As in any other growing economic nation, nearly 48-65% of chronic kidney disease patients in India present in very late stages to the nephrologist with uraemia [1,2]. These patients require urgent haemodialysis; a temporary (non-tunneled) catheter is often used till stabilisation [3]. Cather Related Blood Stream Infection (CRBSI) often sets in within a week or two leading to catheter discontinuation [4]. Further, there is requirement of parenteral antibiotics, repeated hospitalisation and catheter reinsertions escalating the cost of continued treatment [5].
The TCC for haemodialysis serves as an useful bridge through which patient can be initiated on maintenance dialysis. Due to increased catheter longevity, less CRBSI it can be continued till AVF matures or patient opts for alternative form of Renal Replacement Therapy (RRT) [6].
With a small learning curve, many nephrologists are inserting TCC for the needy patients; one of the barriers being need for fluoroscopic guidance which is not available freely when required. Often, fluoroscopy is a shared facility which is difficult to access when most needed by nephrologist [7-9].
Thus, the present prospective study was done with tunneled cuffed haemodialysis catheter insertions using ultrasound guidance alone, looking at insertion complications, infections, bleeding complications, catheter flow rates and catheter longevity.
Materials and Methods
The prospective observational study was conducted at St. John’s Medical College Hospital (SJMCH), Bengaluru, Karnataka, India. A total of 102 patients underwent TCC insertion during the study period from July 2017 to December 2018. A total of 106 procedures were performed as four patients required catheter removal and reinsertion within two weeks. Patients were further followed-up till September 2019 (nine months after the last catheter insertion). The study was approved by Institutional Ethics Committee for research project analysis and publication. All procedures were performed by a senior nephrology consultant and a trainee in the nephrology interventional suite. Fluoroscopy was used in none. Informed consent was obtained from all the patients prior to the procedure.
Inclusion criteria: Patients requiring long term haemodialysis without a prior AVF, awaiting transplant in the near future, acute kidney injury with prolonged recovery time were considered for tunneled catheters and underwent the procedure after signing a written informed consent form.
Exclusion criteria: All patients underwent a bedside ultrasound screening of bilateral Internal Jugular Vein (IJV) and femoral veins. Those with bilateral IJV thrombosis and/or significant anatomical variation were excluded.
Procedures were carried out on an in-patient basis after obtaining basic laboratory work up including haemoglobin and coagulation profile. Patients received prophylactic, intravenous antibiotic- amikacin 500 mg half an hour prior to the procedure and premedications included intravenous tramadol 50 mg and ondansetron 4 mg. Preprocedural sedation was given with short acting benzodiazepine (1 mg IV midazolam), which was used just prior to tunneling procedure and local anaesthesia 2% lignocaine was infiltrated along the path of tunneling. Around 10-15 mL of 2% lignocaine for achieving good local anaesthetic effect along the tunneling path was used. All patients’ Blood Pressure (BP), Oxygen Saturation (SPO2), pulse rate were monitored throughout the procedure. A 14.5 French × 28 cm “Haemoflow” (Medcomp) double lumen catheter with a cuff to tip length of 23 cm and Covidien Chronic Silicone Permacatheter (Medtronic) were used. Eight French catheter with 15 cm cuff to tip length was used in a paediatric patient.
Right IJV was the preferred choice followed by left IJV and femoral veins when the former couldn’t be cannulated due to thrombosis. Under due aseptic precautions, using ultrasound and anatomical landmarks IJV was identified and cannulated as close as possible to the clavicle (“low puncture”).
The catheter was then placed in a loop configuration with the tip placed slightly below the sternal angle and exit site marked on ipsilateral chest wall avoiding axilla/breast tissue. This was followed by lignocaine infiltration, blunt dissection and tunneling directed towards the Internal Jugular Catheter (IJC) puncture site. After the catheter was brought out close to the IJC puncture site, serial dilatation of the vein followed by introduction of trocar and peel away sheath was done. Trocar and guidewire were then removed and the free end of the catheter was introduced through the sheath. Subsequently, sheath was peeled away while holding the catheter in place. Flow was checked in both limbs of the catheter followed by instillation of heparin lock -1 mL of 5000 units heparin diluted with 4 mL normal saline and 1.8 mL was instilled in each limb.
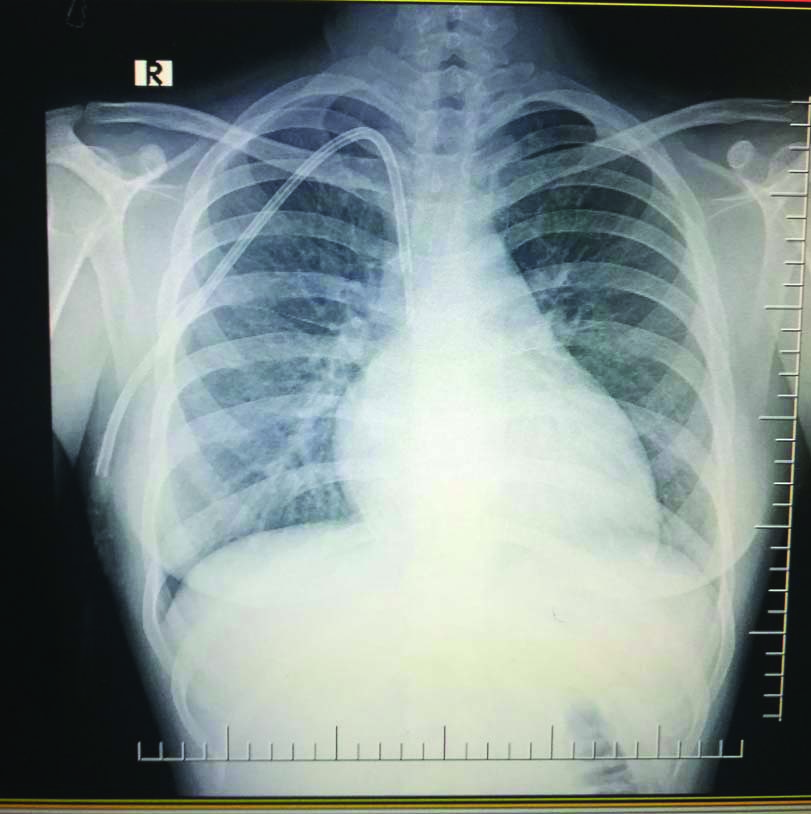
After achieving haemostasis and securing the catheter, sterile dressing was applied. Chest X-ray to confirm tip position [Table/Fig-1] was performed in all patients prior to initiation of haemodialysis. Catheters were handled by dialysis technicians and staff with sterile precautions. Catheter insertion complications like pneumothorax, haemothorax, pericatheter bleed, if any were noted. Subsequently follow-up data regarding catheter flow rates, incidence of CRBSI, catheter longevity were noted.
Chest X-ray depicting TCC and position of catheter tip at junction of Superior Vena Cava (SVC) and right atrium.
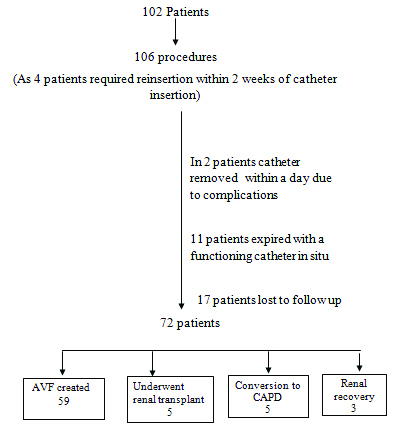
Data collection and follow-up: Initial data was collected by chart review. Seventy two patients were available for further follow-up till September 2019, which was 9 months after the last catheter insertion [Table/Fig-2]. Follow-up data were collected by direct patient interview on Out Patient Department/Haemodialysis unit visit for in-center patients (Cohort A) and by telephonic interview of patients who underwent dialysis at other centers (Cohort B).
Flowchart showing catheter outcome data of 102 patients.
Statistical Analysis
Data was recorded in the predesigned Epi info version 7.0 proforma and analysed by Statistical Package for the Social Sciences (SPSS) software version 24.0.
Results
In the present study, a total of 102 patients (Male 67; Female 35) between the age group of 11 to 77 years (Mean 50.29 years) underwent TCC insertion between July 2017 and December 2018.
Patient characteristics are depicted in [Table/Fig-3].
Patient characteristics of the study group; Cohort A: Patients who underwent maintenance dialysis at SJMCH; Cohort B: Patients who underwent dialysis at any other centers.
| Variables | Whole cohort N=102 | Cohort A N=62 | Cohort B N=40 |
|---|
| Age (mean) in years | 50.29 | 48.8 | 53.05 |
| Male:Female | 67:35 | 44:18 | 23:17 |
| Median catheter days | 89 | 90 | 85.5 |
| Aetiology of renal failure |
| Diabetic nephropathy | 45 | 26 | 19 |
| Glomerulopathy | 26 | 18 | 8 |
| Hypertension | 5 | 2 | 3 |
| Obstructive/reflux uropathy | 3 | 2 | 1 |
| Interstitial disease | 15 | 9 | 6 |
| Loss of graft | 1 | 1 | 0 |
| Prolonged Acute Kidney Injury (AKI) | 5 | 2 | 3 |
| Other | 2 | 2 | 0 |
| Indication for tunneled catheter insertion |
| HD initiation (bridge to AVF) | 88 | 56 | 32 |
| Arteriovenous Fistula (AVF) failure | 4 | 2 | 2 |
| Planned early transplant | 2 | 1 | 1 |
| Acute Kidney Injury (AKI) prolonged | 5 | 3 | 2 |
| TCC insertion with “new venipuncture” | 95 | 58 | 37 |
| Conversion of existing temporary catheter to tunneled catheter | 7 | 4 | 3 |
| Site of insertion |
| Right Internal Jugular Vein (IJV) | 96 | 60 | 36 |
| Left IJV | 5 | 1 | 4 |
| Femoral | 1 | 1 | 0 |
The most common cause of Chronic Kidney Disease (CKD)-Stage V was diabetic nephropathy in 45 patients (44.1%) and the most common indication for catheter insertion was initiation of HD in the absence of permanent vascular access (86.27%).
Right IJV was the preferred site in 96 subjects (94.1%) and left jugular vein/ femoral veins were considered only if right-side was thrombosed or noted to have a significant anatomical variation.
A total of 95 (93.1%) patients underwent the procedure with “new venipuncture” being done during the procedure as the uncuffed catheters were placed higher (>3 cm vertically from the clavicle) posing risk of kinking. Three patients had no prior cannulation and underwent TCC insertion as the primary procedure for initiation of haemodialysis.
Patients were followed-up till September 2019 (9 months after the last catheter insertion) and events recorded. A total of 11386 catheter days were evaluated for catheter outcomes. On an average each patient had a tunneled catheter in-situ for about three months (median 89 days). One patient with difficult vascular access had a functioning TCC for 565 days which was the maximum duration noted in this study.
Complications
1. Acute complications
Two catheters were removed within a day. One due to malposition (venous laceration during attempted left IJV cannulation) and other due to persistent tunnel ooze in a patient who had recently undergone Percutaneous Transluminal Coronary Angioplasty (PTCA) and was on dual antiplatelets. As per the standard of care in nephrology, patients who are on dual antiplatelets and recent PTCA with stent (within one year), antiplatelets cannot be stopped due to risk of stent thrombosis and hence these patients were not excluded for minor vascular procedures like catheter insertions and AV fistula surgeries. However, the small risk of bleed was duly explained to the patients and informed consent was obtained.
Minor anaesthetic complications (sedation, agitation) were noted in 3.9% (4 patients) and tunnel haematoma was noted in 2.9% (3 patients), all managed conservatively. Other complications mentioned in other series like pneumothorax, haemothorax, shearing of vein, haemopericardium were not observed.
2. Chronic complications
a. Infections: Incidence of CRBSI was 1.65 per 1000 catheter days. Nine of the 62 patients (14.5%) who were on dialysis at the center (cohort A) had an episode of CRBSI. The incidence of CRBSI was higher in patients (cohort B) continuing Outstation dialysis (10 patients accounting for 25% CRBSI) presumably due to lack of technician expertise in handling TCC at smaller centers. Three patients had more than one episode of CRBSI.
Majority could be managed with systemic antibiotics, use of antibiotic lock therapy and catheter salvaged. In four out of the 22 episodes, catheter had to be removed. There was no mortality due to CRBSI.
b. Patency of the catheter: Immediately post insertion, adequate blood flow (mean blood flow 230.3 mL/min) was achieved in all except a catheter placed in the left IJC (kinking at the entry site, average blood flow 180 mL/min).
During the further course, four patients presented with poor flow due to luminal thrombosis and catheters were salvaged by local instillation of streptokinase. No catheters were removed due to poor flow.
3. Unusual complications
An elderly woman with the catheter in-situ for over a year, breach in the integrity of subcutaneous tunnel with necrosis of the overlying skin was noted [Table/Fig-4]. She had no overt signs of tunnel infection. As a significant part of the catheter was exposed, it was removed immediately.
Exposed Catheter Tunnel due to pressure necrosis of overlying skin.

Catheter outcomes: Seventy-two patients were followed-up till September 2019 and catheter outcomes were recorded, as presented in [Table/Fig-5].
Catheter outcomes of patients on follow-up.
| Catheter outcome | Number of patients |
|---|
| AVF created | 59 |
| Underwent renal transplant | 5 |
| Method conversion to CAPD | 5 |
| Renal recovery | 3 |
| Death with functioning catheter | 11 |
AVF: Arteriovenous fistula; CAPD: Continuous ambulatory peritoneal dialysis
TCC served as a haemodialysis access till AVF creation in 59 patients. Five of the 72 patients chose CAPD as long term dialysis modality and another five underwent renal transplantation with TCC acting as a useful bridge for the definitive long term RRT.
Exit site bleed was seen in four of the 102 TCC catheter insertions in the present study. Only one patient who was on dual antiplatelets required immediate catheter removal and the other 3 managed conservatively. Four TCC had intraluminal thrombus and the catheters could be salvaged by intraluminal thrombolytic therapy as mentioned in [Table/Fig-6].
| Complications | Number of subjects |
|---|
| Exit site bleed | 4 |
| Catheter kink | 1 |
| Cuff extrusion | 0 |
| Intraluminal thrombus | 4 |
| Initial successful thrombolysis | 4 |
| Catheter removal and/or replacement | 4 |
Discussion
The TCCs are increasingly in vogue because of an early and sustainable vascular access coupled with lack of major haemodynamic compromise. In India, nearly half of the CKD patients present directly in late stages of CKD and have many barriers to AV creation [1]. The delayed processing time from referral to access creation, lack of acceptance and delay and/or failure of fistula maturation pose additional challenges [10]. Therefore, most patients require a “bridge” between initiation of HD and AVF creation. Temporary uncuffed catheters are associated with a high risk of infections even when used for shorter durations as less as two weeks [4]. Therefore, it is important to accept TCC as a “necessary evil” in the present scenario [11].
Despite the above advantages, TCC use is not widespread because of the non availability of fluoroscopy and lack of training of new growing nephrologists with the insertion technique [12]. Earlier this has been an area handled by interventional radiologists, vascular surgeons or general surgeons done in the operation theatres [13].
Two earlier series of Indian data- one from Madurai medical college by Sampathkumar K et al., and the second from KEM hospital, Pune reported insertion practices of TCCs by nephrologists [8,14]. [Table/Fig-7] shows the comparison of complications noted in the present study with that of the study conducted by Madurai medical college and KEM hospital, Pune [8,14]. The procedure was undertaken in nephrology intervention/cardiac catheterisation suite or a fluoroscopy equipped operation theater. The study by Sampathkumar K et al., assessed fluoroscopy guidance requirement, as 8% of the total procedures [8]. However, most centers are not equipped with fluoroscopic facilities and there have been earlier studies comparing safety and complications of fluoroscopy versus modified traditional approach using ultrasound guidance alone [15,16].
Comparison of complications with earlier published Indian data.
| Complications | Sampathkumar K et al., [8] n=100) | Sampathkumar K et al., [14] (n=133) | Present study-SJMCH Bangalore (n=102) |
|---|
| Early complications |
| Exit site bleed | 8 | - | 4 |
| Catheter kink | 2 | 5 | 1 |
| Late complications |
| Cuff extrusion | 2 | 3 | 0 |
| Intraluminal thrombus | 3 | 11 | 4 |
| Initial successful thrombolysis | 2 | 8 | 4 |
| Catheter removal and/or replacement | 3 | 3 | 4 |
| Central vein thrombosis | No data | 4 | Not studied |
| Successful systemic thrombolysis | No data | 3 | Not attempted |
| Malfunction due to fibrin sheath | No data | 5 | 0 |
| Successful changes over a guidewire | No data | 4 | Not attempted |
All 102 procedures in the present study were carried out under ultrasound guidance without fluoroscopy. The rate of complications were no different from that noted in earlier studies [8,14]. [Table/Fig-7] provides a comparative analysis of complications. The complication rates in our study are at par with earlier published data [14].
Of the total 102 TCC insertions, only a single patient had catheter kink, four had intraluminal thrombosis which was successfully thrombolysed using streptokinase.
In the present study, there was 100% success rate for uncomplicated insertions of right-sided jugular TCC using only ultrasound. Similar results with non-fluoroscopic technique have been earlier demonstrated by Motta Elias R et al., [16].
The average blood flow was adequate (230 mL/min) for most catheters except one. In our study, CRBSI rate was 1.65 per 1000 catheter days. Majority of the catheters could be salvaged with systemic antibiotics along with catheter antibiotic lock. Complications mentioned in other series like pneumothorax, haemothorax, shearing of vein, haemopericardium were not observed. One peculiar complication observed was necrosis of the skin overlying the catheter tunnel and if this happens the catheter needs to be removed. A similar albeit less severe scenario was reported by Borisov BK and Linkova SP [17]. They used rotating skin flap to cover the naked catheter.
The most common reason for unplanned catheter removal in this study was catheter related sepsis (failed salvage by antibiotics) which was seen in 4 patients. TCC in the present study was a useful bridge to AV fistula in 59 patients, 5 underwent renal transplant and another 5 opted for peritoneal dialysis as long-term RRT.
The overall data clearly favours using cuffed tunneled catheters as the first vascular access over temporary catheters whenever reasonably longer need for haemodialysis catheter is anticipated.
Limitation(s)
This was a single centre study, observational in nature with a small sample size. Randomised controlled trials with a comparative arm looking at catheter outcomes and haemodialysis adequacy studies and follow-up for central venous stenosis could throw more light regarding use of TCC.
Conclusion(s)
It was concluded that TCCs for haemodialysis initiation can be safely placed by using ultrasound guidance. It can be used for longer period and is a useful bridge to AV fistula. There was 100% success rate for right-sided jugular TCC insertions using ultrasound alone. There were very less infective and bleeding complications with TCC usage highlighting its usefulness in haemodialysis patients.