Chronic Kidney Disease is a global health problem in developing countries like India because of the expensive and life-long treatment and a major cause of morbidity and mortality in these countries hence the early diagnosis and treatment must be started in these patients and find out the co-morbidities. Worldwide more than 1 million people are alive on dialysis or with a functioning graft [1], But in a country like India, most of the population belong to rural areas and hence not able to afford the cost of renal transplant so that lifelong dialysis is commonly adopted the option of therapy by CVC [2] or later on by Arterio-Venous (AV) fistula. Dialysis catheters are commonly inserted in the IJV and femoral vein and these are associated with several complications including mechanical, thrombotic and infectious [2]. Infection and thrombosis are a matter of worry for a treating physician as these are associated with significant morbidity and mortality and also increase patient hospital stay and cost of treatment [2]. There are various studies that favours the formation of thrombosis and associated infection in patients with malignancies (solid tumours, or in haematological malignancy) [2,3].
Since CVC-Related Thrombosis (CVCRT) and CVC-Related Infections (CVCRI) cannot be seen as separate entities, and multiple factors contribute to thrombus formation. Biocompatibility of CVCs catheter [2], vessel damage because of a mechanical injury of vascular endothelium, irritation of the vessel wall by hyperosmolar drugs [3-5], catheter tip position [6-8], side and puncture site of insertion as the left-sided placement and in the subclavian vein was found to be associated with increased risk for CVCRT compared with the right side and in the IJV, which may cause vein compression and kinking of the CVC [7,8]. Platelates abnormalities and CVCRI is also a factor as CVCRT risk is high in patients with a CVCRI compared with those without infection [9,10].
The incidence of thrombosis was maximum in femoral catheter 21.5% and more chance of thrombus formation was noticed in catheters used for HD [9]. The incidence of asymptomatic CVCRT was found 1.5-34.1% [11,12] and symptomatic was 1.2-13.0% [9,13] in haematological malignancy and out of them two-third are clinically silent but it is observed that the risk of symptomatic thrombus formation was seven-fold high in these patients as compared to negative Doppler ultrasonographic findings [14,15]. The symptomatic patients complain of pain and swelling in the neck, arm, headache, abnormal sensation, erythema, venous distension, jaw pain in the ipsilateral side and the average time of complaint is approximately after 2 weeks [3,16-20]. Hence, this study aimed to determine the incidence of thrombosis associated with CVC inserted in IJV only and used for HD in CKD patients and the extent of thrombosis, and associated risk factors and outcomes of the patients admitted in ICU.
Materials and Methods
This prospective observational study was conducted in an ICU at Pacific Institute of Medical Sciences, Girwa, Udaipur, Rajasthan, India, from March 2017 to March 2018. The study included the CKD patients received in the Emergency and Outpatient Department (OPD) after obtaining the Ethics Committee Approval from Institutional Ethical Committee {No. IEC/PIMS/2017/56(A)} and taking informed written consent from the patient relative or appropriate person.
Inclusion criteria: Those OPD patients who required ICU admission and fulfiled the criteria for diagnose CKD. If patients had Shortness Of Breath (SOB) because of suspected pulmonary oedema, bilateral crepitations on auscultation, generalised or bilateral pedal oedema, history of chronic hypertension, anuria, Generalised Weakness (GW), and Arterial Blood Gas (ABG) analysis in favour of metabolic acidosis were included [1]. Laboratory investigations including, CBC showing low haemoglobin (usually <7 gm/dL), high blood urea, and serum creatinine (>200 mg/dL and >10 mg/dL, respectively), USG [14,15] finding in favour of Renal Medical Disease (RMD) [1] and require HD in opinion of nephrologist were included in the study.
Exclusion criteria: Patients who required HD at OPD basis, or those whose catheter was inserted in the femoral and subclavian vein and the patients who faced insertion attempts more than two in IJV, cases using AV fistula and pump catheter for dialysis and patients who require HD for Acute Renal Failure (ARF) were excluded from the study.
Procedure
After admission in ICU, an ABG analysis was performed and simultaneously multi-para monitor were attached including ECG, NIBP, SpO2, and a small 20 G intra-venous cannula was secured and after initial resuscitation and stabilisation, the procedure explained to the patient, and triple lumen HD curved catheter of 16 cm long, 12 Fr, 18 G of haemocent was chosen for insertion in the IJV.
The catheter was inserted by an experienced anaesthesiologist and intensivist within a maximum of two attempts with all aseptic precaution by a blind technique using external anatomical landmark and all three lines were flushed with a heparinised saline solution and then X-ray chest was recommended in each patient before starting dialysis to confirm the right position of the catheter at the junction of SVC and right atrium.
All these patients required HD usually two times within a week. Then after two weeks of catheter insertion, the patient sent for USG Neck to see the presence and size, and extent of thrombus in IJV, and simultaneously, the sign of inflammation was noted in every patient. The radiologist performed duplex colour Doppler USG to find out thrombus.
The data regarding demographics of the patient (age, gender, and weight), co-morbidities {Hypertension (HTN), Diabetes Mellitus (DM), Ischemic Heart Diease (IHD), Cardiovascular Accident (CVA), and others if any}, primary complaints (Anuria, GW, SOB), laboratory investigation (haemoglobin, blood urea, serum creatinine, USG abdomen), cause of CKD (i.e., renal or postrenal), those on chronic medication {Oral Hypoglycaemic Agents (OHA), antihypertensive, anticoagulant, antiplatelet}, the presence of thrombus and size of the thrombus, required vasopressor and ventilator support, outcome of patients post-treatment were recorded.
Statistical Analysis
All these parameters were noted on a Microsoft excel sheet and results were prepared after analysis in Statistical Package for the Social Sciences (SPSS) version 12.0 was used. T-test used for p-value calculation.
Results
Out of total 100 patients included in the study, 63 were males and 37 were females, males to females ratio was 1.7:1, and the most commonly affected age group was between 41-60 years followed by 61-80 years, the average weight for male was 64.66 kg and 53.33 kg for female patients [Table/Fig-1]. Thrombus formation is a common problem in patients who require frequent HD and there are various risk factors and co-morbidities which may contribute in Early Catheter-Related Thrombus formation (ECRT).
Showing demographic characters of CKD patients.
| Age group (years) | Total patients | Males | Females | Average weight (kg) |
|---|
| Males | Females |
|---|
| 20-40 | 21 | 12 | 9 | 66.83 | 41.11 |
| 41-60 | 45 | 33 | 12 | 72.43 | 42.24 |
| 61-80 | 34 | 18 | 16 | 56.12 | 80.24 |
| Total | 100 | 63 | 37 | 64.66 | 53.33 |
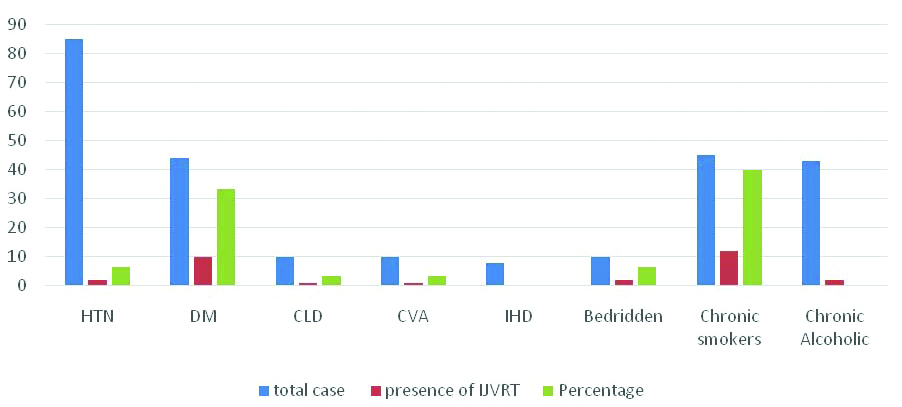
[Table/Fig-2] showed associated comorbidities and risk factors that may be contributing to ECRT in CKD patients. In co-morbidities, males more commonly suffered from HTN in 57 (90.47%), followed by type 2 Diabetes Mellitus in 32 (50.79%), Chronic Lung Disease (CLD) in 10 (15.87%), CVA in 8 (12.69%), IHD in 6 (9.52%) when compared to females. In females, HTN was diagnosed in 28 (75.37%) cases of CKD followed by DM in 12 (32.43%), CVA and IHD in 2 (5.40%) and 2 (5.40%) respectively and 43 (68.25%) of the males were found to be chronic alcoholic and 45 (71.42%) were chronic smokers when compared to females. There was no single case who was an addict for alcohol and smoking and 10 (15.87%) of male patients were in ICU with the bedridden condition and out of these, 6 (60%) were on antiplatelet therapy (aspirin 75 mg).
Co-morbidities and risk factors in CKD patients. (T-test used for p-value).
| Co-morbidities | Males (n,%) | Females (n,%) | p-value |
|---|
| HTN | 57 (90.47%) | 28 (75.37%) | 0.08 |
| DM | 32 (50.79%) | 12 (32.43%) | 0.114 |
| IHD | 6 (9.52%) | 2 (5.40%) | 0.725 |
| CVA | 8 (12.69%) | 2 (5.40%) | 0.407 |
| CLD | 10 (15.87%) | 0 | NA |
| Ch.SK | 45 (71.42%) | 0 | NA |
| Ch.AL | 43 (68.25%) | 0 | NA |
| Bed ridden | 10 (15.87%) | 0 | NA |
HTN: Hypertension; DM: Diabetes mellitus; IHD: Ischemic heart disease; CVA: Cardiovascular accident; CLD: Chronic lung disease; Ch.SK: Chronic smoker; Ch AL: Chronic alcoholic
[Table/Fig-3] showing the associated co-morbidities and risk factors that contributed to CVCRT formation. In this study, it was found that out of total 100 cases, 30 (30%) were found to have thrombus after two weeks of HD catheter insertion in IJV and CVCRT most commonly detected in the diabetic patient with CKD-10 (33.33%), followed by HTN-2 (6.66%), CAV-1 (3.33%), CLD-1 (3.33%) and no thrombus was detected in IHD patients. The most common risk factor for thrombus formation was chronic smoking, 12 (40%), followed by bedridden-2 (6.66%), and chronic alcoholic-2 (6.66%). The presence of thrombus and size was detected by duplex colour doppler USG of the neck and the thrombus was small in size in 25 cases at the entry site of the catheter (<14×5 mm) and large size of thrombus with 80% luminal blocks was observed in 5 cases (>4.1×2 cm).
Showing associated co-morbidities and Risk factors.
[Table/Fig-4] shows the size of diagnosed thrombus and gender distribution. Out of 30 diagnosed cases 25 (83.33%) were small thrombus and 5 (16.66%) were large size thrombus with 80% luminal block. Out of 25 cases of small thrombi, 22 (88%) were found in males and 3 (12%) were found in females and large thrombus was found in total 5 (16.66%) cases and all were diagnosed in males. The common presentation of CKD patients who required ICU admission was noted. Further, the lab parameters and outcome of the CKD patients was studied.
Showing size of thrombus with associated co-morbidities and gender distribution.
| Size of thrombus | Total | HTN | DM | CVA | CLD | IHD | BR | Ch.SK | Ch.AL |
|---|
| Small (<14×5 mm) | 25 | 2 | 8 | 1 | 1 | 0 | 0 | 11 | 2 |
| Large (4.1×2 cm) | 5 | 0 | 2 | 0 | 0 | 0 | 2 | 1 | 0 |
| Males | 27 | 2 | 9 | 1 | 0 | 0 | 1 | 12 | 2 |
| Females | 3 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 |
| Total | 30 | 2 | 10 | 1 | 1 | 0 | 2 | 12 | 2 |
HTN: Hypertension; DM: Diabetes mellitus; IHD: Ischemic heart disease; CVA: Cardiovascular accident; CLD: Chronic lung disease; Ch.SK: Chronic smoker; Ch AL: Chronic alcoholic
Out of total CKD patient, 40 came in ICU with c/o (complain of) SOB, in which 28 (70%) were males and 12 (30%) were females. Forty patient {22 (55%) males, 18 (45%) females} came in ICU with GW, and total 20 patients chief complaint of anuria {13 (65%) males and 7 (35%) females}. SOB was most common complaint by CKD patient followed by GW with male preponderance, as observed in this study. [Table/Fig-5] showed that 67 patients had haemoglobin <7 gm/dL, 88 patients had serum urea >200 mg/dL, 90 patients had serum creatinine >10 mg/dL with male preponderance [Table/Fig-6]. The RMD (70%) is the most common cause of CKD followed by renal stone. Out of a total, 100 CKD patient admitted in ICU throughout one-year total death was 25 [Table/Fig-7].
Showing clinical presentation in CKD in ICU.
| Complaints | Males | Females | Total |
|---|
| SOB | 28 | 12 | 40 |
| GW | 22 | 18 | 40 |
| Anuria | 13 | 7 | 20 |
| Total | 63 | 37 | 100 |
SOB: Shortness of breath; GW: Generalised weakness; CKD: Chronic kidney disease; ICU: Intensive care unit
Comparison of laboratory results in CKD patients.
| Laboratory reports | Males | Females | Total |
|---|
| CBC (Hb) <7 (gm/dL) | 40 | 27 | 67 (67%) |
| Serum urea >200 (mg/dL) | 56 | 32 | 88 (88%) |
| Serum creatinine >10 (mg/dL) | 58 | 32 | 90 (90%) |
Showing outcome and management of survival patients of Chronic Kidney Disease in Intensive Care Unit (ICU).
| Survival (N=75) | Death (N=25) | Management of survived patients | Total (N=100) |
|---|
| RMD (N=50) | N=20 | AV fistula and maintain on dialysis, RT | N=70 |
| Pyonephritis (N=8) | N=2 | Medical management | N=10 |
| Renal stone (N=12) | N=3 | PCNL | N=15 |
| Prostatomegaly (N=5) | 0 | TURP | N=5 |
RMD: Renal medical disease; AV: Arterio venous; PCNL: Percutaneous nephrolithotomy; TURP: Transurethral resection of the prostate
Discussion
The CVC insertion is the most commonly performed procedure in the ICU setting for various reasons like for the administration of various drugs, supportive therapy, for blood sampling, and most important for urgent dialysis in CKD patients. The procedure is associated with various complications, which is divided in early and late, thrombus formation with luminal occlusion being very common early complication in CKD patients.
Several serious complications are recorded in the various study conducted in favour of CVCRT including the tip is located deep in the mediastinum, life-threatening Pulmonary Embolism (PE) (15-25%) in symptomatic patients [21-24], upper-extremity Deep Vein Thrombosis (DVT), and infection [17,21,22,25]. Asymptomatic thrombosis may be clinically important as there is a strong association noted between asymptomatic CVCRT and catheter occlusion and CVCRI [25]. Venous Thromboembolism (VTE), DVT and PE have been studied in the general population, and its annual incidence in the adult population is approximately 1/1000, predominantly in the elderly [26-28].
The well-known risk factors are surgery, carcinoma, prolonged hospitalisation, immobilisation, obesity, pregnancy, puerperium, administration of exogenous hormones, inherited thrombophilia’s. In the present study, 30% of CKD patient had CVCRT, and DM is the most common co-morbidities (33.33%), and smoking (40%) is the dominant risk factor. Indirectly thrombus formation was mostly detected in DM patient with CKD followed by HTN and diabetic nephropathy is a most common cause of CKD worldwide [29]. CKD itself is a risk factor for VTE. Due to increasing incidence of DM, HTN, and Obesity, the number of CKD patients [30,31] with low GFR (On dialysis graded as renal failure) are very high in number approx. 13% with rate of increased incidence of VTE [32]. A study conducted by Keattiyoat W and Cushman M mentioned that due to underlying haemostatic derangement in CKD, these patients are more prone to symptomatic VTE as compared to general population [29].
Tendency of thrombus formation is very high in patients who are on chronic HD because of abnormalities in platelets and coagulation factors and there is no benefits noted till date by use of pharmacological treatment. It may be associated with ischemic heart disease, stroke, vascular access occlusion which increase patients hospital stay and cost of treatment [33-35]. Male preponderance was found in the present study in view of CKD on dialysis, associated comorbidities, risk factors and access thrombus formation and this is favoured by a study conducted by Katherine A who explained that more male patients underwent HD compared to female because of lack of awareness and social factors [32-34]. Men initiate HD early than female [35]. There are various risk factors such as age, body mass index, and plasma glucose level and habits of smoking, lifestyle which also contributes in fast progression of end stage renal disease in male patients [36,37]. The present study also observed Diabetes Mellitus and chronic smoking as high risk factors along with male preponderance, for fast progression of CKD patients on Dialysis.
Limitation(s)
This center is located in rural and tribal areas of Rajasthan, hence most patients belong to low socio-economic status, so severity of disease at the time of presentation was more because of poor accessibility of health services in this socioeconomic group.
Conclusion(s)
The CKD is a major health problem, belongs to the rural area. Maximum patients, unaware, come in the hospital in late-stage and require ICU admission and dialysis. Catheter-related thrombus formation in IJV is a common problem with male preponderance. Diabetes Mellitus and chronic smoking were high risk factors for developing these thrombus.
HTN: Hypertension; DM: Diabetes mellitus; IHD: Ischemic heart disease; CVA: Cardiovascular accident; CLD: Chronic lung disease; Ch.SK: Chronic smoker; Ch AL: Chronic alcoholic
HTN: Hypertension; DM: Diabetes mellitus; IHD: Ischemic heart disease; CVA: Cardiovascular accident; CLD: Chronic lung disease; Ch.SK: Chronic smoker; Ch AL: Chronic alcoholic
SOB: Shortness of breath; GW: Generalised weakness; CKD: Chronic kidney disease; ICU: Intensive care unit
RMD: Renal medical disease; AV: Arterio venous; PCNL: Percutaneous nephrolithotomy; TURP: Transurethral resection of the prostate