Trochanteric fractures are the most common fractures in the elderly around the world and the incidence is increasing each year [1-3]. One year mortality rate of hip fractures can range from 15-20% [4]. Incidence of trochanteric fractures increases in elderly individuals [5]. Intertrochanteric fractures can be classified as stable or unstable [6,7]. Nearly half of these trochanteric fractures are unstable fractures. These are challenging to treat because the internal fixation should be stable as to mobilise the patient early [8].
There are two popular treatment options for internal fixation of these fractures, extramedullary sliding hip screw with side plate and the intramedullary hip screw [9-11]. Cephalomedullary nails such as Proximal Femoral Nails (PFN) and gamma nails are types of intramedullary nails that are the preferred mode of fixation of unstable intertrochanteric fractures.
Although better clinical outcomes result from PFNs, it is a straight nail and hence, does not match the proximal femur to a high extent leading to complications such as screw cut out, femoral shaft fracture, or pain in the thigh and hip [12]. To overcome this problem, Zimmer natural nails were developed which accommodate the complete anatomical structure of the proximal femur. A handful of studies have shown the performance of Zimmer natural nails for treatment of unstable fractures, however, all of these studies included fractures classified according to their anatomical site [12-14]. There is no study that reports the efficacy of Zimmer natural nail for treating unstable intertrochanteric fractures which has been classified according to the ease or difficulty of securing and maintaining fracture reduction. Moreover, the presence of multiple options available to surgeons poses a challenge for healthcare providers to decide on the ideal implant. Therefore, the aim of this study was to investigate the performance of Zimmer natural nails in the fixation of unstable intertrochanteric fractures.
Materials and Methods
A longitudinal cohort study was carried out on 99 patients suffering from unstable trochanteric fractures admitted to a tertiary care hospital from 1st July, 2015 to 30th July, 2015. Both male and female patients were included in the study. Written informed consent was obtained from all the patients.
Inclusion criteria: Patients with trochanter fracture with posteromedial communition, reverse oblique pattern and subtrochanteric extension were included.
Exclusion criteria: Stable trochanteric fracture cases were excluded from the study.
Sample size calculation: The estimated minimum sample size was calculated:

Where, n=Sample size,
Z=Z statistic for a level of confidence (alpha error=5%),
P=Expected prevalence or proportion (If the expected prevalence was 50%, then P=0.5),
d=Precision was 10%.
For this study, the sample size was calculated at 95% confidence levels, 5% alpha error, and 10% absolute precision [3]. Therefore, the sample size was estimated to be 97.
Data Collection
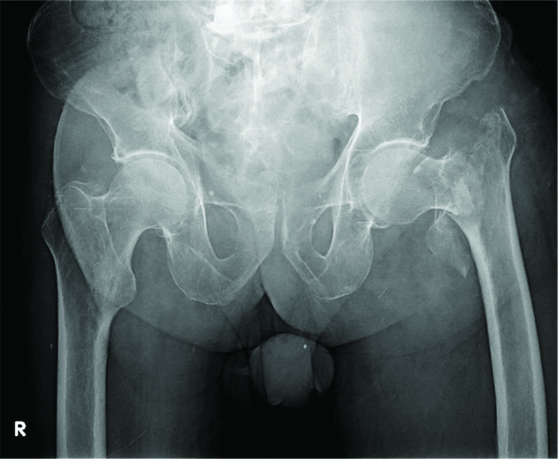
At the time of enrollment, demographic data of patients were collected. All patients underwent thorough clinico-radiological evaluation. Patients were assessed for the presence of co-morbidities which included diabetes mellitus, hypertension, hypothyroidism, and ischaemic heart disease. Fractures were classified based on the criteria by Boyd HB and Griffin LL [15]. This classification categorises fractures into four categories according to the ease or difficulty of securing and maintaining fracture reduction. The categories are: Type I (simple fracture along the intertrochanteric line), Type II (comminuted fractures), Type III (reverse oblique), or Type IV (Fracture in atleast two planes). Type II, III, and IV were considered as unstable [Table/Fig-1].
Radiograph showing left side unstable intertrochanteric fracture.
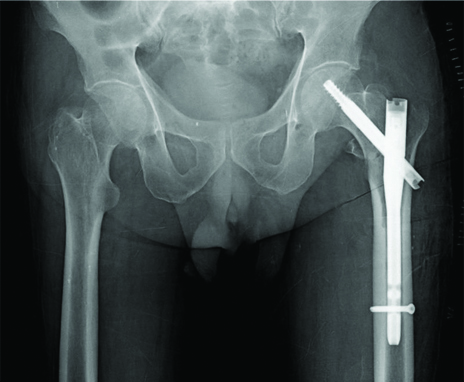
Closed reduction and internal fixation were performed for all the patients with Zimmer natural nail (Zimmer, Warsaw, IN, USA). The surgery was performed by multiple surgeons at two tertiary care hospitals [Table/Fig-2]. The patients were followed at six weeks, three months, and six months postsurgery. At each follow-up examination, fracture healing was assessed by radiography and a Radiographic Union Score for Hip (RUSH) score (10-30 scale) was calculated [16]. Parker score (0-9 scale) was calculated based on the level of mobility of the patients at each follow-up examination [17].
Radiograph showing left Zimmer natural nail in-situ.
Statistical Analysis
Data were analysed using RStudio v3.6.1 and Microsoft Excel 2016. The categorical variable of frequency of patients were expressed as percentages. Continuous variables such as duration of surgery were expressed as mean±Standard Deviation (SD). Chi-square test was performed for comparing categorical variables and ANOVA test was used for continuous variables. A p-value <0.05 was considered statistically significant.
Results
Data were collected from 99 patients with unstable intertrochanteric fracture. Mean age of patients was 69.77 years and the ratio of males to females was nearly 1:0.98. Most patients had Type II fracture, while others had Type III and Type IV. The average duration of surgery was 58.38±9.34 minutes, with no statistically significant difference between each class of fracture [Table/Fig-3].
Demographic and clinical details of the patients.
| Demographic and clinical characteristics | Number of patient (N=99) n (%), Mean±SD |
|---|
| Age (years), Mean±SD | 69.77±11.47 |
| Sex, n (%) | Female | 49 (49.49) |
| Male | 50 (50.51) |
| Co-morbidities, n (%) | Diabetes mellitus | 30 (30.3) |
| Hypertension | 41 (41.41) |
| Hypothyroidism | 2 (2.02) |
| Ischaemic heart disease | 6 (6.06) |
| Location of fracture, n (%) | Left | 54 (54.55) |
| Right | 45 (45.45) |
| Number of fluoroscopic images | 37.15±5.91 |
| Duration of surgerya (minutes), Mean±SD | Type II fracture, n=45 | 60±11.87 |
| Type III fracture, n=26 | 56.15±5.53 |
| Type IV fracture, n=28 | 57.85±6.99 |
| Complications, n (%) | Nil | 93 (93.94) |
| Infection | 2 (2.02) |
| Delayed union | 1 (1.01) |
| Screw cut out | 3 (3.03) |
ANOVA test was used for calculating p-valuea. p-value=0.531
Three patients had lag screw cut out which necessitated implant removal and total hip replacement. Two patients had surgical site infection but responded well to wound debridement. One patient had delayed union which eventually united later and did not required any secondary surgery [Table/Fig-3].
Duration of surgery varied among patients with different classes of fracture and most patients underwent 50-60 minutes of surgery [Table/Fig-4].
Relation of duration of surgery with type of fracture.
| Duration of surgery (minutes) | Type II n=45 | Type III n=26 | Type IV n=28 | p-value |
|---|
| Frequency of patients, n (%) |
|---|
| 45 | 3 (6.67) | 1 (3.85) | 1 (3.57) | 0.772 |
| 50 | 8 (17.78) | 7 (26.92) | 6 (21.43) |
| 55 | 7 (15.56) | 5 (19.23) | 7 (25) |
| 60 | 18 (40) | 12 (46.15) | 8 (28.57) |
| 65 | 2 (4.44) | 0 | 2 (7.14) |
| 70 | 3 (6.67) | 1 (3.85) | 4 (14.29) |
| 80 | 2 (4.44) | 0 | 0 |
| 90 | 1 (2.22) | 0 | 0 |
| 110 | 1 (2.22) | 0 | 0 |
Chi-square test was used for calculating p-value
Parker score of mobility increased consistently with each follow-up examination [Table/Fig-5]. Most patients at six week follow-up checkup had a score of 3, while at three months they had a score of 6. At the end of six months, nearly 90% patients had a high mobility score of 9.
Relation of Parker scores and RUSH scores with type of fracture.
| Type of score | Type II n=45 | Type III n=26 | Type IV n=28 | p-value |
|---|
| Parker score | Frequency of patients, n (%) |
| 6 weeks | 2 | 4 (8.89) | 1 (3.85) | 0 | 0.771 |
| 3 | 30 (66.67) | 18 (69.23) | 19 (67.86) |
| 4 | 8 (17.78) | 5 (19.23) | 6 (21.43) |
| 5 | 3 (6.67) | 2 (7.69) | 3 (10.71) |
| 3 months | 4 | 1 (2.22) | 0 | 0 | 0.616 |
| 5 | 14 (31.11) | 11 (42.31) | 7 (25) |
| 6 | 28 (62.22) | 15 (57.69) | 19 (67.86) |
| 7 | 2 (4.44) | 0 | 2 (7.14) |
| 6 months | 8 | 5 (11.11) | 3 (11.54) | 2 (7.14) | 0.827 |
| 9 | 40 (88.89) | 23 (88.46) | 26 (92.86) |
| RUSH score |
| 6 weeks | 11 | 1 (2.22%) | 1 (3.85%) | 0 | 0.753 |
| 12 | 5 (11.11%) | 2 (7.69%) | 3 (10.71%) |
| 13 | 2 (4.44%) | 0 | 0 |
| 14 | 36 (80%) | 23 (88.46%) | 25 (89.29%) |
| 16 | 1 (2.22%) | 0 | 0 |
| 3 months | 19 | 1 (2.22%) | 0 | 0 | 0.572 |
| 20 | 2 (4.44%) | 0 | 0 |
| 21 | 1 (2.22%) | 0 | 1 (3.57%) |
| 22 | 38 (84.44%) | 26 (100%) | 27 (96.43%) |
| 23 | 1 (2.22%) | 0 | 0 |
| 24 | 2 (4.44%) | 0 | 0 |
| 6 months | 28 | 45 (100%) | 26 (100%) | 28 (100%) | NA |
NA: Not applicable; Chi-square test was used for calculating p-value
The radiological RUSH score also improved at each follow-up examination. Most patients at six week examination had a score of 14, while at three months they had a score of 22. At six month examination, all patients had a score of 28 [Table/Fig-5].
The mean Parker score and RUSH score increased significantly at each follow-up visit [Table/Fig-6]. There was no statistically significant difference between both the scores when compared for each fracture type [Table/Fig-7].
Average Parker score and RUSH score comparison at each follow-up visit.
| Type of score | 6 weeks Mean±SD | 3 months Mean±SD | 6 months Mean±SD | p-value |
|---|
| Parker score | 3.3±0.69 | 5.69±0.56 | 8.89±0.3 | 0.001* |
| RUSH score | 13.73±0.76 | 21.95±0.53 | 28±0 | 0.001* |
ANOVA test was used for calculating p-value. *p<0.05 significant
Average Parker score and RUSH score comparison at each follow-up visit distributed according to the fracture type.
| Type of score | Boyd and Griffin type | p-value |
|---|
| Type II n=45 | Type III n=26 | Type IV n=28 |
|---|
| Parker score | 6 weeks | 3.22±0.7 | 3.31±0.68 | 3.43±0.69 | 0.507 |
| 3 months | 5.69±0.59 | 5.58±0.5 | 5.82±0.54 | 0.11 |
| 6 months | 8.89±0.31 | 8.88±0.32 | 8.93±0.26 | 0.592 |
| RUSH score | 6 weeks | 13.71±0.84 | 13.73±0.77 | 13.78±0.63 | 0.787 |
| 3 months | 21.93±0.78 | 22±0.01 | 21.96±0.18 | 0.816 |
| 6 months | 28±0 | 28±0 | 28±0 | NA |
NA: Not applicable; ANOVA test was used for calculating p-value
Discussion
Cephalomedullary nails are a preferred choice for internal fixation of unstable intertrochanteric fractures, however conventional cephalomedullary nails are associated with a few complications because of their design. Zimmer natural nails were developed to circumvent these complications as they simulate proximal femur anatomy. The aim of this study was to evaluate the efficacy and performance of Zimmer natural nails in the treatment of unstable intertrochanteric fractures.
A total of 99 patients with unstable intertrochanteric fracture were studied in this current study. In a large review of hip fractures in the USA, Karagas MR et al., showed that trochanteric fractures occurred mostly between the ages of 65 to 99 years, with a higher frequency in the age group of 85-99 years [18].
Most patients underwent surgery for an hour to fix the fracture using Zimmer natural nails. The duration of surgery was not significantly different among each class of unstable intertrochanteric fractures. Roh YH et al., have previously found the average surgery duration to be 64 minutes in patients treated with Zimmer natural nails [19]. Persiani P et al., found the average duration of surgery to be 34.63 minutes using natural nails [14]. The difference may have arisen because they included stable as well as unstable intertrochanteric fractures. The differences in the length of duration for internal fixation are not uncommon. A meta analysis by Parker MJ and Handoll HHG has shown that the surgery duration varies to a great extent between different studies that used Gamma nails [9]. A reason for this could be different surgical environment of the hospitals or the efficiency of each surgeon.
The mobility score and radiological scores of healing increased consistently at each follow-up examination (p-value=0.001). Zimmer nails were effective in treating all three categories of unstable intertrochanteric fractures studied here with no statistically significant difference among the three classes. No postoperative complications were observed in 94% of the cases. Current results are consistent with the previous report by Roh YH et al., who showed improved radiological fracture healing and weight bearing without pain with each follow-up [19]. Also, no complications were found in their study. Persiani P et al., found that all the patients who had reverse oblique fracture achieved healing six months postsurgery with a very low complication rate [14]. Previously, our group has shown that Zimmer natural nails resulted in increased radiological healing and mobility in patients with unstable intertrochanteric fractures as compared to PFN [20].
The consistent improved outcome with Zimmer natural nails emphasises their importance in treating unstable fractures. It has been established by Chen J et al. that in fine element analysis, Zimmer natural nails provide biomechanical advantage over PFN when used for reverse oblique unstable fractures [12]. Since Zimmer natural nail is designed to suit the proximal femur anatomy, it provides better support to the fractured fragments and distributes the stress evenly.
In summary, the present study strengthens the previous observations of improved healing and mobility with Zimmer natural nails. Additionally, the study provides better rationale for selecting Zimmer natural nails as it describes their use in the three categories of unstable intertrochanteric fractures.
Limitation(s)
A limitation to this study was the absence of randomisation. Moreover, no comparison was performed with other types of internal fixative devices or with stable fractures.
Conclusion(s)
Zimmer natural nails used in the treatment of unstable intertrochanteric fractures have favourable outcomes. These nails could be preferred for management of such fractures with decreased surgery time, improved radiological and mobility outcomes, and lower complications.
ANOVA test was used for calculating p-valuea. p-value=0.531
Chi-square test was used for calculating p-value
NA: Not applicable; Chi-square test was used for calculating p-value
ANOVA test was used for calculating p-value. *p<0.05 significant
NA: Not applicable; ANOVA test was used for calculating p-value