A Supraglottic Airway Device (SAD) is defined as a device designed to maintain a clear airway, which sits outside the larynx and creates a seal around it [1]. The SAD being a non-invasive airway device is an useful alternative for spontaneous/controlled ventilation with minimal cardiovascular and respiratory disturbances [2,3].
There is an increasing use of SAD in children because of its availability, ease of insertion, minimal disturbances in cardiovascular and respiratory system, lesser risk of airway injury during the perioperative period [4-6]. The lack of laryngeal stimulation makes the SAD a potentially attractive alternative in children with upper respiratory tract infections [7]. An introduction of a new airway device into clinical anaesthesia practise has to fulfil various criteria. This becomes all the more important in paediatric population who have very minimal cardiovascular and respiratory reserves. Studies to evaluate the clinical safety of SAD plays a very important role in the safe practice of paediatric anaesthesia. This study was conducted to evaluate the efficacy of P-LMA and I-GEL in paediatric patients.
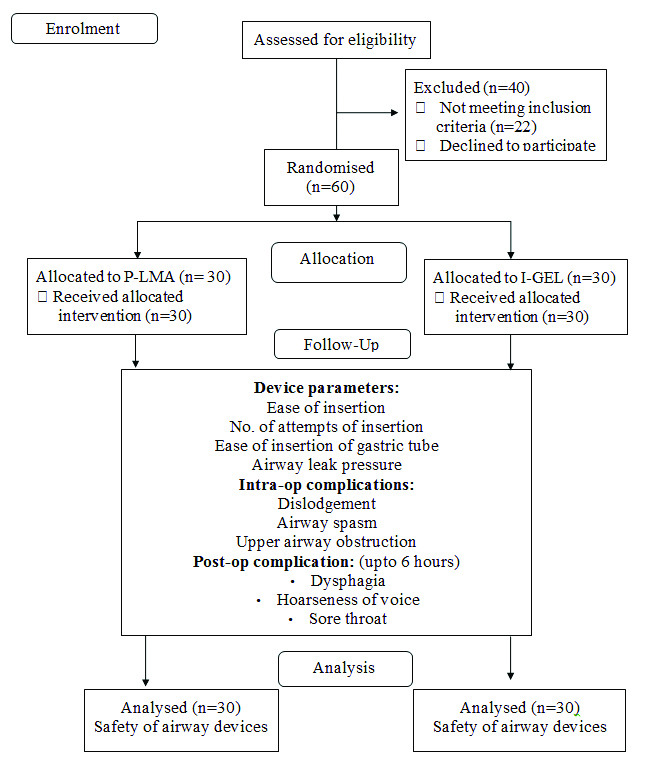
The objectives of this study were to compare parameters like ease and number of attempts of insertion, ease of insertion of gastric tube, leak airway pressure, efficacy during positive pressure ventilation and postoperative complications. When an airway device satisfies these criteria only then can they be safely used in clinical practise. The second objective was to assert whether SAD is a safe device for clinical use in paediatric population.
Materials and Methods
The randomised clinical trial was conducted at a tertiary care hospital attached to JJM Medical College, Davanagere, Karnataka, India. The study period was from July 2015 to August 2017. After obtaining Institutional Ethical Committee clearance (ECR/731/ Inst/KA/2015), verbal and written consent of parent/guardian was taken.
Sample size calculation: Sample size was calculated based on previous studies [8-10]. The mean difference of 3.4 between the groups for airway sealing pressure with a standard deviation of 3.8 for a type 1 error of 0.05 and a power of 0.8 has been considered. The minimum sample size needed was 20 cases in each group. Finally, 60 cases were selected and allocated into two groups (30 in each Group) based on random sampling method.
The study population was randomly divided into two groups P-LMA (Proseal LMA) and I-gel, by computer generated randomisation table, with 30 children in each group.
Inclusion criteria
Children aged between 2-10 years of both gender
Children belonging to ASA grade I and II
Children posted for elective short surgical procedures
Exclusion criteria
Emergency surgeries
Children posted for head and neck surgeries
Syndromic children with airway anomalies
A thorough preanesthetic evaluation was done for all patients on previous day of surgery and the routine investigations were done. Standard Nil Per Oral (NPO) guidelines were given. On the day of surgery, children were premedicated with oral midazolam syrup 0.5 mg/kg body weight 30 minutes before surgery in the preoperative holding room. Intravenous (IV) line was secured and fluid started based on Holiday and Segar formula [11].
On arrival of the child into the operation theatre, monitors like pulse oxymeter, Electrocardiogram (ECG), Oxygen saturation (SpO2), Non Invasive Blood Pressure (NIBP) cuff were attached and baseline values were recorded. All children were induced with sevoflurane, oxygen and nitrous oxide. Inj. glycopyrrolate 0.01 mg/kg followed by Inj. fentanyl 2 microgm/kg and succinyl choline 2 mg/kg was given for relaxation. Facemask ventilation performed until conditions were suitable for insertion of airway. Depending on the group to which the child was allotted, either P-LMA or I-GEL of an appropriate size was inserted and secured by an experienced anaesthesiologist.
The ease of insertion of P-LMA/I-GEL was graded as easy, difficult, and impossible based on a subjective scale (1=easy, 2=difficult, 3=unable to pass) [12]. The number of attempts of insertion of device were noted. Correct position of airway device was confirmed with bilateral chest lift, auscultation of breath sounds and normal capnography curves. The device was firmly secured following which anesthesia was maintained with Nitrous Oxide (N2O) (60%)+Oxygen (O2) (40%)+Isoflurane+vecuronium+Intermittent Positive Pressure Ventilation (IPPV) with paediatric circle system.
Subsequently an appropriate size gastric tube was passed through the drain tube of the airway device. The ease of insertion was assessed based on a subjective scale (same as P-LMA/I-gel) [12]. The correct placement of gastric tube was confirmed by insufflation of air into stomach heard by auscultation over the epigastrium. Monitoring of vital signs i.e. heart rate, non-invasive blood pressure, pulse-oximetry, ECG and End tidal carbon dioxide (EtCO2) were done during intraoperative period. Haemodynamic changes were monitored at baseline and then at 5, 10, 15, 20 and 30 minutes after insertion of airway device.
Monitoring of airway leak pressure/leak airway pressure was done intraoperatively. To measure the airway leak pressure, a fresh gas flow of 3 lit/min was set and the expiration valve closed. When an audible leak was heard from the mouth of patient, the airway pressure was recorded as “P” leak. The expiration valve was opened if P leak reached 40 cm of H2O without an audible leak [13,14]. Airway cuff pressure was measured for P-LMA with non-invasive cuff pressure manometer.
At the end of surgery, residual neuromuscular blockade was reversed with Inj. Neostigmine 0.05 mg/kg IV and Inj. Glyco-pyrollate 0.01 mg/kg IV. Airway device was removed when the child was fully awake, return of adequate respiratory efforts and good muscle strength. Oxygen was provided by hood/face mask in recovery room if required.
Intraoperative complications like dislodgement of device, airway spasm and upper airway obstruction were noted. Postoperative complications like dysphagia, hoarseness of voice and sore throat were noted upto six hours in the postoperative period. The methodology is summarised in [Table/Fig-1].
Statistical Analysis
Statistical tests used were Unpaired t-test and Chi-square test. All the values were analysed and expressed as mean±SD. Statistical comparison was performed by repeated measures of variance followed by Unpaired Student t-test and Chi-square test. A probability value p-value <0.05 was regarded as statistically significant.
Results
Device Parameters
In P-LMA group, 16 (53.3%) children were male and 14 (46.7%) were female. In the I-GEL group, 17 (56.7%) children were male while 13 (43.3%) were female. The mean (mean±SD) age of children in P-LMA group was 4.67 (±1.96) years and that of I-gel group was 5.53 (±2.78) years.
Hemodynamic changes in Heart Rate (HR), BP, Mean Arterial Pressure (MAP), SpO2, and EtCO2 were monitored before induction (baseline), then at 5,10,15, 20 and 30 minutes after insertion of airway device [Table/Fig-2,3,4 and 5]. All the haemodynamic parameters were statistically insignificant as the p-value was >0.05.
| Time | P-LMA | I-gel | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| 0 min | 110.53 | 14.393 | 105.60 | 12.073 | 0.15 |
| 5 min | 109.17 | 14.828 | 102.17 | 12.948 | 0.05 |
| 10 min | 103.53 | 16.827 | 101.13 | 14.371 | 0.55 |
| 15 min | 102.63 | 11.696 | 99.03 | 13.150 | 0.26 |
| 20 min | 103.27 | 12.382 | 100.37 | 16.051 | 0.43 |
| 30 min | 104.33 | 11.610 | 104.33 | 11.610 | 0.10 |
p-value >0.05; not significant
| Time | P-LMA | I-gel | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| 0 min | 99.30 | 8.120 | 95.13 | 8.799 | 0.06 |
| 5 min | 98.6 | 9.732 | 94.11 | 8.901 | 0.07 |
| 10 min | 101.63 | 14.482 | 95.90 | 10.812 | 0.09 |
| 15 min | 101.54 | 13.983 | 96.91 | 10.324 | 0.15 |
| 20 min | 102.47 | 12.937 | 97.81 | 11.076 | 0.14 |
| 30 min | 102.97 | 14.644 | 96.93 | 10.956 | 0.08 |
p-value >0.05, not significant
Diastolic Blood Pressure.
| Time | P-LMA | I-gel | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| 0 min | 63.43 | 5.679 | 60.53 | 6.124 | 0.62 |
| 5 min | 62.33 | 5.095 | 60.40 | 7.171 | 0.23 |
| 10 min | 63.73 | 7.817 | 60.67 | 7.617 | 0.12 |
| 15 min | 62.03 | 13.034 | 60.80 | 7.270 | 0.65 |
| 20 min | 63.83 | 6.998 | 61.40 | 7.449 | 0.19 |
| 30 min | 63.80 | 7.540 | 60.80 | 8.045 | 0.14 |
p-value >0.05, not significant
| Time | P-LMA | I-gel | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| 0 min | 75.40 | 6.697 | 72.20 | 6.493 | 0.07 |
| 5 min | 75.93 | 7.783 | 72.40 | 7.835 | 0.09 |
| 10 min | 75.97 | 8.173 | 72.91 | 7.872 | 0.15 |
| 15 min | 76.30 | 8.150 | 72.64 | 7.313 | 0.07 |
| 20 min | 75.53 | 8.903 | 71.94 | 7.394 | 0.10 |
| 30 min | 76.03 | 7.618 | 72.41 | 7.845 | 0.08 |
p-value >0.05; not significant
Ease of insertion: In both groups, the insertion of device was easy in majority of the patients (p-value=0.99) [Table/Fig-6].
Ease of insertion of device.
| Ease of insertion | I-gel N (%) | P-LMA N (%) | p-value(Fisher-exact test) |
|---|
| Easy | 27 (90%) | 27 (90%) | 0.99 |
| Difficult | 3 (10%) | 3 (10%) |
| Impossible | 0 | 0 |
Number of attempts: In P-LMA group, device was inserted in first and second attempt in 83.3% and 90% in I-gel group (p-value=0.70) [Table/Fig-7].
Number of attempts for insertion of device.
| No. of attempts | I-gel N (%) | P-LMA N (%) | p-value(Fisher-exact test) |
|---|
| 1 | 27 (90%) | 25 (83.3%) | 0.70 |
| 2 | 3 (10%) | 5 (16.7%) |
| 3 | 0 | 0 |
Ease of gastric tube insertion: The gastric tube insertion in P-LMA and I-gel was easy in 80% and 90%, respectively (p-value=0.47) [Table/Fig-8].
Ease of gastric tube insertion.
| Ease of insertion | I-gel N (%) | P-LMA N (%) | p-value(Fisher-exact test) |
|---|
| Easy | 27 (90%) | 24 (80%) | 0.47 |
| Difficult | 3 (10%) | 6 (20%) |
| Impossible | 0 | 0 |
Leak airway pressure/airway sealing pressure: There was no statistically significant difference between P-LMA and I-gel with regard to leak airway pressure [Table/Fig-9].
Leak airway pressure/airway sealing pressure (in cm of H2O).
| Leak airway pressure | I-gel | P-LMA | p-value (Fisher-exact test) |
|---|
| 0 min | 24.17±1.39 | 23.07±2 | 0.55 |
| 30 min | 23.7±1.78 | 23.4±2.25 | 0.57 |
Airway Parameters
Oxygen saturation and end tidal carbon dioxide values: There was no statistically significant difference between P-LMA and I-gel with regard to SpO2 and EtCO2 values at various time intervals [Table/Fig-10].
Oxygen saturation and end tidal carbon dioxide values.
| Time (min) | SpO2 | Time (min) | EtCO2 |
|---|
| P-LMA Mean±SD | I-GEL Mean±SD | p-value(Fisher-exact test) | P-LMA Mean±SD | I-GEL Mean±SD | p-value(Fisher-exact test) |
|---|
| 0 | 98.50±0.820 | 99.50±0.682 | 0.28 | 0 | 33.27±7.292 | 33.40±3.953 | 0.93 |
| 5 | 98.73±0.944 | 96.27±16.499 | 0.41 | 5 | 33.17±6.843 | 34.37±5.561 | 0.45 |
| 10 | 98.83±1.085 | 95.87±18.131 | 0.42 | 10 | 32.70±7.415 | 33.83±5.233 | 0.49 |
| 15 | 96.10±16.283 | 98.93±0.907 | 0.37 | 15 | 33.53±7.343 | 32.97±6.026 | 0.74 |
| 20 | 98.70±1.088 | 99.23±0.728 | 0.29 | 20 | 32.63±7.911 | 33.00±4.571 | 0.82 |
| 30 | 98.50±0.820 | 99.37±0.809 | 0.12 | 30 | 33.37±7.393 | 33.80±5.346 | 0.79 |
Complications
Intraoperatively, dislodgement of the device was noted in 1 (3.33%) child in each group. Postoperatively, all the children were monitored and followed up for 6 hours during which sore throat was observed in 2 (6.66%) and 4 (13.33%) children in I-gel and P-LMA group respectively [Table/Fig-11].
Intraoperative and post operative complications.
| Complications | Variables | I-gel N (%) | P-LMA N (%) | p-value (Fisher-exact test) |
|---|
| Intraoperative complications | Airway spasm | 0 | 0 | 0.99 |
| Dislodgement | 1 (3.33%) | 1 (3.33%) |
| Upper airway obstruction | 0 | 0 |
| Postoperative complications | Sore Throat | 2 (6.66%) | 4 (13.33%) | 0.99 |
| Dysphagia | 1 (3.33%) | 2 (6.66%) |
| Hoarseness of Voice | 0 | 0 |
Discussion
Evaluation of P-LMA and I-gel was conducted with regard to the device, their effect on the airway and associated complications. Both the devices were comparable with regard to the parameters studied. The haemodynamic changes observed in both the device groups were comparable to each other with no statistical significance.
The device insertion parameter was similar in both groups among 90% of the children. Similar conclusion was given by Mitra S et al., and Saran S et al., in their study among paediatric population [15,16]. 98% success rate for insertion of I-gel within two attempts was reported by Beringer RM et al., [17] Singh I et al., concluded that I-gel is easier to insert, requires less attempts, has easier gastric tube placement and is less traumatic as compared to P-LMA [18].
Mitra S et al., reported a success rate among 97% and 83% of children with I-gel and P-LMA, respectively; Shin WJ et al., found that paediatric I-gel insertion was easier with less number of attempts compared to P-LMA; whereas Beringer RM et al., reported a success rate of paediatric I-gel insertion during first and second attempt in 92% and 7% of children, respectively [15,17,19].
Goldmann K et al., in their comparative study of P-LMA and classic LMA, reported that the device were positioned successfully within 2 attempts. They also stated that P-LMA is an invasive device with potential of clinically relevant upper airway obstruction when compared to Classic LMA. The same precautions should be kept in mind while using P-LMA. The ease of insertion of any new airway device mainly depends on the user’s familiarity with the device. The patients’ outcome can be improved in emergency situations such as “can’t ventilate can’t intubate” scenario with an easy-to use supraglottic airway device [20]. An inexperienced or untrained user may find insertion of SAD as a difficult task especially in emergency situation [21-24]. White MC et al., suggested that insertion of P-LMA is successful in the first attempt even without prior experience of the anaestheiologist [1]. In this study, all the anaesthesiologists were experienced and had exposure to paediatric cases.
The standard insertion techniques recommended by the manufacturer were used in this study. Various techniques with introducer and gum elastic bougie have been compared by many authors [20,25]. P-LMA insertion is easier due to the absence of a rear cuff. The side-by-side presence of the airway tube and drainage tube prevents its rotation during insertion. This is in contrast to the cuff in Classic LMA which folds on itself when deflated and makes its insertion theoretically difficult [7,26].
In this study, insertion of gastric tube was easy in 90% and 80% of patients in I-gel and P-LMA group, respectively. A subjective scale was used for assessing the ease of gastric tube insertion as was done by Jagannathan N et al., [12]. The selection of appropriate size gastric tube was based on the description given by Dorsch JA and Dorsch SE [27]. Ekinci O et al., [28]. They concluded that the success rate of gastric tube placement was higher in the I-gel group (92.5%, first attempt) than in the P-LMA group (72.5%, first attempt). Jagannathan N et al., were successful in passing a gastric drain tube among all children in their study. [12] Goldmann K et al., reported successful introduction of gastric tube without any difficulty in 29 patients with one attempt [19]. They also suggested that a greater degree of protection against aspiration was provided by P-LMA due to avoidance of gastric insufflation and the possibility of emptying the stomach. The above belief is supported by cadaveric study and various case reports [13,29-32].
The EtCO2 curve and values were taken as the confirmatory end points for proper insertion of the airway device along with other parameters like bilateral chest lift and auscultation of breath sounds. Though the time required for airway insertion has not been recorded in this study, capnography recording has been taken to confirm the successful placement of the airway device. There was no statistically significant difference between the 2 groups.
In this study, the mean (±SD) leak airway pressure in P-LMA was 23.4 (±2.25) cm of H2O and for I-gel 23.7 (±1.78) cm of H2O. These findings corelate with other studies [21,33-35]. Goldmann K et al., concluded that P-LMA is better than Classic LMA in children, as it forms a more effective seal due to higher mean P leak which makes P-LMA more suitable in patients with poor pulmonary compliance [36]. Jagannathan N et al., suggested that P-LMA in children provides effective ventilation with pressure control mode and supraphysiologic tidal volume with low airway leak pressure of <15 cm of H2O [12]. Beringer RM et al., suggested that I-gel in children is superior to Classic LMA since the I-gel forms a better airway seal but inferior to that of P-LMA [18].
The P-LMA and I-gel offer the advantage of identifying gastric contents in the drain tube even without any obvious signs of regurgitation. The drain tube in these SADs serve dual purpose of early warning that regurgitation has occurred and potentially prevents aspiration [18].
In this study, there was dislodgement of device in 1 patient in each study group. An incidence of 13.33% of sore throat was noted in P-LMA and only 6.66% in I-gel. Keijzer C et al., found that incidence of post-operative sore throat and neck complaints were more in P-LMA (14.67%) than I-gel (2.75%) [37]. Das B et al., reported a very low incidence of complications (airway trauma, sore throat) which was clinically and statistically insignificant [38] The above findings were supported by Wong DT et al., in their review article that concuded a lower incidence of sore throat with paediatric I-gel, since the device exerts less pressure on perilaryngeal tissue due to its non-inflatable cuff [39]. Various post-operative adverse events like sore throat, dysphonia and dysphagia are mainly dependent on depth of anaesthesia, method of insertion, number of insertion attempts, mode of analgesia, time of anaesthesia and type of post-operative analgesia. These lower incidence of complications may be due to higher rate of success of insertion at first attempt as opined by Francksen H et al., [21]. Beringer RM et al., are of the opinion that the long stem of the I-gel makes it more prone for dislodgement and hence careful taping of the device in place is very much necessary to maintain a good airway seal and involves a learning curve [17].
Limitation(s)
The study parameters may have been highly variable had it been conducted in emergency surgeries, head and neck surgeries.
Conclusion(s)
Paediatric P-LMA and I-gel are comparable to each other with regard to ease of insertion, number of attempts of insertion, ease of gastric tube insertion, airway leak pressure, efficiency of ventilation and fewer complications.