Association of Portal Vein Indices with Upper Gastrointestinal Endoscopic Findings in Patients with Cirrhosis of Liver
MS Revathy1, Ajay Kandpal2, B Sumathi3, S Chitra4, M Manimaran5, G Sathya6
1 Professor and Head, Department of Gastroenterology, Stanley Medical College, Chennai, Tamil Nadu, India.
2 Senior Resident, Department of Gastroenterology, Stanley Medical College, Chennai, Tamil Nadu, India.
3 Associate Professor, Department of Gastroenterology, Stanley Medical College, Chennai, Tamil Nadu, India.
4 Assistant Professor, Department of Gastroenterology, Stanley Medical College, Chennai, Tamil Nadu, India.
5 Assistant Professor, Department of Gastroenterology, Stanley Medical College, Chennai, Tamil Nadu, India.
6 Assistant Professor, Department of Gastroenterology, Stanley Medical College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ajay Kandpal, Flat 601, Tower 9, North Town, Stephenson Road, Perambur, Chennai, Tamil Nadu, India.
E-mail: kandykilroy@gmail.com
Introduction
Upper Gastrointestinal (UGI) bleed is major cause of mortality and admissions in cirrhotics. Timely initiation of prophylaxis reduces the burden of disease. Few endoscopists at periphery are compelled to look at other options to identify at risk patients. This study explores Portal Vein Diameter (PVD) as an option while taking clues and corrections from past studies.
Aim
To identify any association between increase in portal pressure with appearance of oesophageal varices.
Materials and Methods
This was an observational cross-sectional study on 75 patients of cirrhosis of liver, from November 2018 to June 2019. Baseline characteristics were noted and assessment of the severity of disease was done. Endoscopy and Portal Vein (PV) Doppler was performed in same time frame. Analysis of Variance (ANOVA) and unpaired t-tests were used for analysis of the collected data. A p-value <0.05 was considered significant in both the tests.
Results
Grade of varices was found to have a direct relationship with portal diameter and a statistically significant inverse relationship with Portal Venous flow Velocity (PVV) (p-value 0.037). Total 28 patients had active bleed or history of UGI bleed and showed higher mean portal diameter and lower average portal velocity compared to patients without any history of variceal bleeding. A statistically significant relation was found between diameter of Portal Vein (PV) and Child-Turcotte-Pugh (CTP) grade from A to C. Patients with grade C had on an average, the biggest portal diameter and lowest PVV. Patients with Model for End-Stage Liver Disease (MELD) scores values higher than 14 and had higher mean PV diameter and a lower mean PVV. Also, hepato-fugal flow was recorded with advanced cirrhosis.
Conclusion
In advanced cirrhosis, the PV Doppler can be thought of as a substitute to endoscopy in starting primary medical prophylaxis, though more extensive study is needed to arrive at a definitive conclusion.
Gastroesophageal varices, Portal vein diameter, Portal vein flow velocity
Introduction
The UGI bleed is one of the most commonly encountered medical emergencies and a major cause of mortality and hospital admissions in cirrhotics. The most common reason is the bleeding gastroesophageal varices; a potentially lethal complication unless rapidly controlled, arising by virtue of portal hypertension, an inexorable side effect of liver cirrhosis [1,2]. Portal hypertension is defined when the pressure gradient between portal vein and inferior vena cava is increased to more than 5 mmHg [3,4]. But to measure this gradient, the tests available are invasive and not readily available in peripheral areas [3,5].
Almost 35 to 80% of patients with cirrhosis have oesophageal varices, more so in patients with CTP grade C cirrhosis (up to 85%) out of these almost one-third patients experience episodes of variceal bleeding [1,6]. The first bleeding episode can cause mortality in up to 40% of patients. Outcome of the bleeding is usually related to the severity of the underlying cirrhosis [7]. Ranging from 0% in CTP grade A to almost 40% in grade C [8]. Endoscopy is the gold standard in diagnosis of varices but is an invasive procedure requiring a lot of expertise and still carries some risk of bleeding [3,4]. Besides its diagnostic value, ability to perform preventive or emergency treatment through endoscopy provides an added benefit [9]. Periodic screening by endoscopy is required to assess the progression of portal hypertension or varices thus making it unpleasant as well as expensive for the patients. Also, it is important to note that half of the patients with portal hypertension may not develop varices even in 10 years therefore will be undergoing unnecessary screening. Moreover, lesser availability of endoscopy units as well as limited number of expert Endoscopists, in the peripheral region compels to look at other options for early identification of the patients at risk [10,11]. Timely initiation of prophylaxis carried before onset of index bleed, either medical in form of Non-Selective Beta Blockers (NSBB) or intervention like Endoscopic Variceal Ligation (EVL), reduces the burden of disease, and can be life-saving at times. So, assessment of bleeding risk by screening and triaging of the patients that either needs further investigation or immediate prophylaxis at the earliest, can significantly improve the prognosis [12].
In recent years, multiple researchers have come forward with various studies exploring several non-invasive procedures in evaluating various facets of portal hypertension in cirrhotics, although their clinical value is still not proven [3,5,13,14]. Colour Doppler ultrasonography is one such alternative that has been brought to notice. It can be used to correlate the portal vein indices (portal vein diameter and portal vein velocity) and presence or absence of oesophageal varices [3,5-7]. Large varices are mostly associated with higher ultrasonographic portal venous diameter [15]. Other parameters including splenic enlargement, ascitis, presence of collateral vessels and changes in splenic and hepatic arterial resistance can also be identified using colour Doppler [1,7]. Its availability even at the peripheral regions and absence of any side effects due to the procedure tilts the scale in its favour [5-7].
This study aimed to identify any significant association between increases in portal pressure with appearance of oesophageal varices. It explored the possibility of establishing PV Doppler as a screening tool to start primary prophylaxis for UGI bleed in cases of cirrhosis and also for long term monitoring.
Materials and Methods
A cross-sectional observational study was conducted over a period of eight months on patients’ of cirrhosis of liver with varied CTP status. Total 75 patients, admitted between November 2018 and June 2019, were included in the study using a convenient sampling method. The study was conducted in a tertiary care hospital, Stanley Medical College, Chennai, Tamil Nadu, India. The Institutional Ethical Committee approved the study (meeting held on 3rd April 2019).
Inclusion criteria: Patients of any gender 18 to 75 years of age having a confirmed diagnosis of cirrhosis of liver and presenting for the first time were enrolled in the study.
Exclusion criteria: Patients with bleeding disorders of any kind, immunocompromised status and those patients on any treatment or those who have undergone endoscopic or surgical treatment for varices in the past were excluded from the study.
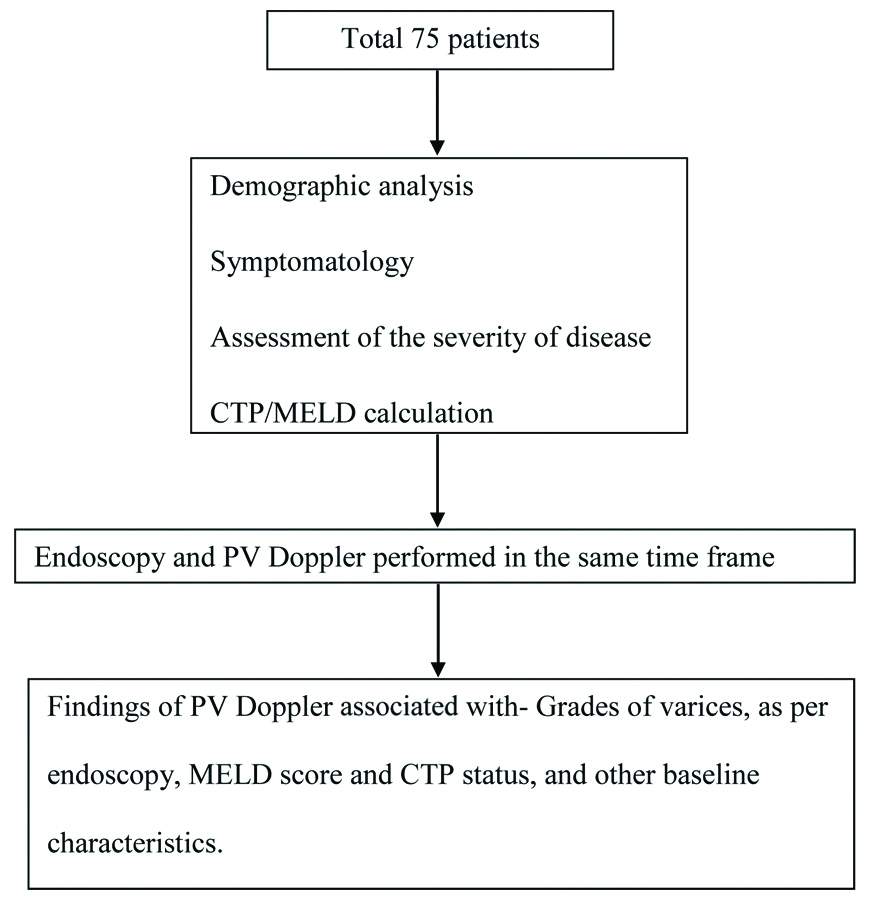
Baseline characteristics were noted as per performa. Assessment of the severity of disease was done using CTP and MELD scores. The endoscopy and PV Doppler were performed in same time frame. The process has been summarised in [Table/Fig-1].
Study methodology.
PV: Portal vein; CTP: Child-turcotte-pugh; MELD: Model for endstage liver disease
Statistical Analysis
The findings of PV Doppler were assessed for any association with grades of varices, MELD score and CTP status, and also with other baseline characteristics using ANOVA and unpaired t-tests for analysis of the collected data. A p-value <0.05 was considered significant in both the tests. The cut-off of 14 MELD score was selected by applying the Youden’s Index after plotting the Reciever Operating Characteristic (ROC) curve. Statistical analysis was conducted using graph pad and Microsoft excel.
Results
Out of the 75 patients included in the study, 60 were males. The mean±SD portal diameter of 11±4.12 mm and mean portal velocity 7.18±4.09 cm/sec was recorded. Twelve patients were found to have grade 1 varices. Grades of varices had an inverse relationship with portal venous velocity, which was found to be statistically significant on assessment using one-way ANOVA (p-value=0.037) and a direct relationship with the diameter of Hilum, but it was not statistically significant. Twenty-eight patients were found to have presented with or had history of UGI bleed. These patients had a mean portal diameter of 10.36±2.873 mm and a mean portal velocity of 10.2±6.0 cm/sec. Patients presenting with, or those who have been treated for UGI bleed were observed to have higher mean portal vein diameter and lower mean PVV, compared to those presenting without UGI bleed but these relations were found to be statistically non-significant [Table/Fig-2].
Association of varices with Portal Vein Diameter (PVD) and Portal Vein flow Velocity (PVV).
| Varices | Number | PVD (mm) | Statistical outcome | PVV (cm/sec) | Statistical outcome |
|---|
| Grade 1 | 12 | 9.225±3.146 | One-way ANOVA:f-ratio=0.9361p-value=0.399825. | 12.834±5.638 | One-way ANOVA:f-ratio=3.53818.p-value=0.037594. |
| Grade 2 | 24 | 10.371±2.722 | 9.895±5.219 |
| Grade 3 | 11 | 11±4.123 | 7.182±4.094 |
| Active bleeding/history of bleeding | 28 | 10.36±2.873 | Unpaired t-test: p-value >0.05 | 10.2±6.0 | Unpaired t-test: p-value >0.05 |
| No Active bleeding/history of bleeding | 47 | 9.98±2.70 | 10.43±4.2266 |
On categorising as per Child Pugh criteria, 38 patients had grade C cirrhosis and mean portal diameter of 10.6±2.42 mm and Portal velocity of 9.60±5.47 cm/sec. Twenty-eight patients presented with grade B cirrhosis having a mean portal diameter of 9.04±2.51 mm and mean portal velocity of 11.29±4.69 cm/sec. Nine patients were recorded to have grade A cirrhosis with mean portal diameter 6.43±2.07 mm and portal velocity of 11.8 6±5.34 cm/sec. A significant relationship was found between diameter of PV and CTP grade from A to C, patients with grade C had on an average the biggest portal diameter (p-value=0.00027). Although the mean PVV was seen to fall with the increase in CTP grade from A to C, it was not statistically significant [Table/Fig-3].
Association of CTP status with Portal Vein Diameter (PVD) and Portal Vein flow Velocity (PVV).
| CTP grade | N | PVD (mm) | Statistical outcome | PVV (cm/sec) | Statistical outcome |
|---|
| A | 9 | 6.43±2.07 | One-way ANOVA:f-ratio=9.43361.p-value=0.00027. | 11.86±5.34 | One-way ANOVA:f-ratio=1.00365.p-value=0.37 |
| B | 28 | 9.04±2.51 | 11.29±4.69 |
| C | 38 | 10.6±2.42 | 9.60±5.47 |
CTP: Child-turcotte-pugh grading
On comparing portal values with corresponding MELD scores, it was observed that patients with MELD values higher than 14 had higher mean PV diameter and lower mean PVV. On assessment of MELD scores 15 patients were found to have scores higher than 14, these patients had a mean portal diameter of 8.09±2.77 mm and a mean portal velocity of 11.73±4.74 cm/sec. The relationship between MELD Score and PV diameter was found to be statistically significant (p-value=0.0089 using unpaired t-test) [Table/Fig-4]. Another finding observed was that, the advanced disease with higher CTP grade and MELD scores more than 14 were more likely to have hepato-fugal flow.
Association of MELD score with Portal Vein Diameter (PVD) and Portal Vein flow Velocity (PVV).
| MELD score | Number | PVD (mm) | Statistical outcome | PVV (cm/sec) | Statistical outcome |
|---|
| >14 | 15 | 8.09±2.77 | Unpaired t-test: p-value=0.0089. | 11.73±4.74 | Unpaired t-test: p-value=0.039 |
| <14 | 50 | 11.734±4.74 | 10.360±5.61 |
Discussion
All chronic liver disease patients do not have varices and all varices do not bleed. This fact envisages whether routine endoscopy in all cirrhotics is justified. In the present study, 63% patients of cirrhosis of liver had varices. The relationship between the grade of varices and portal velocity was found to be statistically significant. A total of 16% patients with grade 3 varices had a lower mean portal velocity and a higher mean portal diameter. Similar results were reported in a study by Li FH et al., [1]. Even the patients with active UGI bleed or history of the same were noted to be having higher mean portal diameter, and a lower mean portal velocity, strengthening the findings of this study of a probable relationship between Doppler findings and variceal bleed.
Upon assessment of the relationship of Doppler and the grade of cirrhosis, 51% patients had CTP grade C. A statistically significant relationship was found between PV diameter and CTP grade from A to C. The mean PVV was seen to fall with the increase in CTP grade from A to C, it was not statistically significant as depicted in [Table/Fig-4]. Another finding was a statistically significant relationship, between higher MELD score, especially more than 14 and high PV diameter as well as a low PV velocity. Similar results were found in a study by Ali WI et al., and Yan G et al., [16,17]; although there were a few studies that claim this relation to be untrue [5,18,19]. Another finding observed was that, the advanced disease with higher CTP grade and MELD scores more than 14 were more likely to have hepato-fugal flow (no data shown), this finding is supported by findings from the study by Gaiani S et al., [18].
Although PV Doppler is not in any way equivalent to the gold standard i.e., endoscopy, several other studies like this, also believe PV Doppler to be a good alternative to endoscopy for assessment of varices and portal vein size and portal velocity to be an indicator of bleeding oesophageal varices [20-23].
Limitation(s)
Nevertheless, the study does have several limitations. The sample size was relatively small as it was restricted by no. of patients presenting to the hospital over the duration of the study. Also PV Doppler has its own limitations by being a subjective investigation.
Conclusion(s)
In advanced cirrhosis, the PV Doppler can be thought of as a substitute to endoscopy in starting primary medical prophylaxis. This has more importance for cirrhotic patients in a developing country like India where to assess the disease progression; repeated screening by endoscopy is not always available or affordable, especially in the resource constricted settings. And as we know that, timely initiation of prophylaxis has proven benefits for outcome of the patients, using Doppler as a substitute can have a significant impact. Hence, we are justified in starting primary medical prophylaxis in cirrhotic patients on the basis of the PV Doppler and general condition of the patient. A multicentre, well-designed more extensive study with larger group of patient is recommended, for further development and research in this area so as to arrive at a definitive conclusion.
CTP: Child-turcotte-pugh grading
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 15, 2020
Manual Googling: Feb 22, 2021
iThenticate Software: Apr 17, 2021 (14%)
[1]. Li FH, Hao J, Xia JG, Li HL, Fang H, Hemodynamic analysis of esophageal varices in patients with liver cirrhosis using color Doppler ultrasoundWorld J Gastroenterol 2005 11(29):4560-65.10.3748/wjg.v11.i29.456016052688 [Google Scholar] [CrossRef] [PubMed]
[2]. Bhasin DK, Malhi NJ, Variceal bleeding and portal hypertension: Much to learn, much to exploreEndoscopy 2002 34(2):119-28.10.1055/s-2002-1984511822007 [Google Scholar] [CrossRef] [PubMed]
[3]. Vaishnav B, Bamanikar A, Chatterjee L, Grewal G, Kakrani AL, Comparative study for the prediction of large oesophagheal varices by ultrasound doppler and serum markers in portal hypertension due to liver cirrhosisThe Journal of Medical Research 2018 4(1):48-52.10.31254/jmr.2018.4111 [Google Scholar] [CrossRef]
[4]. Vanbiervliet G, Pomier-Layrargues G, Huet PM, Invasive diagnosis of portal hypertension in cirrhosis: A critical evaluation of the hepatic venous pressure gradient measurementGastroenterol Clin Biol 2005 29(10):988-96.10.1016/S0399-8320(05)88171-0 [Google Scholar] [CrossRef]
[5]. Achim CA, Bordei P, Dumitru E, The role of ultrasonography in the evaluation of portal hemodynamics in healthy adults and pathologic conditionsARS Medica Tomitana 2016 2(22):128-34.10.1515/arsm-2016-0022 [Google Scholar] [CrossRef]
[6]. Nemichandra Salam KS, Kanse VY, Shiakh N, Singh D, Singh K, Non endoscopic predictors of esophageal varices in patients with cirrhosis of liverIOSR Journal of Dental and Medical Sciences 2015 14(1):65-68. [Google Scholar]
[7]. Masoud S, Elzefzafy WM, Elnaggar A, Saleh OI, Ibrahiem A, Color Doppler ultrasonography changes of portal circulation after band ligation of esophageal varices in Egyptian patients with chronic liver diseaseAmerican Journal of Medicine and Medical Sciences 2018 8(7):145-54. [Google Scholar]
[8]. Cremers I, Ribeiro S, Management of variceal and nonvariceal upper gastrointestinal bleeding in patients with cirrhosisTher Adv Gastroenterol 2014 7(5):206-16.10.1177/1756283X1453868825177367 [Google Scholar] [CrossRef] [PubMed]
[9]. Akhavan Rezayat K, Mansour Ghanaei F, Alizadeh A, Shafaghi A, Babaei Jandaghi A, Doppler surrogate endoscopy for screening esophageal varices in patients with cirrhosisHepat Mon 2014 14(1):e1123710.5812/hepatmon.1123724497873 [Google Scholar] [CrossRef] [PubMed]
[10]. Zhang CX, Xu JM, Li JB, Kong DR, Wang L, Xu XY, Predict esophageal varices via routine trans-abdominal ultrasound: A design of classification analysis modelJ Gastroenterol Hepatol 2016 31(1):194-99.10.1111/jgh.1304526197990 [Google Scholar] [CrossRef] [PubMed]
[11]. Shastri M, Kulkarni S, Patell R, Jasdanwala S, Portal vein doppler: A tool for noninvasive prediction of esophageal varices in cirrhosisJ Clin Diagn Res 2014 8(7):MC12-15. [Google Scholar]
[12]. Elkenawy YN, Elarabawy RA, Ahmed LM, Elsawy AA, Portal vein flow velocity as a possible fast noninvasive screening tool for esophageal varices in cirrhotic patientsJGH Open 2020 4(4):589-94.10.1002/jgh3.1230132782943 [Google Scholar] [CrossRef] [PubMed]
[13]. Uppalapati S, Lokesh S, Correlation of portal vein diameter with the presence of oesophageal varices in chronic liver disease: A prospective studyInt J Adv Med 2018 5(4):859-64.10.18203/2349-3933.ijam20182529 [Google Scholar] [CrossRef]
[14]. Shanker R, Banerjee S, Anshul Ganguly S, Bansal S, Uppal A, A study of association of portal vein diameter and splenic size with gastro-esophageal varices in liver cirrhosis patientsIOSR Journal of Dental and Medical Sciences 2016 15(9):125-29.10.9790/0853-150906125129 [Google Scholar] [CrossRef]
[15]. D’Amico G, Pagliaro L, Bosch J, The treatment of portal hypertension: A meta-analytic reviewHepatology 1995 22(1):332-54.10.1002/hep.18402201457601427 [Google Scholar] [CrossRef] [PubMed]
[16]. Ali WI, Hammad MI, Abu AMZ, Heikal IA, Association between portal vein colored doppler ultrasound findings and severity of liver disease in cirrhotic patients with portal hypertensionAIMJ 2020 March 10.21608/aimj.2020.22659.1095 [Google Scholar] [CrossRef]
[17]. Yan G, Duan Y, Ruan L, Chao T, Yang Y, A study on the relationship between ultrasonographic score and clinical score (MELD, CPT) in cirrhosisHepatogastroenterology 2005 52(65):1329-33. [Google Scholar]
[18]. Gaiani S, Bolondi L, Bassi SL, Zironi G, Siringo S, Barbara L, Prevalence of spontaneous hepatofugal portal flow in liver cirrhosis. Clinical and endoscopic correlation in 228 patientsGastroenterology 1991 100(1):160-67.10.1016/0016-5085(91)90596-D [Google Scholar] [CrossRef]
[19]. Dib N, Konate A, Oberti F, Calès P, Noninvasive diagnosis of portal hypertension in cirrhosis. Application to the primary prevention of varicesGastroenterol Clin Biol 2005 29(10):975-87.Article in French10.1016/S0399-8320(05)88170-9 [Google Scholar] [CrossRef]
[20]. Plestina S, Pulanic R, Kralik M, Plestina S, Samarzija M, Colour Doppler ultrasonography is reliable in assessing the risk of esophageal variceal bleeding in patients with liver cirrhosisWien Klin Wochenschr 2005 20(19-20):711-17.10.1007/s00508-005-0424-x16416372 [Google Scholar] [CrossRef] [PubMed]
[21]. Bhattarai S, Gyawali M, Dewan K, Shrestha G, Patowary B, Sharma P, Study of portal vein diameter and spleen size by ultrasonography and their association with gastro-esophageal varicesNepalese Journal of Radiology 2017 4(2):06-14.10.3126/njr.v4i2.18482 [Google Scholar] [CrossRef]
[22]. Bosch J, Groszmann RJ, Shah VH, Evolution in the understanding of the pathophysiological basis of portal hypertension: How changes in paradigm are leading to successful new treatmentsJ Hepatol 2015 62(1 Suppl):S121-30.10.1016/j.jhep.2015.01.00325920081 [Google Scholar] [CrossRef] [PubMed]
[23]. Zaman A, Becker T, Lapidus J, Benner K, Risk factors for the presence of varices in cirrhotic patients without a history of variceal hemorrhageArch Intern Med 2001 161(21):2564-70.10.1001/archinte.161.21.256411718587 [Google Scholar] [CrossRef] [PubMed]