Atypical Presentation of an Adrenal Mass
Krishna Swathi Pavuluri1, N Senthil2, RB Sudagar Singh3, L Suja4
1 Postgraduate, Department of Internal Medicine, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
2 Professor, Department of Internal Medicine, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
3 Professor, Department of Internal Medicine, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
4 Associate Professor, Department of Internal Medicine, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Krishna Swathi Pavuluri, Sri Ramachandra Institute of Higher Education and Research, Opp. V7 Hotel, Porur, Chennai-600116, Tamil Nadu, India.
E-mail: swathipavuluri94@gmail.com
Catecholamine-secreting tumours arise from chromaffin cells of the adrenal medulla, and the sympathetic ganglia referred to as pheochromocytomas and catecholamine secreting paragangliomas, respectively. The incidence of pheochromocytoma is less. This was about a 38-years-old male patient that complained of burning sensation while micturition and right loin pain. On evaluation, he was found to have a right adrenal mass of size of 6 cm. The patient was found to have right ureteric caliculi and right Double J Stent (DJ) was done. Patient was advised for further evaluation but he was not willing at that point of time. Thus, pheochromocytoma has to be one of the differentials in a young person presenting with hypertension or with atypical presentation. Because pheochromocytoma is one of the correctable causes of hypertension and a person can have a near normal or average life span after surgery. This patient presented with urinary symptoms followed by typical features of cholelithiasis rather than symptoms of pheochromocytoma.
Cholecystitis, Cholelithiasis, 123I MIBG scintigraphy, Pheochromocytoma, Zellballen pattern
Case Report
In 2017, a 38-year-old male patient came with the complaints of burning micturition and right iliac region pain from past three days, pain was of pricking type with no renal angle or right iliac fossa tenderness. Ultrasonography (USG) abdomen showed right ureteric caliculi and right suprarenal mass of 6 cm. Soon after, Double J (DJ) stenting was done. Postprocedure vitals (blood pressure was 120/80 mmHg and pulse rate was 80 beats/min) were stable. Patient was planned for further evaluation of the right adrenal mass, but he was not willing for further management.
After one year, the patient visited again with complaint of right hypochondriac pain. At that time, the blood pressure was 150/90 mmHg. Computed Tomography (CT) of whole abdomen showed cholelithiasis and increased size of the right adrenal mass. A 24 hour urine metanephrines and Vanillylmandelic Acid (VMA) were 8.5 mg/24 hours and 1.2 mg/24 hours (normal range=1 mg/24 hours), respectively. The condition was diagnosed as pheochromocytoma. Later, the patient was started on antihypertensives (tab. amlodipine-atenelol 5 mg/50 mg OD) and planned for emergency laparoscopic cholecystectomy because of right hypochondriac pain and fever.
Surgery was done under general anaesthesia and agents used were sevoflurane 3%, fentanyl 100 mcg, propofol 80 mg and vecuronium 6 mg. Intraoperatively, the patient had a heart rate of 90 beats/min and blood pressure of 90/60 mmHg to 154/94 mmHg; so he was administered inj. esmolol of 30 mg and inj. phenylephrine of 20 mcg. The patient was given calcium channel blockers and beta blockers with alpha-blockers, as needed till the day of surgery. Intraoperatively, inflamed thickened gallbladder with 30 mL of pus was present. He withstood the procedure well without any complications during the surgery, and was advised to follow-up for the adrenal mass.
The patient presented after one year with the complaints of right hypochondriac pain, palpitations and shortness of breath since one week; blood pressure was 160/90 mmHg with rest of the examination being normal. Investigations showed fasting blood glucose 127 mg/dL, postprandial blood glucose 190 mg/dL, serum creatinine 1.0 mg/dL, serum calcium 9.1 mg/dL, Alkaline phosphatase (ALP) 202 IU/L, vitamin D 9.5 ng/mL, serum phosphorous 2.6 mg/dL, Thyroid Stimulating Hormone (TSH) 1.82 mIU/L and Parathyroid Hormone (PTH) was 91.6 pg/mL. Chest radiograph was normal.
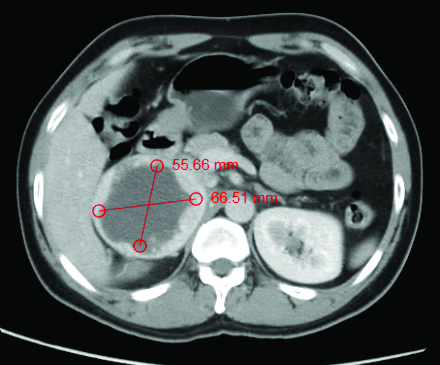
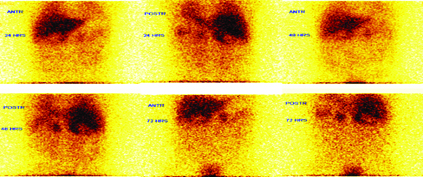
Electrocardiography (ECG) showed T-wave inversions in v4-v6, normal sinus rhythm and 2D-Echo showed concentric left ventricular hypertrophy with ejection fraction of 65%. USG abdomen showed thick-walled right complex supra renal cystic lesion of size 7.4×7.2 cm and increased vascularity in the lesion wall. A 24 hour urine metanephrines was 1.2 mg (up to 1), 24 hour urine normetanephrines 4890 mcg/24 hr (<600 mcg/24 hr) and normetanephrine creatinine ratio 4890 UG/G creatinine (86-236 UG/G creatinine). Contrast-Enhanced Computed Tomography (CECT) of whole abdomen showed a well-defined thick-walled mass with intense peripheral enhancement on arterial phase measuring 7×8.2×7.6 cm. It was seen replacing the right adrenal gland with mass effect on adjacent structures, i.e., Inferior Vena Cava (IVC) anteromedially, the upper pole of the right kidney inferiorly, liver superiorly and relatively well-maintained fat planes [Table/Fig-1]. The size was more than 6 cm and the radiographical diagnosis was malignant pheochromocytoma. 123I MIBG scan showed abnormal tracer uptake in both suprarenal regions with a large cold area in the right suprarenal region in the both 48 and 72 hours delayed static images [Table/Fig-2].
Axial view of the CECT abdomen showing right suprarenal mass.
I123-MIBG scan showed uptake with large cold area in the right suprarenal region at 48 and 72 hours.
The patient underwent laparoscopic right adrenalectomy in the different hospital. The histopathological examination showed large and irregular cell nests with a focal zellballen pattern with the absence of necrosis, nuclear atypia and mitosis (0-1/10 HPF), and no vascular and adrenal evidence capsular invasion. Histopathological examination confirmed right adrenal pheochromocytoma. Postprocedural follow-up after two months showed fasting blood glucose was 100 mg/dL, postprandial blood glucose was 120 mg/dL and blood pressure of 130/90 mmHg. He did not require antihypertensives since postoperative day one till date.
Discussion
Catecholamine secreting tumours are most common in 4th-5th decade of life effecting equally men and women. Mula-Abed WA et al., reported pheochromocytoma of size 7×8 cm in a 50-year-old female [1]. This patient presented with a tumour of size 7×8.2 cm at 38 years of age, without typical symptoms of pheochromocytoma.
Typical symptoms associated with pheochromocytoma are palpitations, tremors, headache and diaphoresis which may occur in spells and paroxysms [2,3]. Dolan RT et al., reported pheochromocytoma in a 45-year-old female presenting as recurrent urinary tract infections with Latent Autoimmune Diabetes Mellitus (LADA), but the index patient presented with urinary symptoms with Impaired Glucose Tolerance (IGT) [4]. Overproduction of catecholamines, as in pheochromocytoma, leads to resistance to insulin on peripheral tissues leading to impaired glucose tolerance [5]. But after surgery some patients revert to normal, as in the present case. Nerli RB et al., reported a 4 cm pheochromocytoma in a 37-year-old male patient presenting as right ureteric caliculi [6].
Clinical suspicion of pheochromocytoma is required for biochemical testing. It includes measurement of 24 hour catecholamines and metanephrines in both plasma and urine, but urine metanephrines have 98% sensitivity and specificity, while plasma metanephrines have sensitivity of 96% and the specificity of 85% and associated with highly false-positive rate with plasma metanephrine measurement [7]. First test for localisation of the tumours of abdomen and adrenals is CT or Magnetic Resonance Imaging (MRI) which have a sensitivity of >95% and specificity of >65% [8,9]. If abdominal imaging is negative, then I-123 MIBG scintigraphy is indicated and this procedure has a sensitivity of 80% and the specificity of 99% [9,10].
Surgery is the definitive treatment for pheochromocytoma. Malignant ones are biochemically and histologically similar to benign ones, as the only indication for presence of malignant tumours are local invasion into the surrounding tissues [11]. In case of bilateral adrenalectomy, glucocorticoids to be given if planned preoperatively. Autotransplantation of the adrenocortical tissue with complete bilateral adrenalectomy do not circumvent the need for lifelong glucocorticoid treatment [12].
Conclusion(s)
This article reported a case of large right adrenal pheochromocytoma confirmed clinically, biochemically and histologically; in a 38-year-old Indian male. Patient recovered completely after resection and there was no evidence of extra-adrenal spread. Annually 24 hour urine fractionated catecholamines and metanephrines must be checked for recurrence. The patient presented with a tumour size of 6 cm with ureteric caliculi at presentation and features of cholelithiasis rather than symptoms of pheochromocytoma.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 11, 2020
Manual Googling: Mar 15, 2021
iThenticate Software: Apr 24, 2021 (10%)
[1]. Mula-Abed WA, Ahmed R, Ramadhan FA, Al-Kindi MK, Al-Busaidi NB, Al-Muslahi HN, A Rare Case of Adrenal Pheochromocytoma with Unusual Clinical and Biochemical Presentation: A Case Report and Literature ReviewOman Med J 2015 30(5):382-90.10.5001/omj.2015.7626421121 [Google Scholar] [CrossRef] [PubMed]
[2]. Stein PP, Black HR, A simplified diagnostic approach to pheochromocytoma. A review of the literature and report of one institution’s experienceMedicine (Baltimore) 1991 70(1):46-66.10.1097/00005792-199101000-000041988766 [Google Scholar] [CrossRef] [PubMed]
[3]. Bravo EL, Pheochromocytoma: New concepts and future trendsKidney Int 1991 40(3):544-56.10.1038/ki.1991.2441787652 [Google Scholar] [CrossRef] [PubMed]
[4]. Dolan RT, Butler JS, McEntee GP, Bryne MM, Pheochromocytoma presenting as recurrent urinary tract infections: A case reportJ Med Case Report 2011 5(6):01-08.10.1186/1752-1947-5-621226896 [Google Scholar] [CrossRef] [PubMed]
[5]. Murao K, Imachi H, Sato M, Dobashi H, Tahara R, Haba R, A case of pheochromocytoma complicated with slowly progressive type 1 diabetes mellitus and chronic thyroiditisEndocrine 2007 32(3):350-53.10.1007/s12020-008-9049-y18256939 [Google Scholar] [CrossRef] [PubMed]
[6]. Nerli RB, Patil RA, Patne P, Suresh SN, Hiremath MB, Unusual presentation of pheochromocytomaJ Sci Soc 2014 41:136-39.10.4103/0974-5009.132866 [Google Scholar] [CrossRef]
[7]. Kudva YC, Sawka AM, Young WF Jr, Clinical review 164: The laboratory diagnosis of adrenal pheochromocytoma-the Mayo clinic experienceJ Clin Endocrinol Metab 2003 88:4533-39.10.1210/jc.2003-03072014557417 [Google Scholar] [CrossRef] [PubMed]
[8]. Wiseman GA, Pacak K, O’ Dorisio MS, Neumann DR, Waxman AD, Mankoff DA, Usefulness of 123I-MIBG Scintigraphy in the evaluation of patients with known or suspected primary or metastatic Pheochromocytoma or Paraganglioma: Results from a prospective multicentre trialJ Nucl Med 2009 50:1448-54.10.2967/jnumed.108.05870119690028 [Google Scholar] [CrossRef] [PubMed]
[9]. Brink I, Hoegerle S, Klisch J, Bley TA, Imaging of pheochromocytoma and paragangliomaFam Cancer 2005 4:61-68.10.1007/s10689-004-2155-y15883712 [Google Scholar] [CrossRef] [PubMed]
[10]. Havekes B, King K, Lai EW, Romjin JA, Corssmit EP, Pacak K, New imaging approaches to pheochromocytomas and paragangliomasClin Endocrinol (Oxf) 2010 72:137-45.10.1111/j.1365-2265.2009.03648.x19508681 [Google Scholar] [CrossRef] [PubMed]
[11]. Amar L, Servais A, Gimeniz-Roqueplo AP, Zinzindohoue F, Chatellier G, Pierre-François P, Year of diagnosis, features at presentation, and risk of recurrence in patients with Pheochromocytoma or secreting ParagangliomaJ Clin Endocrinol Metab 2005 90:2110-16.10.1210/jc.2004-139815644401 [Google Scholar] [CrossRef] [PubMed]
[12]. Okamoto T, Obara T, Ito Y, Yamashita T, Kanbe M, Iihara M, Bilateral adrenalectomy with autotransplantation of adrenocortical tissue or unilateral adrenalectomy: Treatment options for pheochromocytomas in multiple endocrine neoplasia type 2AEndocrine Journal 1996 43(2):169-75.10.1507/endocrj.43.1698793332 [Google Scholar] [CrossRef] [PubMed]