Reversal of Pulmonary Hypertension in a Patient with Chronic Mountain Sickness after Relocation to Low Altitude
Abdirashit Maripov1, Kubatbek Muratali Uulu2, Samatbek Satybaldyev3, Nadira Kushubakova4, Akpay Sarybaev5
1 Senior Scientist and Head, Department of Mountain and Sleep Medicine and Pulmonary Hypertension, National Center of Cardiology and Internal Medicine, Bishkek, Kyrgyzstan.
2 Junior Scientist, Department of Mountain and Sleep Medicine and Pulmonary Hypertension, National Center of Cardiology and Internal Medicine, Bishkek, Kyrgyzstan.
3 Junior Scientist, Department of Mountain and Sleep Medicine and Pulmonary Hypertension, National Center of Cardiology and Internal Medicine, Bishkek, Kyrgyzstan.
4 Junior Scientist, Department of Mountain and Sleep Medicine and Pulmonary Hypertension, National Center of Cardiology and Internal Medicine, Bishkek, Kyrgyzstan.
5 Professor and Director, Department of Mountain and Sleep Medicine and Pulmonary Hypertension, National Center of Cardiology and Internal Medicine, Bishkek, Kyrgyzstan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Akpay Sarybaev, T. Moldo Street 3, Bishkek, Kyrgyzstan.
E-mail: ak_sar777@mail.ru
Long-term high altitude residence can be complicated by development of Chronic Mountain Sickness (CMS) characterised by excessive erythrocytosis and neurological symptoms. In some patients, CMS may be associated with various degrees of Pulmonary Hypertension (PH). There have been no reports on changes in the pulmonary circulation and Right Ventricular (RV) structure following translocation to low altitude of patients with CMS. Here, the authors report a case of 56-years-old female patient, resident of Sary-Mogol (3,000 m, Kyrgyzstan), diagnosed of CMS on clinical and laboratory examination. Transthoracic echocardiography revealed slightly dilated right ventricle and significantly enlarged pulmonary artery diameter was found. The patient undergone complete resolution of symptoms and alleviation of PH within three years of residence at low altitude. Thus, relocation to low altitude cures CMS and reverses PH.
Erythrocytosis, High altitude, Neurological symptoms, Pulmonary circulation
Case Report
A 56-year-old female resident of Sary-Mogol (3,000 m, Kyrgyzstan) presented with complaints of frequent headache, daytime sleepiness, paresthesia, easy fatigability and dyspnoea on mild exertion during the author’s field expedition to this area. The patient was born in Osh, Kyrgyzstan located at 960 m. At age 23, she got married and moved to Shaimak (4,000 m, Tajikistan), where she lived for 19 years and then moved to Sary-Mogol.
Laboratory examination showed haemoglobin concentration of 197 g/L, red blood cell count of 6.88×1012/L and haematocrit 64%. The CMS Qinghai questionnaire score was 16. Transthoracic echocardiography revealed a slightly dilated Right Ventricle (RV). The pulmonary artery was significantly dilated with a diameter of 4.36 cm [Table/Fig-1a]. Tricuspid regurgitation signal was not detectable in this patient. Pulmonary artery acceleration time was measured at 90 msec with estimated mean pulmonary artery pressure of 34 mmHg [Table/Fig-1b]. A Right Ventricular (RV) systolic function was preserved with RV fractional area change of 46.2% and peak systolic velocity at the lateral tricuspid annulus of 24.7 cm/sec. The ratio of early tricuspid inflow to annular diastolic velocity E/Ea, as a non-invasive estimation of RV filling pressure, was increased at 6.2. The patient was diagnosed as having a severe form of CMS with high altitude PH and relocation to low altitude was recommended.
Transthoracic Echocardiogram. a) Pulmonary artery diameter in the parasternal short-axis of pulmonary bifurcation view at first presentation; b) Pulmonary artery flow velocity profile in the main pulmonary artery and measurement of pulmonary artery acceleration time in the parasternal short-axis view at first presentation; c) Pulmonary artery diameter during follow-up; d) Pulmonary artery flow velocity profile and measurement of pulmonary artery acceleration time during follow-up.
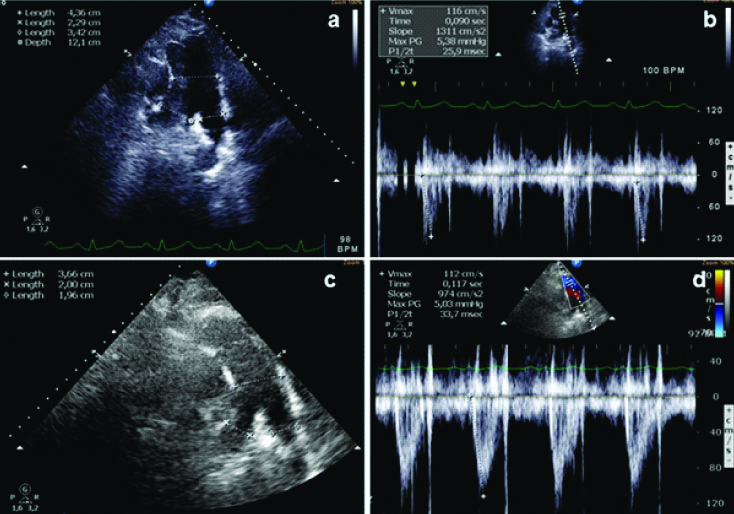
The patient followed the recommendation and moved to Osh. Three years later, the patient reported complete resolution of the symptoms. Blood cell count showed normalisation of all the parameters: haemoglobin 152 g/L, erythrocytes 4.92×1012/L and haematocrit 46%. Repeat echocardiography did not reveal any changes in the RV chamber dimensions. However, the diameter of the pulmonary artery was significantly decreased to 3.65 cm [Table/Fig-1c]. The pulmonary artery acceleration time was increased and measured at 117 msec [Table/Fig-1d]. Estimated mean pulmonary artery pressure was 18 mmHg. The RV systolic function was maintained and the ratio of early tricuspid inflow to annular diastolic velocity E/Ea, decreased to 3.7.
Discussion
Long-term high altitude residence leads to development of PH of mild to moderate degrees. In addition, high altitude residence can be complicated by development of excessive erythrocytosis and CMS. In some patients, CMS may be associated with various degrees of PH [1]. In some individuals, PH is severe leading to RV dysfunction [2]. RV dysfunction in highlanders is associated with greater morbidity and mortality [3]. Although, no evidence of resting RV dysfunction in CMS patients with PH and RV dilatation has been found in recent studies [4,5], an exaggerated PH during mild exercise associated with daily activity has been suggested as an underlying cause of morbidity and mortality in these patients [6].
Given the important role of hypoxia in the pathogenesis of CMS and high altitude PH, it is believed that relocation of the place of residence to lower altitudes would cure the disease. In this regard, reduction of haemoglobin levels has been observed in temporary high altitude residents with excessive erythrocytosis after six months of de-induction [7]. Similarly, resolution of symptoms within 1-21 months of return to low altitude has been reported in 99 out of 102 temporary residents with high altitude PH. In two men, however, PH persisted, one of them continued to deteriorate, and died [8]. Sustained PH at lowland in some highlanders suggests that long-term high altitude residence may induce irreversible vascular remodeling. Although, resolution of mild PH has been shown in healthy high altitude dwellers after two years of residence at sea level [9,10], it remains unknown, if migration to lowland regions leads to reversal of PH in patients with CMS.
Conclusion(s)
This reports a case of complete resolution of symptoms and alleviation of PH in a patient with CMS within three years of residence at low altitude. As this case illustrates, relocation to lowland not only cures CMS but also reverses PH, atleast in some patients, thus representing a very effective approach in managing this condition.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Dec 31, 2021
Manual Googling: Feb 10, 2021
iThenticate Software: Apr 20, 2021 (18%)
[1]. Leon-Velarde F, Maggiorini M, Reeves JT, Aldashev A, Asmus I, Bernardi L, Consensus statement on chronic and subacute high altitude diseasesHigh Alt Med Biol 2005 6(2):147-57.10.1089/ham.2005.6.14716060849 [Google Scholar] [CrossRef] [PubMed]
[2]. Maripov A, Mamazhakypov A, Karagulova G, Sydykov A, Sarybaev A, High altitude pulmonary hypertension with severe right ventricular dysfunctionInt J Cardiol 2013 168(3):e89-90.10.1016/j.ijcard.2013.07.12923911270 [Google Scholar] [CrossRef] [PubMed]
[3]. Penaloza D, Arias-Stella J, The heart and pulmonary circulation at high altitudes: Healthy highlanders and chronic mountain sicknessCirculation 2007 115(9):1132-46.10.1161/CIRCULATIONAHA.106.62454417339571 [Google Scholar] [CrossRef] [PubMed]
[4]. Maignan M, Rivera-Ch M, Privat C, Leon-Velarde F, Richalet JP, Pham I, Pulmonary pressure and cardiac function in chronic mountain sickness patientsChest 2009 135(2):499-504.10.1378/chest.08-109418719057 [Google Scholar] [CrossRef] [PubMed]
[5]. Huez S, Faoro V, Guenard H, Martinot JB, Naeije R, Echocardiographic and tissue Doppler imaging of cardiac adaptation to high altitude in native highlanders versus acclimatized lowlandersAm J Cardiol 2009 103(11):1605-09.10.1016/j.amjcard.2009.02.00619463523 [Google Scholar] [CrossRef] [PubMed]
[6]. Stuber T, Sartori C, Schwab M, Jayet PY, Rimoldi SF, Garcin S, Exaggerated pulmonary hypertension during mild exercise in chronic mountain sicknessChest 2010 137(2):388-92.10.1378/chest.09-135519783668 [Google Scholar] [CrossRef] [PubMed]
[7]. Liu C, Liu B, Zhang EL, Liao WT, Liu J, Sun BD, Elevated pentose phosphate pathway is involved in the recovery of hypoxiainduced erythrocytosisMol Med Rep 2017 16(6):9441-48.10.3892/mmr.2017.780129039604 [Google Scholar] [CrossRef] [PubMed]
[8]. Singh I, Khanna PK, Lal M, Hoon RS, Rao BD, High-altitude pulmonary hypertensionLancet 1965 1(7404):146-50.10.1016/S0140-6736(65)90229-1 [Google Scholar] [CrossRef]
[9]. Grover RF, Vogel JH, Voigt GC, Blount SG Jr, Reversal of high altitude pulmonary hypertensionAm J Cardiol 1966 18(6):928-32.10.1016/0002-9149(66)90443-7 [Google Scholar] [CrossRef]
[10]. Sime F, Penaloza D, Ruiz L, Bradycardia, increased cardiac output, and reversal of pulmonary hypertension in altitude natives living at sea levelBr Heart J 1971 33(5):647-57.10.1136/hrt.33.5.6475115010 [Google Scholar] [CrossRef] [PubMed]