A hyperdynamic state in patients with cirrhosis is characterised by increased Cardiac Output (CO), plasma volume as well as a decreased Systemic Vascular Resistance (SVR) and blood pressure [1]. Initially, the impaired LV performance in cirrhotic patients was thought to be due to the direct toxic effect of alcohol [2].
Cirrhotic cardiomyopathy is the term used to describe a combination of symptoms suggestive of structural and functional cardiac changes resulting from liver cirrhosis. These encompass problems in systolic and diastolic dysfunction, electrophysiological changes and macroscopic and microscopic structural abnormalities. Alcoholic cardiomyopathy is a subtype of acquired dilated cardiomyopathy occurring as a result of high alcohol intake over a period of time. Hepatic cirrhosis culminates into hyperdynamic circulation, which leads to dysfunctions of cardiac structure and function that make up the Cirrhotic Cardiomyopathy (CCM) syndrome. This syndrome contains along with hyperdynamic circulation, systolic and diastolic dysfunctions, increased repolarisation of the ventricles, and problems with the sinus node in raising Heart Rate (HR) during increased activity [3-9].
Cardiac dysfunction in cirrhotic population occurs in the setting of a circulatory dysfunction and is characterised by dilated splanchnic vasculature. At the earlier stages of cirrhosis, the circulatory dysfunction is compensated by a hyperdynamic circulation. Later, the progression of liver disease and portal hypertension leads to progressive vasodilatation, which causes a decrease in the effective arterial blood volume that activates the Renin-Angiotensin-Aldosterone System (RAAS) and the Sympathetic Nervous System (SNS) [10]. These changes in the circulation can result in the cardiac dilatation of the left chambers and the beginning of functional cardiac changes. High norepinephrine levels cause impairment of β-adrenergic receptor function [11]. Factors apart from the sympathetic nervous activity and the aldosterone system have been suspected in the causation of cardiac dysfunction in cirrhosis. These are Nitric Oxide (NO), Carbon Monoxide (CMO) and endogenous cannabinoids [6]. Aggregation of these chemicals along the porto-systemic shunts may result in negative inotropic effect and these can also be involved in the pathogenesis of Left Ventricular Diastolic Dysfunction (LVDD) in Cardiomyopathy (CCM) [12]. Inflammation is implicated in the genesis of cardiac dysfunction particularly in decompensated cirrhosis. Cytokines can affect myocardial function in two ways, namely via the effects on both the myocyte contractility and the extracellular matrix [13] not only do they affect myocardial remodeling, but also the cytokines have been seen to have direct and indirect effects on myocardial function.
It has been estimated that as many as 50% of patients undergoing liver transplantation developed some signs of cardiac dysfunction and about 7-21% of patients died from heart failure in the post liver transplantation period [7,14]. Hence, this study was conducted to assess the occurrence of cardiac dysfunction in cirrhosis and to correlate with severity and aetiology of cirrhosis in our centre.
Materials and Methods
This cross-sectional study was conducted at Jawaharlal Nehru Medical College, Wardha, Maharashtra from September 2017 to September 2019. The approval from Institutional Ethics Committee was received on 30/09/2017 with Reference Number-DMIMS (DU)/IEC/2017-18/6754.
Sample size calculation: A total of 150 patients were enrolled according to sample size calculated with the following formula as N=Z 1-α/2*p* (1-p)/d2*; Where Zα/2=normal distribution at α/2=1.96; p=prevalence of cardiomyopathy in liver cirrhosis as per study of Somani PO et al., i.e., 30% [13]; d=desired margin of error 7%=0.07; n=1.962×0.30(1-0.30)=144.6. Patients presented to the hospital with complains suggestive of a presumptive diagnosis of liver cirrhosis (abdominal distension, pedal oedema, jaundice, altered sensorium) and were then diagnosed on the basis of clinical examination, laboratory parameters and ultrasonography findings.
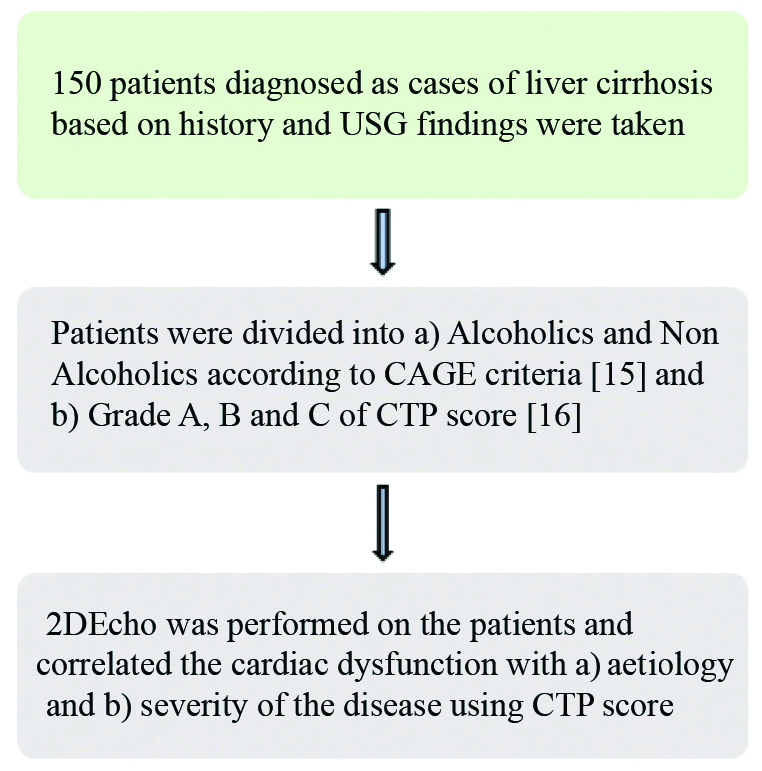
Inclusion criteria: The cases included cirrhotic patients either with or without ascites, diagnosis of cirrhosis was made on unequivocal clinical grounds (chronic liver disease stigmata, jaundice, ascites, oesophageal varices), deranged liver function tests and ultrasonographic features consistent with cirrhosis (diffuse alteration and nodular transformation of liver parenchyma and signs of portal hypertension). Flow chart of the study had been shown in [Table/Fig-1].
Flow chart showing the plan of study.
USG: Ultrasonography; CTP: Child-turcotte pugh
Exclusion criteria: The exclusion criteria were cases of documented pre-existing cardiac dysfunction or history of cardiovascular disorder in the past, cases of existing pulmonary disease, with a smoking history, all patients under 18 years of age and patients with known anaemia, hypertension, cardiac, endocrine and renal disease leading to cardiac dysfunction.
Diagnosed cases of liver cirrhosis were considered after taking informed consent, history of alcoholism established using CAGE criteria [15], classified into Child Pugh Score A, B, C [16] followed by a detailed echocardiographic assessment of each case for LV systolic and diastolic dysfunction. Echocardiographic examinations was done using 2-Dimensional and Doppler Echocardiographic techniques using the Wipro Echocardiography Machine, (Wipro GE VIVIDE SR- 460051 WXE [15]) with patient lying in the supine and left decubitus position.
Systolic dysfunction: Thus, Ejection Fraction was calculated using SIMPSON’S formula
LVEF (%)=(Left Ventricle End Systolic Volume (LVEDV)-Left Ventricle End Systolic Volume (LVESV)÷LVEDVReference normal value used=An EF of <55% was taken as systolic dysfunction. Normal Left Ventricular Ejection Fraction (LVEF) >55% [16]
Diastolic dysfunction: Diastolic function can be assessed by multiple parameters (e.g., E/E’, E/A, Isovolumic Relaxation Time (IVRT), E-Wave Deceleration Time (EDT), Pulmonary Flow). No single parameter is perfect or superior over another. So, a combination approach was taken and hence parameter E/e’ and E/A were taken for this study.
Four chamber views was obtained and optimised. LV diastolic function was assessed by Doppler interrogation of Trans mitral velocity at early (E) and late (A) LV filling. From the mitral inflow signal, we measured the E velocity (E), the A velocity (A) and the E/A ratio of early diastolic LV filling. Pulsed wave Tissue Doppler Imaging (TDI) was performed at the junction of the septal mitral annulus. Early diastolic velocities (e’ medial) were recorded and E/e’ medial ratio was calculated and patient were categorised as Presence or Absence of LV diastolic dysfunction according to the American Society of Echocardiography (ASE) guidelines [17]. LVDD was said to be present if E/A ratio (cm/second) was between 0.8-1.5, and septal e’ was <8 cm/second. It was said to be absent if E/A ratio was more than 1 and septal e’ more than 8 cm/second.
The grades of diastolic dysfunction were defined on the basis of E/A ratio as Grade I (impaired relaxation pattern) E/A <0.8, Grade II (Pseudo normal) as E/A 0.8-1.5, and Grade III (Restrictive filling) E/A >2. To distinguish between Normal and Pseudo normal patterns, authors take normal as E/A ratio more than 1 but less than 2, both decreasing with Valsalva, and no change in ratio, and E/septal e’ less than 10, whereas Pseudo normal has E/A ratio of 0.8-1.5, on Valsalva E decreases more than A and ratio decreases <1 and E/septal e’ is more than 1 [18].
Statistical Analysis
This was done by using descriptive and inferential statistics using Chi-square test, Pearson’s Correlation Coefficient and Multiple Regression analysis and software used in the analysis was Statistical Package for the Social Science (SPSS) 22.0, and p<0.05 was considered as level of significance.
Results
Out of 150 patients, mean age and duration of hospital stay (days) amongst study population was 45.15±13.41 years and 5.32±2.08 days, respectively. About 62% of the study population were alcoholics. Cardiac dysfunction was noted in 51 (LVSD in 9 patients and LVDD in 42 patients). LV diastolic dysfunction was observed in 28% of study population and systolic dysfunction in 6% of the population. Out of 42 patients, 24 had Grade I Diastolic dysfunction 10 had Grade II Diastolic dysfunction and 8 had Grade III Diastolic dysfunction. All other baseline characteristics are shown in [Table/Fig-2].
Baseline characteristics of the study population n=150.
| Characteristics | Values |
|---|
| Mean age (years) (Mean±SD) | 45.15±13.41 |
| Males, n (%) | 133 (88.7) |
| Females, n (%) | 17 (11.3) |
| Mean duration of stay at the hospital (days) (Mean±SD) | 5.32±2.08 |
| Mean pulse rate (bpm) (Mean±SD) | 80.88±5.4 |
| Mean blood pressure (mmHg) (Mean±SD) | 110/70±20/7.1 |
| Number of patients who had a history of alcoholism, n (%) | 93 (62) |
| Number of patients who had no history of alcoholism, n (%) | 57 (38) |
| Echocardiographic parameters |
| LV ejection fraction (%) (Mean±SD) | 58.02±6.77 |
| E/A ratio | 0.99-0.35 |
| E/e’ | 12.2-4.1 |
| Cases having LVSD, n (%) | 9 (6) |
| Cases having LVDD American Society of Echocardiography (ASE) grading [17], n (%) | 42 (28) |
| Grade I | 24 |
| Grade II | 10 |
| Grade III | 8 |
| Cases in CTP |
| CTP grade A | 84 |
| CTP grade B | 55 |
| CTP grade C | 11 |
LV: Left ventricler; LVSD: Left ventricular systolic dysfunction; LVDD: Left ventricular diastolic dysfunction; CTP: Child-turcotte-pugh
Among the 9 (6%) of patients having LVSD four was alcoholic and five non-alcoholic and this result had no statistically significant difference. Diastolic dysfunction was present in 69% of alcoholic patients and 31% of non-alcoholic patients with no statistically significant difference as shown in [Table/Fig-3].
Correlation of cardiac dysfunction with the aetiology of liver cirrhosis amongst study population.
| Variables | Alcoholic | Non-alcoholic | Total |
|---|
| Left ventricular systolic dysfunction (EF<55%) |
| Present | 4 (44.4%) | 5 (55.6%) | 9 (100%) |
| Absent | 89 (63.1%) | 52 (36.9%) | 141 (100%) |
| Total | 93 (62%) | 57 (38%) | 150 (100%) |
| r=0.069 p=0.263 |
| Left ventricular diastolic dysfunction |
| Present | 29 (69.0%) | 13 (31.0%) | 42 (100%) |
| Absent | 64 (59.3%) | 44 (40.7%) | 108 (100%) |
| Total | 93 (62%) | 57 (38%) | 150 (100%) |
| r=0.079 p=0.334 |
(Pearson’s Correlation Coefficient and p-value were used for statistical analysis)
EF: Ejection fraction
Out of the 9 cirrhotic patients with LVSD two patients were in grade A CTP, four in grade B CTP and three in grade C CTP and this was statistically significant as per Chi-square test. LV Diastolic dysfunction was in 17 (20.2%) of Grade A of Child Pugh Score, 14 (25%) of Grade B and 11 (100%) Grade C with statistically significant difference as shown in [Table/Fig-4].
Correlation of cardiac dysfunction with the severity of liver cirrhosis amongst study population.
| Variables | CTP A | CTP B | CTP C | Total |
|---|
| Left ventricular systolic dysfunction (EF <55%) |
| Present | 2 (22.2%) | 4 (44.4%) | 3 (33.4%) | 9 (100%) |
| Absent | 82 (58.2%) | 51 (36.2%) | 8 (5.6%) | 141 (100%) |
| Total | 84 (56%) | 55 (36.7%) | 11 (7.3%) | 150 (100%) |
| r=0.195 p=0.017 |
| Left ventricular diastolic dysfunction |
| Present | 17 (20.2%) | 14 (25%) | 11 (100%) | 42 (28%) |
| Absent | 67 (79.8%) | 41 (75%) | 0 (0%) | 108 (72%) |
| Total | 84 (100%) | 55 (100%) | 11 (100%) | 150 (100%) |
| r=0.199 p=0.004 |
(Pearson’s Correlation Coefficient and p-value were used for statistical analysis)
Logistic regression for the predictor of cardiac dysfunction in the form of systolic and diastolic dysfunction was statistically of no significant difference, as shown in [Table/Fig-5].
Logistic regression of the Left Ventricular (LV) Diastolic Dysfunction and Left Ventricular (LV) Systolic Dysfunction.
| Variables | Variables in the equation |
|---|
| B (LVDD) | B (LVSD) | S.E. (LVDD) | S.E. (LVSD) | Sig. (LVDD) | Sig. (LVSD) | Exp(B) (LVDD) | Exp(B) (LVSD) |
|---|
| Step 1a | Age | -0.022 | -0.024 | 0.015 | 0.028 | 0.134 | 0.403 | 0.978 | 1 |
| Gender (Male) | 1.180 | 18.606 | 0.797 | 9240.354 | 0.139 | 0.998 | 3.255 | 120409234 |
| History of alcohol (present) | 0.920 | 18.955 | 0.421 | 5228.222 | 0.029 | 0.997 | 2.511 | 170628242 |
| Constant | -1.654 | -38.645 | 1.137 | 10616.895 | 0.146 | 0.997 | 0.191 | 0.000 |
a. Variable(s) entered on step 1: age, gender A, history of alcohol.
B (coefficient for the constant); SE (standard error), Exp (B) exponentiation of the B coefficient; Sig. (significance level.)
Discussion
A total of 150 cases where the mean age was 45.15 years, with a male: female ratio of 8:1, out of which 62% population had a history of alcoholism. This study shows that 6% of the study population had systolic dysfunction which was similar to the study conducted by Punekar P and Thakur DK which also show 6% of the study population of 100 patients, which was similar in the pattern with Ashmawy MM et al., showing systolic dysfunction in 10% of the patients and Hammami R et al., which showed 17.5% patients with systolic dysfunction [20-22]. In the present study, diastolic dysfunction was observed in 28% of study population. The diastolic dysfunction observed in this study had no significant correlation with the aetiology of the liver cirrhosis, but the correlation of the dysfunction with the severity of the disease seen by Child Pugh Score was found to be statistically significant, especially in Child Pugh Score Grade C, where 100% of the cases had diastolic dysfunction. This finding was in agreement with the other various studies conducted globally [23,24]. Karagiannakis DS et al., also found 38% patients with diastolic dysfunction which was not associated with the severity of the disease [25]. Sampaio F and Pimenta J, and Rimbas RC et al., also found the diastolic dysfunction to be 44% and 47.8% [26,27].
On the contrary, Sidmal PS et al., conducted a similar study in the South Indian population where the diastolic dysfunction was seen to be 91.6% (31.6% mild and 60% moderate) but that might have been because their study population comprised of more cases of CTP class C patients (30 out of 60 cases) than this study [28]. Similar results were seen with Ashmawy MM et al., Hammami R et al., and Salari A et al., where the study population consisted of a higher number of Child Pugh C patients than our study [21,22,29].
However, in our study, logistic regression for predictors of systolic dysfunction like age, male sex and history of alcohol consumption were found to be of no statistically significant difference, suggesting that the above variables maybe confounders for cardiac dysfunction in liver cirrhosis. There was no significant correlation in our study regarding the LV systolic dysfunction or the LV diastolic dysfunction with aetiology of liver cirrhosis (alcoholic and non-alcoholic). Though, the direct effects of cirrhosis on the cardiac function has statistical significance in our study, the role of alcohol in the LVSD and LVDD could not be significantly established, which suggests that cardiac changes in alcoholic liver cirrhosis are more because of the pathophysiological effects of cirrhosis than as a result of alcohol. Other studies by Lee SS and Alexander J et al., also stated that cardiac changes were due to cirrhosis per se rather than alcohol [30,31].
In the present study, systolic dysfunction was present in Child Pugh Score B (44.4%) as compared to Child Pugh Score A (22.2%) and Child Pugh Score C (33.4%); whereas Diastolic dysfunction was in 20.2% in Grade A of Child Pugh Score, 25% in Grade B of Child Pugh Score and 100% Grade C of Child Pugh Score. By this analysis it could be suggested that the more severe the disease, the more diastolic dysfunction. This finding was consistent with other various studies by Punekar P and Thakur DK, Sidmal PS et al., and Lee SS which revealed diastolic dysfunction was found to be more in Child Pugh Score grade C as compared to Child Pugh Score grade B and Child Pugh Score grade A [20,28,30]. Ashmawy MM et al., showed 60 patients with diastolic dysfunction out of which 30 were in CPS grade C which is higher in frequency compared to our study [21]. This could have been because the study was conducted with 30 patients in each Child Pugh group.
It is recommended that all patients of liver cirrhosis should undergo echocardiographic evaluation for cardiac dysfunction so that morbidity and mortality after haemodynamics altering procedures like liver transplantation and Transjugular Intrahepatic Portosystemic Shunt (TIPSS) can be prevented.
Limitation(s)
A higher sample size would have shown more statistically significant correlation between the disease and the aetiology or severity. Details of long standing disease and follow-up were not included in this study.
Conclusion(s)
This study revealed higher prevalence of LV diastolic dysfunction as compared to LV systolic dysfunction in cases of liver cirrhosis. The correlation of left sided cardiac dysfunction with the aetiology of liver cirrhosis (alcoholic vs non-alcoholic) was statistically insignificant. The correlation of cardiac dysfunction with severity of liver cirrhosis (CTP scoring) was statistically significant thereby suggesting that the cardiac changes may be due to cirrhosis rather than alcohol.
LV: Left ventricler; LVSD: Left ventricular systolic dysfunction; LVDD: Left ventricular diastolic dysfunction; CTP: Child-turcotte-pugh
(Pearson’s Correlation Coefficient and p-value were used for statistical analysis)
EF: Ejection fraction
(Pearson’s Correlation Coefficient and p-value were used for statistical analysis)
a. Variable(s) entered on step 1: age, gender A, history of alcohol.
B (coefficient for the constant); SE (standard error), Exp (B) exponentiation of the B coefficient; Sig. (significance level.)