Hypospadias is one of the most common congenital anomaly occurring in children with an incidence of 1 in 200 to 1 in 300 live births [1]. This kind of genital abnormality is a matter of concern for parents requiring correction in the form of urethroplasty before the child goes to school. Considering the variable anatomy of this congenital defect, complications following hypospadias surgery are also very common [2], the most common being fistula formation, meatal stenosis or meatal dehiscence. Hence, to provide a complication-free cosmetically-acceptable outcome, repair remains a challenge for all those who are involved in surgical correction of this anomaly. No single surgical technique has stood the test of time as gold standard for hypospadias repair. It is the experience of surgeon in modifying and refining the technique that he practices routinely which can improve the outcome to a large extent.
Standardised surgical technique like Snodgrass Tubularised Incised Plate (TIP) urethroplasty with a covering layer of tunica vaginalis flap is the most commonly practiced procedure for proximal hypospadias without significant chordee [3,4] and for those with chordee, chordee correction and Bayer’s flap followed by tubularisation of ventral skin in second stage with a covering layer of tunica vaginalis flap is the option [5].
The aim of the study was to highlight the complications and outcome of urethroplasty for proximal hypospadias in children using two standardised surgical techniques with intermediate layer of vascularised flap.
Materials and Methods
A retrospective study was conducted among the patients operated by the Paediatric Surgery Unit at a tertiary care hospital, between March 2017 till February 2019. The study data was retrospectively analysed during the period June 2020 to August 2020. The data relating to urethroplasty for proximal hypospadias in children between the age group of 2-13 years were analysed retrospectively. Informed consent for surgery was obtained from the parents of each patient and the study was approved by institutional ethics committee (letter number KIIT/KIMS/IEC/320/2020).
The anatomical abnormality in terms of position of meatus, penile chordee, age at operation, type of surgical procedure, early and late complications during follow-up period were noted.
Inclusion criteria: Children with penoscrotal, proximal, mid and distal penile hypospadias where meatus was situated 1.5 cm proximal to tip of glans penis with or without chordee were included in the study.
Exclusion criteria: All cases of distal hypospadias with meatus at or less than 1.5 cm to the tip of glans penis (coronal, sub coronal and glandular) and failed urethroplasty cases.
Surgical Procedure
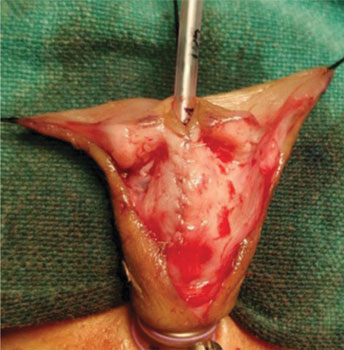
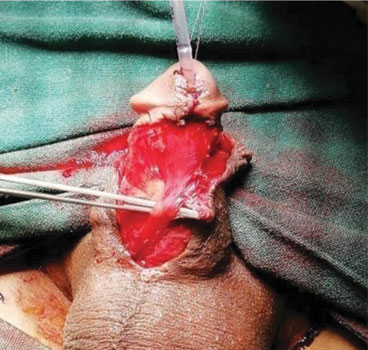
Children with penile chordee had to undergo chordee correction and Bayer’s flap procedure [6,7] followed by urethroplasty after six months [Table/Fig-1]. Here, the neourethra was created from the strip of ventral skin using inverted extra-epithelial continuous sutures of 6.0 polydiaxone over no 8F or 10F feeding tube depending on the age of the child. This feeding tube was kept as urethral stent cum urinary catheter in the postoperative period. Patients having no significant penile chordee had undergone primary TIP urethroplasty [Table/Fig-2] as described by Snodgrass in Baskin LS and Ebbers MB study [1]. In these patients also, neourethra was tubularised over no 8F or 10F feeding tube as urethral stent cum urinary catheter [Table/Fig-3]. In both types of urethroplasty, neo-urethra was covered by vascularised tunica vaginalis flap, except in four cases where dartos-vascularised flap was used due to absence of tunica vaginalis [8].

Tubularised Incised Plate with flap.
TIP with urethral catheter as stent.
Intermediate layer cover: After degloving penile skin up to the root of scrotum, a window was created and testis delivered through same wound. Tunica vaginalis configured into a vascularised flap. Then the testis was pushed back to scrotal sac and scrotal dartos layer repaired after proper haemostasis without any drain [8-10]. Intermediate layer covered whole length of neourethra up to the glans tip, followed by glansoplasty and penile skin reconstruction. In most of the cases of TIP and staged procedure, tunica was put as intermediate layer except in four patients where dartos vascularised flap was harvested from dorsal prepuce and penile skin [Table/Fig-4,5] [11,12].

Staged urethroplasty with TV flap.
TV: Tunicavaginalis

As per the routine postoperative care, all patients following surgery were provided with good compression dressing applied to the penile shaft. Three layered wound dressing was done in all the cases. Inner single layer of bactigrass followed by three to four layers of gauze to absorb the blood and collections, then a layer of dynaplast to secure everything in place. Inner layer of bactigrass was used for easy and pain free removal [13]. Feeding tube as urethral stent cum urinary catheter was kept for 10 days. Bed rest and prophylactic antibiotics (ceftriaxone and amikacin) with anticholinergics (Tolteredine) were given for 10 days. First dressing was changed on 5th and catheter removed on 10th postoperative day. All the patients without any complications were discharged same day and those with minor fistula were re-catheterised with an indwelling Foley’s catheter of appropriate size before discharge. They were followed-up in OPD after 10 days for removal of catheter.
Statistical Analysis
Descriptive statistical analysis was used using MS-Excel. Data is presented in form of frequency and percentage for categorical data and mean/average for continuous data.
Results
A total number of 31 patients were included in this study group, after excluding 17 patients of distal and recurrent failed hypospadias. Urethroplasty in children was performed in two age groups- between four-seven years and between 10-13 years with mean age of 7.31 years.
Twenty patients had significant penile chordee (penoscrotal-12, proximal penile-1, and mid penile-7) [Table/Fig-6]. In all these patients, two staged urethroplasty was done with tunica vaginalis flap as intermediate layer. Rest 11 patients who had minor or no chordee (midpenile-two and distal penile with meatus 1.5 cm at or proximal to the tip of glans penis- nine), underwent TIP urethroplasty with tunica flap in seven and dartos flap in four due to absence of tunica vaginalis (two cases had bilateral herniotomy for inguinal hernia and two cases had bilateral orchidopexy for undescended testis) [Table/Fig-7]. In the study, the age of the patients ranged from two to 13 years with mean age at urethroplasty being 7.31 years.
Demography of hypospadias.
| Diagnosis | Frequency (n) | Percent (%) |
|---|
| Penoscrotal with chordee | 12 | 38.70 |
| Proximal penile with chordee | 1 | 3.22 |
| Midpenile with chordee | 7 | 22.58 |
| Midpenile without chordee | 2 | 6.45 |
| Distal penile with meatus >1.5 cm below glans tip without chordee | 9 | 29.03 |
| Total | 31 | 100 |
| Surgical procedure | Frequency (n) | Percent (%) |
|---|
| Staged with TVF | 20 | 64.5 |
| TIP with TVF | 7 | 22.58 |
| TIP with dartos | 4 | 12.90 |
| Total | 31 | 100.0 |
TVF: Tunicavaginalis flap; TIP: Tubularised incised plate
Out of 27 patients of urethroplasty with tunica vaginalis as intermediate layer, three had minor fistula following removal of catheter. They were followed-up in OPD after re-catheterisation with appropriate indwelling Foley’s catheter for 10 days and had spontaneous healing of the fistula. One patient had large sub-coronal early fistula with dehiscence of glansoplasty and was re-operated after six months. Two patients developed meatal stenosis on follow-up and improved on regular meatal dilatation. No patient had urethral stricture, skin flap necrosis, scrotal haematoma or testicular atrophy. However, there was ipsilateral pulling up of testis in four patients. One of the four patients who had TIP repair with dartos flap as intermediate layer developed late urethrocutaneous fistula after two weeks of discharge from hospital and required re-operation after six months. Other three patients had no complications [Table/Fig-8].
| Intermediate layer | Complications | Frequency (n) | Percent (%) |
|---|
| Tunicavaginalis flap | Nil | 17 | 62. 92 |
| Early fistula | 4 | 14.81 |
| Late fistula | Nil | 00 |
| Meatus stenosis | 2 | 7.40 |
| Pulling up of testis | 4 | 14.81 |
| Dartos flap | Nil | 3 | 75.0 |
| Late fistula | 1 | 25.0 |
During mean follow-up of one year (ranging from six months to two years), three patients required catheterisation, two meatal dilatations and two re-operations (one with early fistula and wound dehiscence, another for late fistula) after 6 months. Four patients had slight upward pulling of ipsilateral (site of Tunicavaginal (TVT) flap) testis [Table/Fig-9].
Follow-up outcomes of procedures.
| Follow-up outcomes | Frequency (n) | Percent (%) |
|---|
| Good cosmesis | 20 | 64.51 |
| Catheterisation | 3 | 9.67 |
| Meatus dilatation | 2 | 6.45 |
| Re-operation | 2 | 6.45 |
| Ipsilateral pulling up of testis | 4 | 12.90 |
| Total | 31 | 100.0 |
Discussion
The result of hypospadias repair depends mostly on the type of surgical techniques and experience of the surgeon [8,9,14]. The choice of technique of hypospadias repair also depends on the components of this anomaly namely urethral plate size, penile chordee, size of phallus/glans and location of meatus [8,14]. The ultimate goal of repair is to provide a straight penile shaft with meatus at the tip as far as possible. In this study, additional layer of vascularised flap in two standardised techniques of urethroplasy helped in preventing fistula formation and wound dehiscence.
In the study, 27 out of 31 patients, tunica vaginalis was used as intermediate layer. Four patients had early urethrocutaneous fistula (14.8%), two patients had meatal stenosis (7.4%) and four had slight pulled up ipsilateral testis (14.8%). In other four patients of TIP urethroplasty where dartos was used as intermediate layer, one patient was re-operated for late urethrocutaneos fistula at corona glandis (25%). The staged repair of hypospadias with tunica vaginalis flap cover gives excellent cover to neourethra as mentioned by Kadian YS et al., 18 out of total 22 (81.8%) had successful functional and cosmetic outcome [8]. This is comparable to the present study.
Whenever there is chordee, it is better to have a graded correction and staged repair [15]. The staged procedure suits most of the patients from proximal presentation than that of distal. Primary repair using TIP urethroplasty for distal and mid-penile hypospadias is also a well-accepted technique, where minimal chordee (<30 degree) almost gets corrected by degloving the penile shaft skin. Patient with proximal hypospadias who underwent staged repair had less complication as compared to single staged repair [16,17].
In comparison to staged procedure, primary repair using TIP in both proximal and distal hypospadias gives similar result. But in these two types of repair, the role of vascularised flap in preventing wound related complications like urethrocutaneous fistula and wound dehiscence is well-established and practiced. Use of tunica vaginalis flap, whenever possible, gives good protection to urethral suture line [8,18]. Good vascularity and easy availability is the main advantage of tunica vaginalis flap which is not affected by penile disorders. This flap for wrapping the neourethra was first used by Snow BW [19]. In this study, out of 27 patients where tunica vaginalis flap was used as intermediate layer, 4 (14.8%) had urethrocutaneous fistulas of which three had minor fistula and healed spontaneously with 10 days of re-catheterisation. Only one patient (3.7%) required delayed repair. The overall incidence of urethrocutaneous fistula following repair of hypospadias varies from 0-23% [20]. With tunica vaginalis flap as intermediate layer, the incidence of fistula reduces to 0-5% [8,11,18]. In present study, among four patients (TIP) where dartos flap was used one presented with delayed urethrocutaneous fistula (incidence 25%) at the corpora glandular junction and required surgical repair later. KadianYS et al., showed that tunicavaginalis flap cover of neourethra in stage repair gives good result. Dhua AK et al., compared tunica vaginalis with dartos flap as soft tissue cover in primary hypospadias repair and their result showed TVF may have an edge over dartos fascia for soft tissue coverage of the neourethra [8,18].
Use of tunica vaginalis flap as an intermediate layer has been advocated by many and in this study, older children were having thick tunica layer to be wrapped over the neourethra and perform a glansplasty over it. It needs more dissection of the glans wing for glansplasty and gives a bulky appearance to penile shaft. One of older patients had dehiscence of glansplasty and urethrocutaneous fistula with tunica vaginalis flap. The probable reason could be an increased wound tension due to bulky tunica and postoperative oedema. Therefore, in older children it is better to use adequate size stent for creation of urethral tube and to replace it with a small size indwelling catheter for the purpose of urinary drainage. A patient undergoing surgery in adulthood should be counseled on all of these variables to avoid unreasonable expectations [21,22].
In the present study, no separate incision was given over the scrotum to deliver the testis nor was any drain put to prevent scrotal hematoma or abscess. The complication like slight pull up of ipsilateral testis was observed in four older children without penile torque (14.8%) but no infection or testicular atrophy. Pattaras JG and Rushton HG found penile torque after the use of tunica vaginalis wrap in hypospadias repair [23]. Dartos flap are available locally and don’t require another incision but the incidence of urethrocutaneous fistula and skin necrosis is higher in comparison to tunica vaginalis flap [10,11]. Dartos flap may cause damage to intrinsic blood supply of skin leading to more necrosis. Babu R and Hariharasudhan S found tunica vaginalis flap is superior to inner preputial dartos flap as a waterproofing layer for primary TIP repair [24].
Adequate pressure dressing has a significant role in preventing hematoma, postoperative oedema, displacement of urethral catheter, but also carries the risk of ischemia, infection and pain during removal [25]. In present study, three layered wound dressing was used. Inner single layer of bactigrass followed by three to four layers of gauze to absorb the blood and collections, then a layer of dynaplast to secure everything in place. Inner layer of bactigrass was used for easy and pain free removal [13].
Limitation(s)
Limitation of this study is the small sample size.
Conclusion(s)
Vascularised intermediate layer should be used routinely in all proximal hypospadias repair, as it prevents wound dehiscence and fistula formation to a large extent. Tunica vaginalis flap proved to be an excellent intermediate layer but one has to be cautious not to have testis related complications. Routine use of indwelling catheter, prophylactic IV antibiotics and anticholinergics prevents wound related complications. Minor early leaks after intermediate layer cover do heal with prolong catheterisation and not necessarily need another surgery.
TVF: Tunicavaginalis flap; TIP: Tubularised incised plate