambe AD, Godiff SP, Mulay S, Joshi M, ACL insufficiency: Does delay in index surgery affect outcome in recreational athletesInt Orthop 2006 30(2):104-09.10.1007/s00264-005-0055-x16501976 [Google Scholar] [CrossRef] [PubMed]
[11]. Brambilla L, Pulici L, Carimati G, Quaglia A, Prospero E, Bait C, Prevalence of associated lesions in anterior cruciate ligament reconstruction: Correlation with surgical timing and with patient age, sex, and body mass indexAm J Sports Med 2015 43(12):2966-73.10.1177/036354651560848326473010 [Google Scholar] [CrossRef] [PubMed]
[12]. Månsson O, Sernert N, Rostgard-Christensen L, Kartus J, Epub 2014. Long-term clinical and radiographic results after delayed anterior cruciate ligament reconstruction in adolescentsAm J Sports Med 2015 43(1):138-45.10.1177/036354651455567325384503 [Google Scholar] [CrossRef] [PubMed]
[13]. Bernstein J, Early versus delayed reconstruction of the anterior cruciate ligament: A decision analysis approachJ Bone Joint Surg Am 2011 93(9):122510.2106/JBJS.J.0122521543669 [Google Scholar] [CrossRef] [PubMed]
[14]. Fowler PJ, Regan WD, The patient with symptomatic chronic anterior cruciate ligament insufficiency. Results of minimal arthroscopic surgery and rehabilitationAm J Sports Med 1987 15(4):321-25.10.1177/0363546587015004053661812 [Google Scholar] [CrossRef] [PubMed]
[15]. Jarvinen M, Natri A, Lehto M, Kannus P, Reconstruction of chronic anterior cruciate ligament insufficiency in athletes using a bone-patellar tendon-bone autograft. A two-year follow-up studyInt Orthop 1995 19(1):01-06.10.1007/BF001849067768652 [Google Scholar] [CrossRef] [PubMed]