Imaging of Complete Vertebral Duplication with Normal Neurological Status: A Rare Case
Vishal Thakker1, Nisarg Thakker2, Manali Arora3, Rajan Patel4
1 Assistant Professor, Department of Radio-Diagnosis, Pramukhswami Medical College, Anand, Gujarat, India.
2 Postgraduate Resident, Department of Radio-Diagnosis, Pramukhswami Medical College, Anand, Gujarat, India.
3 Assistant Professor, Department of Radio-Diagnosis, Pramukhswami Medical College, Anand, Gujarat, India.
4 Postgraduate Resident, Department of Radio-Diagnosis, Pramukhswami Medical College, Anand, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Manali Arora, H. No. 1546, Sector 15, Sonipat, Haryana, India.
E-mail: drmanaliat@gmail.com
Vertebral Duplication represents the most severe aspect of the spectrum of Split Cord Malformations (SCMs). It is a rare anomaly with very few reported cases. Associated other spinal anomalies along with severe neurovascular and genitourinary anomalies may also co-exist. Hereby, authors report a case of a 21-years-old adult female, who presented with history of trauma, incidentally detected to be having complete lumbar duplication along with dural sac duplication and multiple complex segmentation anomalies in the form of incarcerated lateral hemivertebra, butterfly vertebra and non segmented lateral hemivertebra at D10 to D12 vertebrae. On Computed Tomography (CT) imaging these anomalies become well evident while the patient presented with no neurological manifestations or abnormalities. This is a rarely reported scenario in literature where no neurological symptoms are seen in a case of vertebral duplication.
Computed tomography, Lumbar vertebra, Spinal anomaly, Spinal duplication, Split cord
Case Report
A 21-year-old female patient presented with history of head injury due to road traffic accident followed by loss of consciousness. Subsequently, CT scan of dorso-lumbar spine was done which revealed complete lumbar spinal duplication anomaly along with dural sac duplication at Lumbar (L) 4 vertebral level. Also, L2-L3-L4 block vertebra, complete sacralisation of the L5 vertebra (Castellvi classification Type IIIB) [1] and posterior spina bifida occulta at lumbo-sacral level were observed. She had no difficulty in walking prior to the trauma. Patient had no neurovascular or genitourinary complaints.
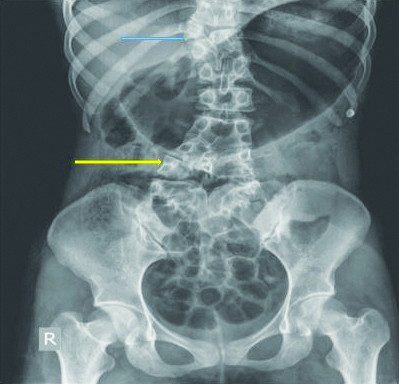
After evaluation for head injury, radiographs of the spine were obtained to rule out spinal injury [Table/Fig-1]. Incidentally, she was found to be having a duplication anomaly of the lumbar spine on radiography. Multiple complex segmentation anomalies in the form of incarcerated lateral hemivertebra, butterfly vertebra and non segmented lateral hemivertebra at Dorsal (D) 10 to D12 vertebrae [Table/Fig-2]. Mild scoliosis involving lower dorso-lumbo-sacral spine. Since patient had normal neurological status post-management for head trauma, she was kept on observation for spinal anomalies.
Plain radiograph Anteroposterior (AP) view of lumbo-sacral spine and pelvis shows Hemi vertebra (blue arrow) and vertebral duplication (yellow arrow) amongst other vertebral anomalies.
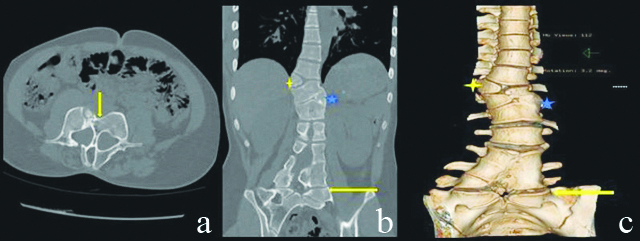
CT Axial bone window images: (a) of lumbar spine at the level of L4 vertebra revealed incomplete lumbar spinal duplication anomaly (Yellow Arrow) along with dural sac duplication at L4 vertebral level. Coronal Bone window; (b) and Volume Rendered Coronal images; (c) show multiple complex segmentations anomalies (yellow arrows) in the form of incarcerated lateral hemi vertebra, butterfly vertebra and non segmented lateral hemivertebra at D10 to D12 vertebral levels (Yellow and Blue Asterix) with complete sacralisation of the L5 vertebra.
Discussion
The Split Cord Malformations (SCMs) are congenital anomalies which are rare and include a wide spectrum of abnormalities. The milder versions include spina bifida occulta to fibrous septae between the two hemicords. The most severe pattern of SCM presents as complete bony duplication of the vertebral column each harbouring its own spinal hemicord. This is often associated with other bony anomalies of the spine causing neurological deficit [1,2]. Only few rare cases of vertebral duplication with normal neurological status are reported in literature [2,3].
Pang D et al., classified the Diastematomyelia in two types. Type I consists of two hemicords, each within its own dural sac [4]. The separation is by a median osteocartilaginous septum. Type II is the presence of two hemicords within a single dural sac separated by a fibrous septum. Present case is classified as Type I SCM as per this classification however, each hemicord has its own bony canal.
In evaluation of vertebral anomalies, plain x-ray is the first modality of investigation with both AP and lateral view. It may show vertebral anomalies and bony spur. Magnetic Resonance Imaging (MRI) is the investigation of choice which shows the exact morphology of the cord and its hemi divisions along with the extent and pattern of splitting. It also shows associated anomalies such as tethering of cord, thickening of filum terminale. CT scan with sagittal, coronal and volume rendered reformations is helpful for better bony details [5].
Complete vertebral duplication is a rare congenital entity with only few reported cases. Though, often associated with other bony anomalies and severe genitourinary and gastrointestinal features, asymptomatic patients with normal neurovascular status have also been reported [2,6]. Incesu L et al., presented a 15-year-old female with lower back pain who showed asymmetric lumbar spine duplication on radiological evaluation [2]. She had a tethered cord with a filum terminale lipoma in the sacrum. Since the neurological status of the patient was normal, she was followed by conservative treatment.
Cebesoy O et al., also presented a case of lumbar duplication in an adult male with no associated anomalies and intact neurological status [3]. Similar observations were made by Morgan EN et al., who described complete duplication of lumbar spine and sacrum in a six-year-old child and Ahmed S et al., who described a complete thoraco-lumbar duplication in a six-year-old with overlying lipoma [7,8]. Both these patients had intact neurological status with no focal deficit.
While, it has been proposed in literature that both Type I and II of SCM must be surgically intervened; in view of possible tethering of cord with growing age and manifestation of neurological deficits [9]. In patients like the present one, with no presentation of neurological symptoms and no associations, a more conservative approach with observation has now been suggested by Ahmed S et al., and Goldberg BA et al., [8,10]. A close monitoring is advised in such cases with judicial balancing of the risks to benefits of surgical intervention.
Conclusion(s)
Though multiple clinical presentations and associations of vertebral duplication are known, a normal neurological status is rare but reported. Incidental detection of vertebral anomalies occurs in these cases which may be followed-up non-surgically.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jan 06, 2021
Manual Googling: Apr 06, 2021
iThenticate Software: Apr 30, 2021 (13%)
[1]. Nardo L, Alizai H, Virayavanich W, Liu F, Hernandez A, Lynch JA, Lumbosacral transitional vertebrae: Association with low back painRadiology 2012 265(2):497-503.10.1148/radiol.1211274722952380 [Google Scholar] [CrossRef] [PubMed]
[2]. Incesu L, Karaismailoglu TN, Selcuk MB, Neurologically normal complete asymmetric lumbar spine duplicationAmerican Journal of Neuroradiology 2004 25(5):895-96. [Google Scholar]
[3]. Cebesoy O, Mete A, Karsli B, Complete lumbar spine duplication in a neurologically intact manThe Journal of Spinal Cord Medicine 2009 32(1):99-102.10.1080/10790268.2009.1176075919264056 [Google Scholar] [CrossRef] [PubMed]
[4]. Pang D, Dias MS, Ahab-Barmada M, Split cord malformation: Part I: A unified theory of embryogenesis for double spinal cord malformationsNeurosurgery 1992 31(3):451-80.10.1227/00006123-199209000-000101407428 [Google Scholar] [CrossRef] [PubMed]
[5]. Kumar J, Afsal M, Garg A, Imaging spectrum of spinal dysraphism on magnetic resonance: A pictorial reviewWorld Journal of Radiology 2017 9(4):178-90.10.4329/wjr.v9.i4.17828529681 [Google Scholar] [CrossRef] [PubMed]
[6]. Sinha S, Agarwal D, Mahapatra AK, Split cord malformations: An experience of [4] 203 casesChild’s Nervous System 2006 22(1):03-07.10.1007/s00381-005-1145-115933885 [Google Scholar] [CrossRef] [PubMed]
[7]. Morgan EN, Caskey SM, Bronson WE, Baird GO, Tompkins BJ, Caskey PM, Lumbar spine duplication: A case reportJournal of Pediatric Orthopaedics B 2016 25(3):275-77.10.1097/BPB.000000000000027726849460 [Google Scholar] [CrossRef] [PubMed]
[8]. Ahmed S, Xenos C, Hockley AD, Thoraco-lumbar duplication of the spineChild’s Nervous System 2000 16(9):603-06.10.1007/PL0000730111048637 [Google Scholar] [CrossRef] [PubMed]
[9]. Kumar R, Singh V, Singh SN, Split cord malformation (occult spina bifida): An Indian scenarioJK Science 2005 7(4):192-94. [Google Scholar]
[10]. Goldberg BA, Erwin WD, Heggeness MH, Lumbar spine duplication presenting as adolescent scoliosis: A case reportSpine 1998 23(4):504-07.10.1097/00007632-199802150-000219516710 [Google Scholar] [CrossRef] [PubMed]