Iatrogenic Left Main Coronary Artery Dissection Treated with Bare Metal Stents: A Case with Twelve Years Angiographic Follow-up
Shuvanan Ray1, Sunil Jain2, Sabyasachi Mitra3
1 Consultant, Chief of Cardiac Intervention, Department of Cardiology, Fortis Hospital, Kolkata, West Bengal, India.
2 Consultant, Department of Cardiology, Anandalok Hospital, Kolkata, West Bengal, India.
3 Registrar, Department of Cardiology, Fortis Hospital, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Shuvanan Ray, 730, EM Bypass Road, Anandapur, Kolkata-700107, West Bengal, India.
E-mail: shuvananray@gmail.com
Complications during the course of Percutaneous Coronary Interventions (PCI) are common. One of the complications is iatrogenic Left Main Coronary Artery (LMCA) dissection, which is considered as lethal in nature and prevails in around 0.07% PCI cases. Timely diagnosis and immediate revascularisation is mandatory to manage LMCA dissection in order to avoid worsening of patient’s haemodynamic condition and to re-establish antegrade coronary blood flow. Here, authors report a case of catheter-induced iatrogenic LMCA dissection developed during stenting of a lesion in Left Anterior Descending (LAD) coronary artery of a 32-year-old male patient. The patient was managed by implantation of two Matrix (Sahajanand Medical Technologies, Pvt., Ltd., Surat, India) Bare Metal Stents (BMS) using double barrel technique to treat the dissection in left main coronary bifurcation. The patient was regularly followed-up and even after 12 years of the index procedure, the angiographic data revealed good patency of stents in LMCA without any major cardiac events.
Bail-out technique, Bifurcation, Double barrel technique, Simultaneous kissing technique
Case Report
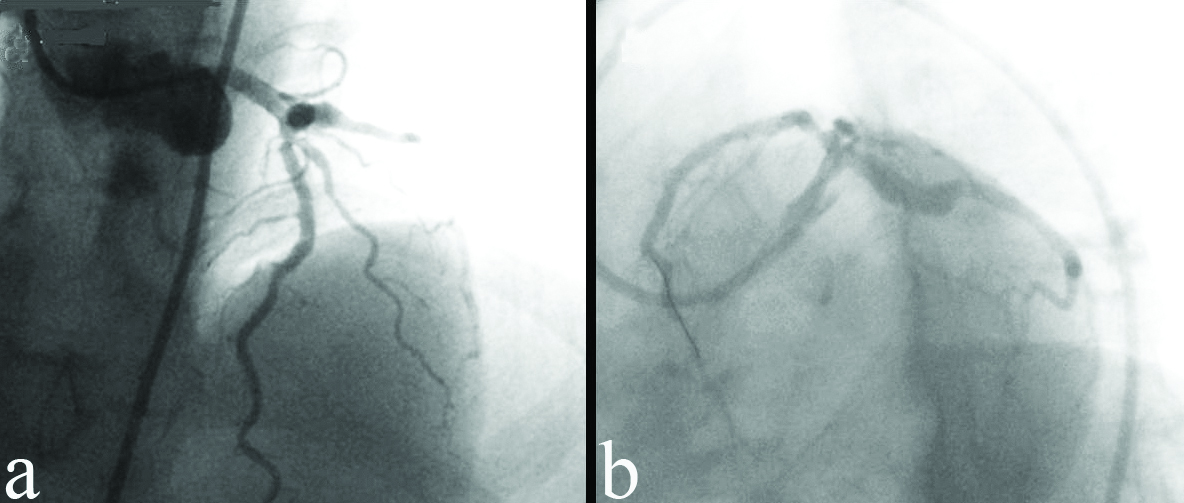
The case represents a male who was non-diabetic, non-hypertensive and a continuous smoker. In 2006, at the age of 32 years, he had undergone coronary angioplasty to treat ostio-proximal Left Anterior Descending (LAD) coronary artery lesion [Table/Fig-1] with implantation of 3×18 mm BxSonic BMS (Cordis Cardiology, FL, USA). However, suddenly after stenting, the patient developed severe chest pain and hypotension. A zipper like type-B dissection was observed in proximal Left Circumflex (LCx) Coronary Artery may be due to the guiding catheter [Table/Fig-2a]. The condition of the patient worsened and in no time he experienced a cardiac arrest. Immediately, cardiopulmonary resuscitation was started to stabilise the patient.
Left coronary angiogram before angioplasty: a) Ostio-proximal lesion in Left Anterior Descending (LAD) artery; and b) left anterior oblique-caudal view showing ostio-proximal lesions in Left Anterior Descending (LAD) artery.
a) Right anterior oblique, cranial projection showing double-lumen (arrow) type-B iatrogenic dissection with contrast dye hang-up in the left main artery; b) Two Matrix 3×28 mm and 3×32 mm bare metal stents deployed using double-barrel technique to seal the dissection in left main bifurcation; and c) Final postprocedure TIMI flow.
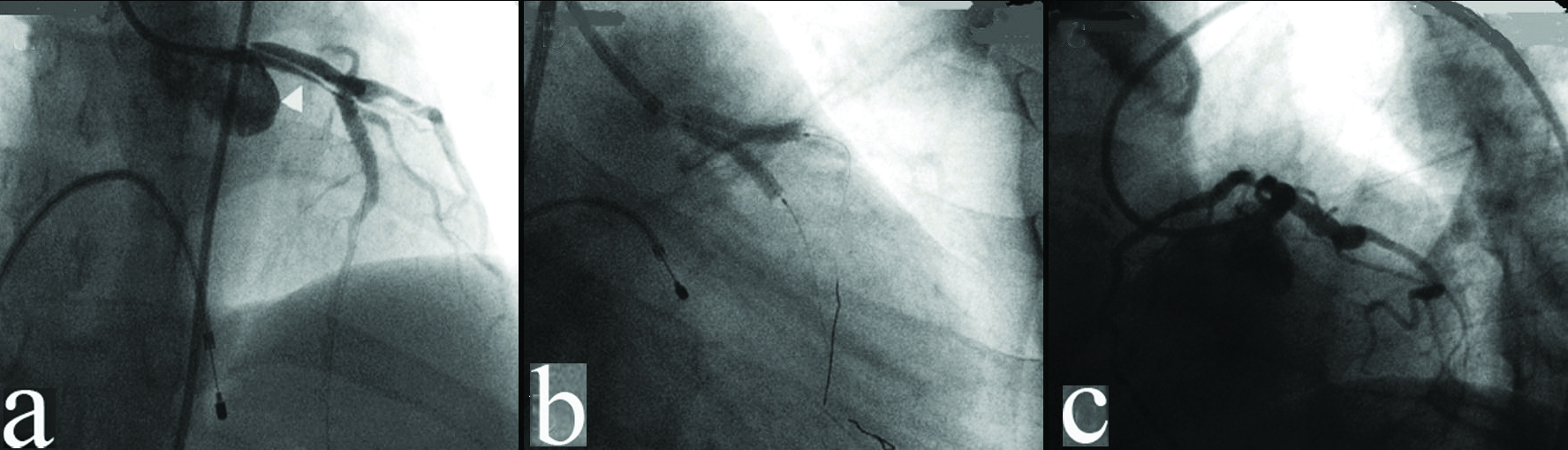
Meanwhile, during cardiopulmonary resuscitation LAD and LCx were wired to seal the dissection. The Left Main Coronary Artery (LMCA) to LAD and LCx were stented using double barrel technique with two Matrix BMS (Sahajanand Medical Technologies, Pvt., Ltd., Surat, India) of 3×28 mm and 3×32 mm size using simultaneous kissing stent deployment technique [Table/Fig-2b] with final Thrombolysis in Myocardial Infarction (TIMI-3) results [Table/Fig-2c]. The patient’s condition was stabilised and he was discharged after four days of coronary angioplasty with clopidogrel 75 mg, aspirin 150 mg and atorvastatin 40 mg once in a day.
After one year, in 2007 the patient came for regular check-up and was stable and asymptomatic. Coronary angiography was performed which showed that LMCA and both branches (LAD and LCx) were open with patent stents. However, one stent in the double barrel in LMCA was blocked with thrombus and the load of circulation was virtually taken-up by another stent in LMCA [Table/Fig-3a]. As the patient was asymptomatic, thrombus was left as it was and the patient was discharged. The patient was advised to continue the same drug regimen (clopidogrel 75 mg, aspirin 150 mg and atorvastatin 40 mg once in a day). The patient came for yearly follow-up on regular basis without any symptoms and was found stable every time.
Follow-up angiogram: a) at one year follow-up, showing one stent in the double barrel in Left Main Coronary Artery (LMCA) was blocked with thrombus; b) at eight years follow-up showing left anterior oblique-cranial view; and c) at 12 years follow-up.
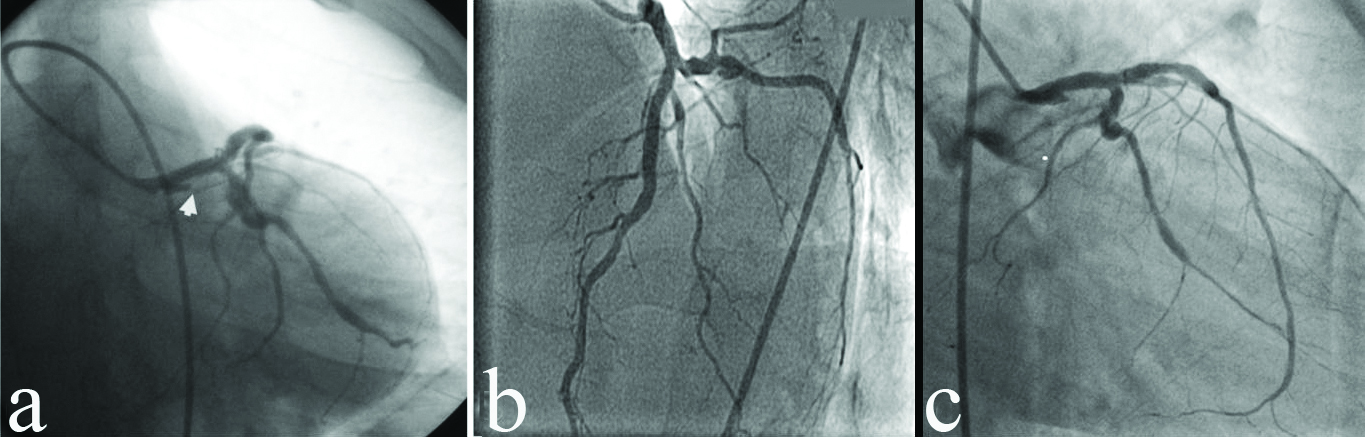
In 2014, after eight years, the patient presented with a complaint of minor chest pain and thus, coronary angiography was performed. Angiogram showed the same result as that observed in 2007, which confirmed that thrombus had not enlarged [Table/Fig-3b]. The patient was asked to continue antiplatelet (Aspirin 150 mg) and atorvastatin 40 mg. Again in 2017, the patient was followed-up by performing coronary angiography which also showed same results as previous with stabilised conditions and no symptoms [Table/Fig-3c].
Discussion
Iatrogenic coronary artery dissections are typically either caused during passage/negotiation of any interventional device or due to any mechanical injury to the arterial wall during the procedure. Iatrogenic LMCA dissection is considered as one of the most devastating complications if not diagnosed and managed immediately. Bail-out stenting using double barrel technique rather than coronary artery bypass surgery is considered as a more favourable practical approach as it permits rapid re-establishment of LMCA patency [1,2].
Here, in the present report, authors encountered a case of guiding catheter-induced iatrogenic type-B LMCA dissection extending up to proximal LCx during stenting of ostio-proximal LAD lesion. The patient suddenly developed haemodynamic deterioration and cardiac arrest, which was immediately stabilised using cardiopulmonary resuscitation. Successful bail-out stenting using double barrel technique [3,4], with implantation of two Matrix BMS at LMCA bifurcation covering proximal LAD and proximal LCx, was performed to seal the dissection as well as to revascularise LAD lesion using simultaneous kissing stent technique.
The simultaneous kissing stent technique is the simplest practical approach for bifurcation lesions. In simultaneous kissing stent technique, the two wires can stay at the site for the entire procedure after initial wiring of the two main vessels. In the present case, as authors were dealing with an unstable patient, we could not afford rewiring and thus, simultaneous kissing stent technique was the best suited according to the patient’s condition. Furthermore, it also offers other advantages such that it does not need separate postdilatation as kissing balloons are always used. It also provides minimum disruption to the stent design compared to other bifurcation techniques [5].
In addition, the development of very late stent thrombosis following BMS implantation is very infrequent due to complete endothelisation of BMS within four weeks of implantation compared to drug-eluting stents. Several studies and case reports in literature have reported very long-term (≥10 years) follow-up of BMS and none of them were without complications [6-10]. Literature also states that the risk of very late stent thrombosis following BMS implantation doubles after 10 years compared to one year [10]. The disruption of in-stent neo-atherosclerosis plays an important role in the pathogenesis of very late stent thrombosis following BMS implantation [10]. However, in the present case, significant thrombus or neo-atherosclerosis were not evident even at 12 years angiographic follow-up. This case demonstrated good patency of BMS at 12 year follow-up in patients with iatrogenic LMCA dissection without any major adverse events. The thin struts (80 μm) and hybrid cell design of Matrix BMS and continuous anti-platelet therapy might have played effective role in clinical performance of both the stents even after 12 years of implantation.
Conclusion(s)
The present case is the case of iatrogenic LMCA dissection without any significant visible thrombosis in coronary angiography, even after 12 years of the index procedure. This case points towards bail-out use of double barrel technique for iatrogenic LMCA dissection and also hint the successful off-label use of BMS and defines the significance of BMS in the era of drug-eluting stents.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 17, 2020
Manual Googling: Mar 04, 2021
iThenticate Software: Apr 17, 2021 (5%)
[1]. Kubota H, Nomura T, Hori Y, Yoshioka K, Miyawaki D, Urata R, Successful bailout stenting strategy against lethal coronary dissection involving left main bifurcationClinical Case Reports 2017 5(6):89410.1002/ccr3.97228588834 [Google Scholar] [CrossRef] [PubMed]
[2]. Jeyakumaran B, Raj A, Pandit BN, Kumar T, Deora S, Iatrogenic left main coronary artery dissection due to pin-hole balloon rupture: Not to be panicked…Acute Cardiac Care 2015 17(4):80-82.10.3109/17482941.2016.117427127283143 [Google Scholar] [CrossRef] [PubMed]
[3]. Damelou A, Davlouros P, Karantalis V, Alexopoulos D, Double-barrel stenting of distal left main stenosis in a patient with acute coronary syndrome: Intravascular ultrasound and optical coherence tomography follow-up at six monthsCan J Cardiol 2010 26(7):e282-85.10.1016/S0828-282X(10)70428-1 [Google Scholar] [CrossRef]
[4]. Teirstein PS, Unprotected left main intervention: Patient selection, operator technique, and clinical outcomesJACC: Cardiovascular Interventions 2008 1(1):05-13.10.1016/j.jcin.2007.12.00119393138 [Google Scholar] [CrossRef] [PubMed]
[5]. Morton AC, Siotia A, Arnold ND, Korgul P, Bowles J, Heppenstall J, Simultaneous kissing stent technique to treat left main stem bifurcation diseaseCatheter Cardiovasc Interv 2007 69(2):209-15.10.1002/ccd.2094417195202 [Google Scholar] [CrossRef] [PubMed]
[6]. Katayama T, Yamamoto F, Ishizaki M, Iwasaki Y, Very late bare metal stent thrombosis presenting with acute myocardial infarction: 14 years after coronary stentingInternal Medicine 2010 49(15):1549-52.10.2169/internalmedicine.49.333720686289 [Google Scholar] [CrossRef] [PubMed]
[7]. Katayama T, Yamamoto T, Iwasaki Y, A case report of very late thrombosis of coronary bare-metal stent 10 years after stentingInt Heart J 2007 48(4):547-52.10.1536/ihj.48.54717827826 [Google Scholar] [CrossRef] [PubMed]
[8]. Acibuca A, Gerede DM, Vurgun VK, Bare-metal stent thrombosis two decades after stentingCardiovasc J Afr 2015 26(4):e1910.5830/CVJA-2015-03426407330 [Google Scholar] [CrossRef] [PubMed]
[9]. Lau JK, Alcock RF, Brieger D, Lowe HC, Complex, diffuse in-stent atherosclerosis over a decade following bare metal stentingCoronary Artery Disease 2015 26:e69-70.10.1097/MCA.000000000000020526247273 [Google Scholar] [CrossRef] [PubMed]
[10]. Doyle B, Rihal CS, O’Sullivan CJ, Lennon RJ, Wiste HJ, Bell M, Outcomes of stent thrombosis and restenosis during extended follow-up of patients treated with bare-metal coronary stentsCirculation 2007 116(21):2391-98.Epub 2007/11/0710.1161/CIRCULATIONAHA.107.70733117984377 [Google Scholar] [CrossRef] [PubMed]