The glossary of prosthodontic terms defines edentulism as ‘the state of being edentulous or without natural teeth [1].’ Since some sort of treatment is required for a completely edentulous individual, a more apt definition would be “the physical state of the jaw(s) following removal of all erupted teeth and the condition of the supporting structures available for reconstructive or replacement therapies [2].” Edentulism is a chronic irreversible state and a terminal consequence of a multifactorial process including biological (caries, periodontal disease, pulpal pathology, trauma, oral cancer) and patient-related factors (access to care, patient’s choices, treatment options, etc.,) [3]. It has an impact on chewing efficiency, nutrition, and general health, which lessens the oral health-related quality of life [4-10].
The complete loss of dentition affects numerous normal and vital human functions, including the ability to perform two of the most vital tasks of life that are eating and speaking; thus it can be considered a disability [11,12]. Complete loss of teeth is from the same group of known variable risk factors as other noncommunicable diseases like smoking, use of alcohol, and harmful carbohydrate-rich dietary behaviors [13]. Thus, edentulism satisfies the World Health Organisation (WHO) definition of physical impairment and can present challenges for those plagued with this ailment [14,15]. It remains a huge global health care liability, and will for the near future [16-18]. Thus, there is a growing demand for complete denture prostheses in the future, as it is a worldwide problem [5,19-22].
To frame a proper treatment plan for an edentulous patient, information obtained from various diagnostic aids needs to be classified according to their treatment based on complexity. The lack of a classification system and referral has forever been an obstacle for an accurate system of treatment planning among prosthodontists [23]. Consequently, the American College of Prosthodontists (ACP) formed a classification system to answer all these queries and help in treatment planning. McGarry TJ et al., proposed various classifications, including the PDI for completely edentulism (1999), partially edentulous patients (2002), and completely dentate patients (2004) [2,24,25]. These were implemented to diagnose patients in need of prosthetic treatment based on the complexity of the oral conditions seen at the first diagnostic appointment [26].
Materials and Methods
The study was a cross-sectional survey conducted in the outpatient clinics of Ibn Sina National College, Jeddah, Saudi Arabia from April 2019 to December 2019. The study was conducted after obtaining approval from the Institutional Ethical Committee (IEC Ref No. H-24-13022019). A total of 122 completely edentulous patients of Saudi and non-Saudi origin were selected based on convenient sampling as per previous studies [7,27]. The purpose of the detailed clinical and radiographic examination was explained and written informed consent was obtained from the patient.
Inclusion and Exclusion criteria: Completely edentulous patients of all age groups who were willing to get their treatment with complete dentures in the dental school were included in this study.
However, completely edentulous patients with maxillofacial defects, craniofacial abnormalities, bone grafts, oral manifestations of systemic disease (lupus erythematosus, pemphigus vulgaris, Crohn’s disease, etc.,), those desiring dental implants, retained roots, and those who were weak and unable to tolerate the treatment were excluded.
Clinical and Radiographic Examinations
Eight people were included in this study. Five interns and two teaching assistants (dentists who had just graduated), were oriented and trained in the calibration process to record the PDI worksheet by a prosthodontist. Demographic details age, gender, nationality, all appropriate clinical data (intraoral and extraoral) [7], and the patient’s medical and dental history were recorded. The intra-examiner reliability and inter-examiner reliability were assessed using the Kappa coefficient which was 0.90, which reflects ‘almost perfect agreement.’ All the people involved in this study were further oriented about the four main diagnostic criteria of PDI.
The four criteria were:
1. Radiographic mandibular bone height [Table/Fig-1] [2]
Mandibular bone height seen in Orthopantomagram (OPG) (Type III).
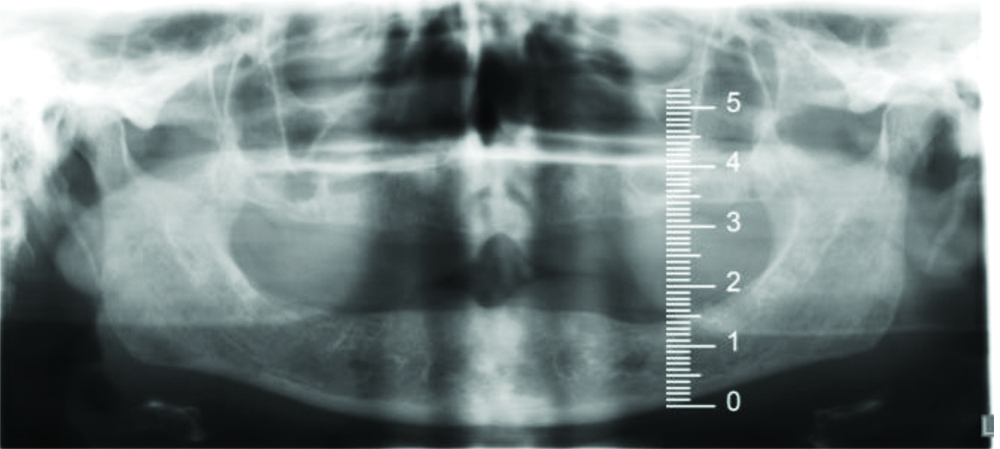
Type I (most favourable): Residual bone height ≥21 mm measured at the least vertical height of the mandible.
Type II: Residual bone height of 16-20 mm measured atleast vertical height of the mandible.
Type III: Residual alveolar bone height of 11-15 mm measured atleast vertical height of the mandible.
Type IV: Residual vertical bone height ≤10 mm measured atleast vertical height of the mandible.
2. Maxillary residual ridge morphology [Table/Fig-2] [2]
Maxillary residual ridge morphology (Type A).
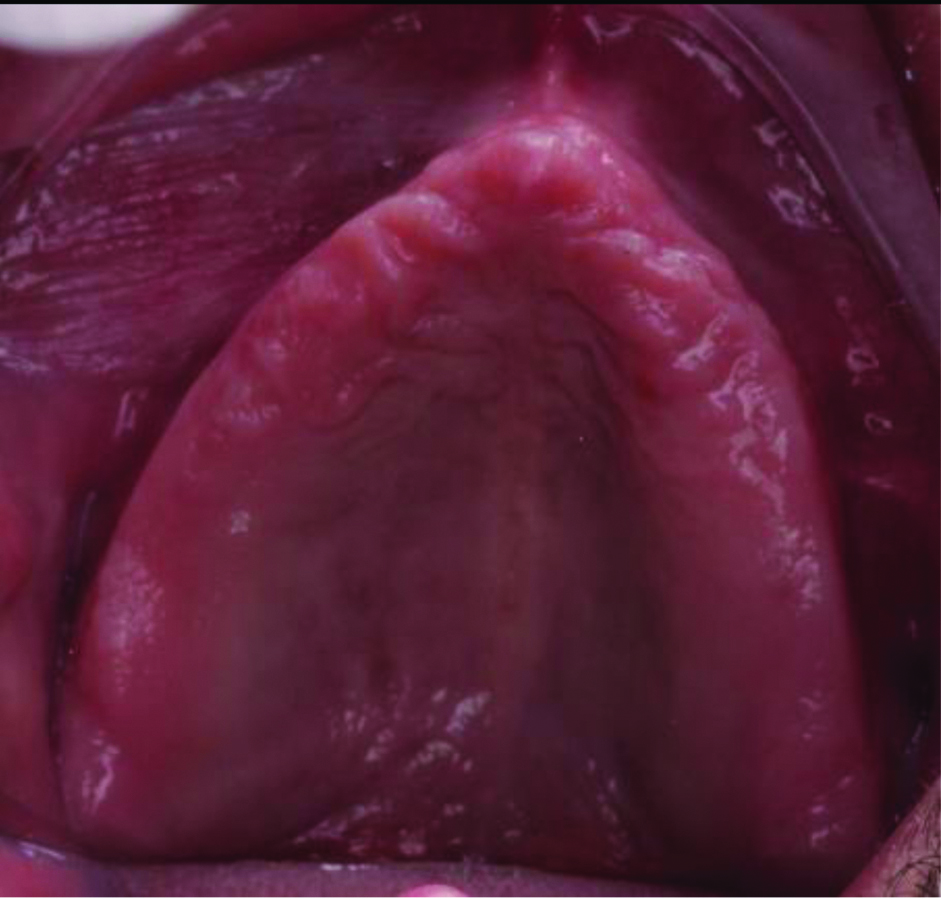
Type A (most favourable): Anterior labial and posterior buccal vestibular depth that resists vertical and horizontal movement of the denture base.
Type B: Loss of posterior buccal vestibule.
Type C: Loss of anterior labial vestibule.
Type D: Loss of anterior labial and posterior buccal vestibules.
3. Mandibular muscle attachment [Table/Fig-3] [2]
Mandibular muscle attachments (Type A).

Type A (most favourable): Attached mucosal base without undue muscular impingement during normal function in all regions.
Type B: Attached mucosal base in all regions except the labial Mentalis muscle attachment near the crest of the alveolar vestibule.
Type C: Attached mucosal base in all regions except anterior buccal and lingual vestibules-canine to canine.
Type D: Attached mucosal base only in the posterior lingual region.
Type E: No attached mucosa in any region.
4. Maxillomandibular relationship [Table/Fig-4] [2]
Maxillomandibular relationship (Class I).

Class I (most favourable): Tooth position that has normal articulation and teeth supported by the residual ridge.
Class II: Tooth position outside the normal ridge relation (excessive horizontal overlap).
Class III: Tooth position outside the normal ridge relation to attain aesthetics, phonetics, and articulation (cross-bite).
Other minor factors such as- tongue size, inter-arch space, cases that require pre-prosthetic surgery, and modifying factors (oral manifestation of systemic disease, psychosocial, temporomandibular disorders (TMD) symptoms, maxillofacial defects, ataxia, refractory patients, and history of paresthesia or dysesthesia) were also taken into consideration when classifying patients according to PDI [2,7].
Prosthodontic Diagnostic Index (PDI) classification system was built on the complete history, clinical examination, and systemic evaluation of each patient, based on four categories: Class I to Class IV [7].
Class I (ideal or minimally compromised): Patients who present ideal or minimally compromised complete edentulism and all four criteria are favourable.
Class II (moderately compromised): Patients who suffer from moderately compromised anatomic structures and constant physical dilapidation of the denture-supporting anatomy.
Class III (substantially compromised): Patients who have substantially compromised anatomic structures.
Class IV (severely compromised): Patients who come with the most weakened form of supporting anatomic structures where surgical reconstruction is typically designated, but cannot always be performed due to the patient’s health, desires, and past dental history.
One variable with a higher score is sufficient to classify the patient into a more complex (higher-level) group. This means the influence of each variable on the overall determination of class, and the final classification is determined by the variable with the highest level of complexity. For example, no matter how favourable the rest of the variables, a patient with 11-15 mm of mandibular residual bone height [Table/Fig-1] would be assigned to Class III (substantially compromised) [28].
An examination of the digital Orthopantomogram (OPG) of each patient was performed. Examiners were taught to record the height of the mandibular bone by measuring the least vertical height from the distance between the superior and inferior borders of the mandible by a scale, in millimeters [Table/Fig-1] [29]. Re-examination of all radiographs was performed to ensure intra-examiner reliability. Using the same reference points, measurements of the height of the mandibular bone were performed by two other examiners. Measurements of some of the radiographs by one examiner were re-recorded by another one to improve inter-examiner reliability [29].
The examiner classifies the morphology of the maxillary residual ridge, and then the category that is most descriptive of the mandibular muscle attachments is selected. Finally, the maxillomandibular relation was classified. The rest of the worksheet was then filled and the overall classification of the patient was performed according to the diagnostic findings and allotted to the students, teaching assistants, or specialists.
Statistical Analysis
The recorded data (counts and percentages) were compiled and entered into a spreadsheet (Microsoft Excel 2015).
Results
Out of 122 patients, most patients i.e., 51 (41.5%) in the study were in the age group of 51-60 years and 70 (57%) were male, and the majority were Saudi nationals 56 (45.9%). The results of the same are summarised in [Table/Fig-5,6 and 7].
Age-wise distribution of the sample (n=122).
| Age (years) | N | Percentage (%) |
|---|
| Less than 50 | 23 | 18.5% |
| 51-60 | 51 | 41.5% |
| 61-70 | 35 | 29% |
| 70 and above | 13 | 11% |
| Total | 122 | 100% |
Gender-wise distribution of the sample.
| Gender | N | Percentage (%) |
|---|
| Male | 70 | 57% |
| Female | 52 | 43% |
| Total | 122 | 100% |
Nationality-wise distribution of the sample.
| Nationality | N | Percentage (%) |
|---|
| Saudi | 56 | 45.9% |
| Indian | 13 | 10.7% |
| Pakistani | 12 | 9.8% |
| Sudani | 12 | 9.8% |
| Egyptian | 12 | 9.8% |
| Yemeni | 8 | 6.6% |
| Burmawi | 7 | 5.8% |
| Others | 2 | 1.6% |
| Total | 122 | 100% |
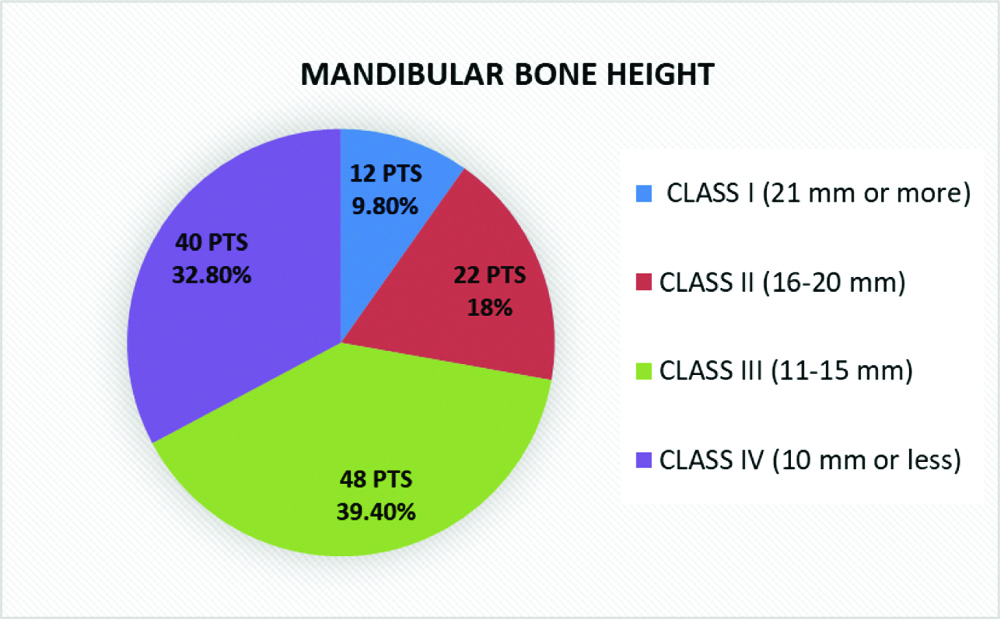
[Table/Fig-8] shows the first criteria for PDI, mandibular bone height. It was observed that the majority of 48 (39.4%) patients exhibited Class III, 40 (32.8%) exhibited Class IV, 22 (18%) Class II, and 12 (9.8%) Class I.
Mandibular bone height.
PTS: Patients
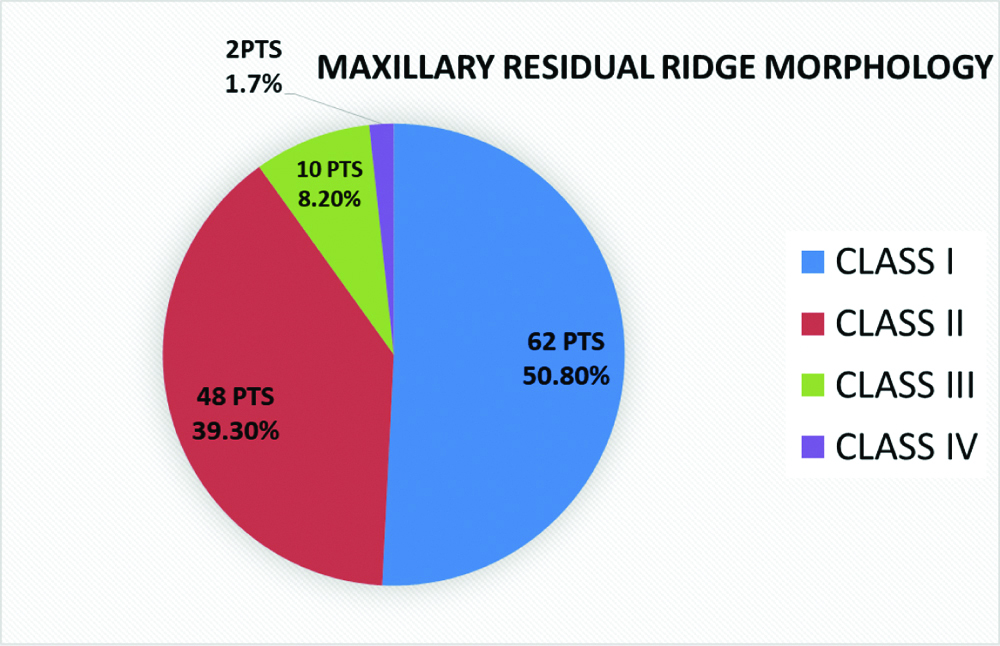
[Table/Fig-9] shows the morphology of maxillary residual ridge. The majority of 62 (50.8%) patients were classified as Class I and 48 (39.3%) were Class II. The least number of 10 (8.2%) patients were of Class III and two (1.7%) Class IV.
Maxillary residual ridge morphology.
PTS: Patients
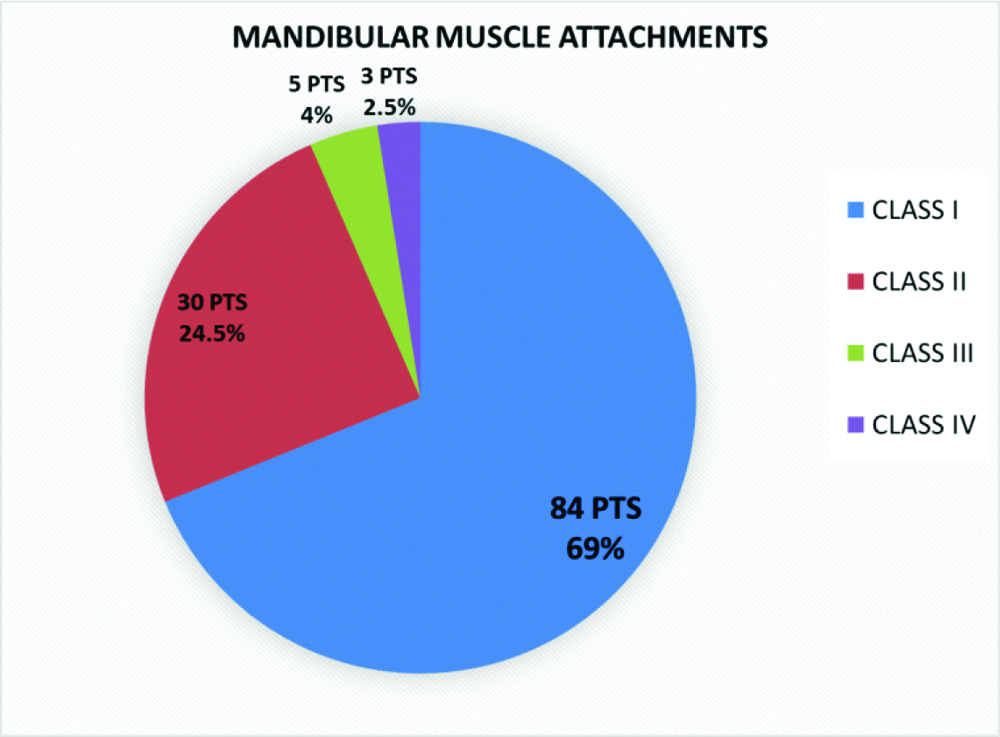
[Table/Fig-10] shows the muscle attachment of the mandibular arch. The maximum number of 70 (57.4%) patients belonging to Class I with adequate attached mucosa were Type A and 14 (11.5%) Type B (no attached buccal mucosa), 14 (11.5%) were of Type A, and 16 (13.1%) were Type B in Class II. Class III and IV comprised eight (6.5%) cases.
Mandibular muscle attachments.
PTS: Patients
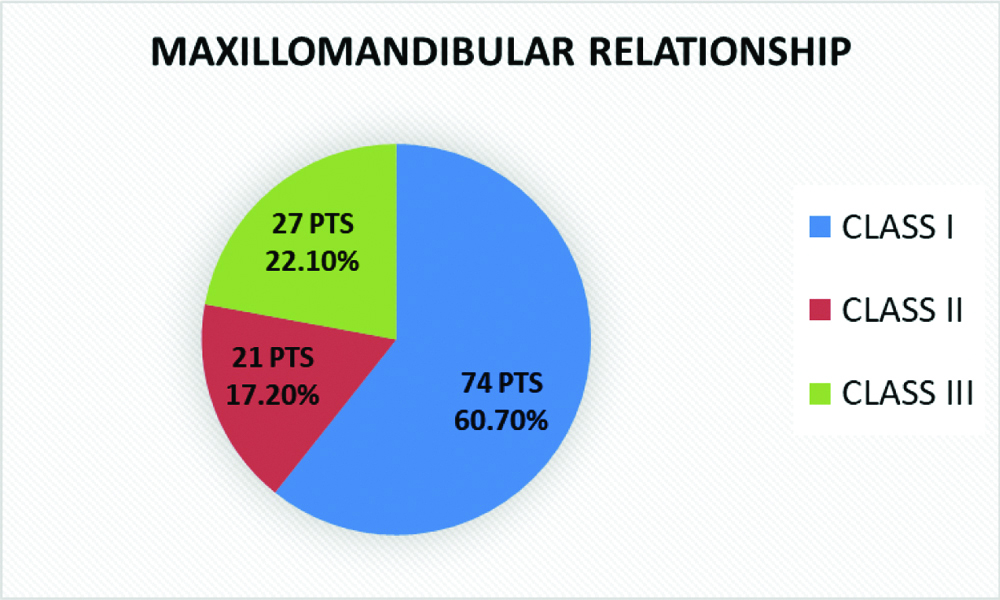
[Table/Fig-11] shows the maxillomandibular relationship. A majority 74 (60.7%) were Class I, 21 (17.2%) were Class II, and 27 (22.1%) were Class III.
Maxillomandibular relationship.
PTS: Patients
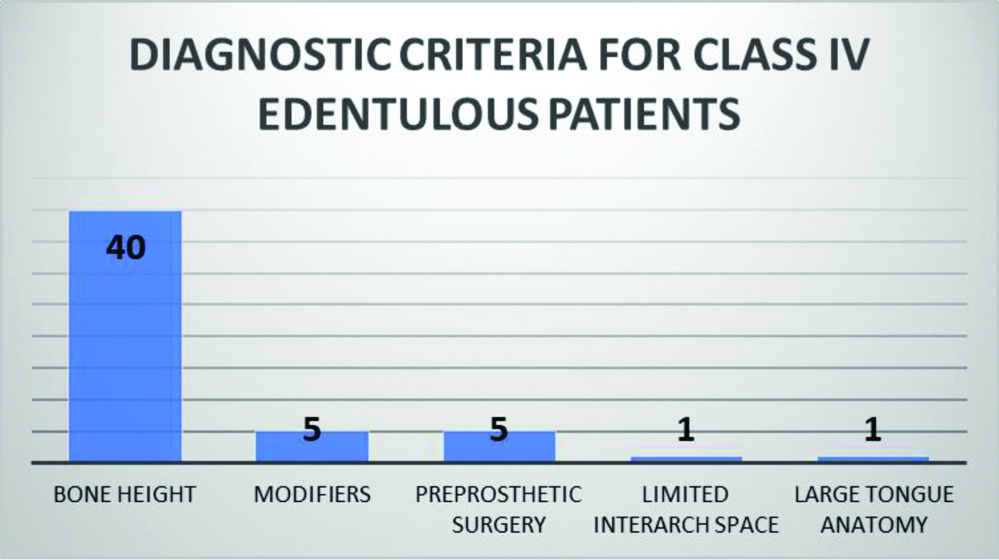
[Table/Fig-12] shows 52 patients who came under the complicated category of diagnostic criteria of Class IV. A 40 (76.9%) patients exhibited compromised bone height of less than 10 mm, five (9.6%) were refractory patients, who come under the category of modifiers, five (9.6%) required pre-prosthetic surgical procedures to improve the anatomy of maxillary and mandibular ridges, whereas one (1.9%) exhibited large tongue hindering denture stability and one (1.9%) had limited interarch space.
Diagnostic criteria for Class IV edentulous patients (52 patients).
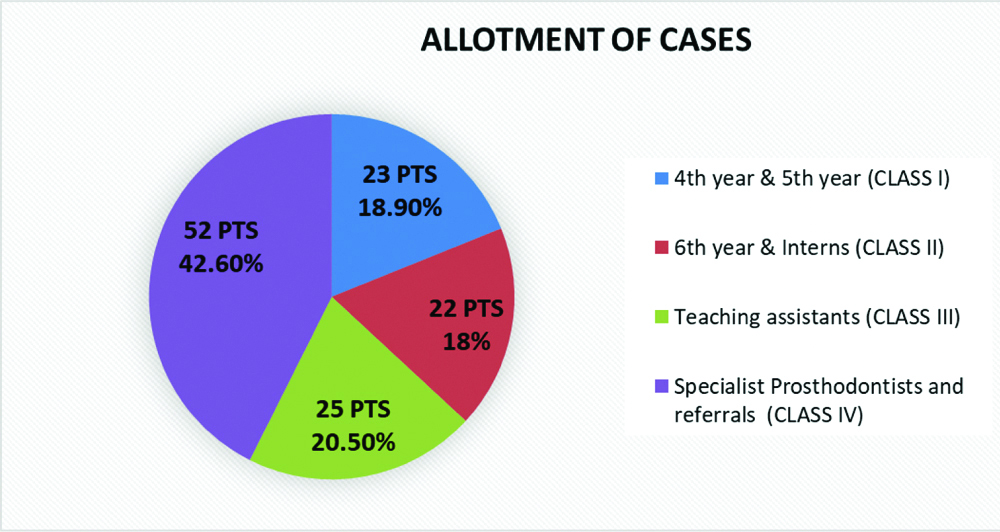
[Table/Fig-13] shows the overall classification of the PDI. The majority of 52 (42.6%) patients were of Class IV, 25 (20.5%) Class III, 23 (18.9%) Class I, and 22 (18%) Class II.
Overall PDI classification.
PTS: Patients
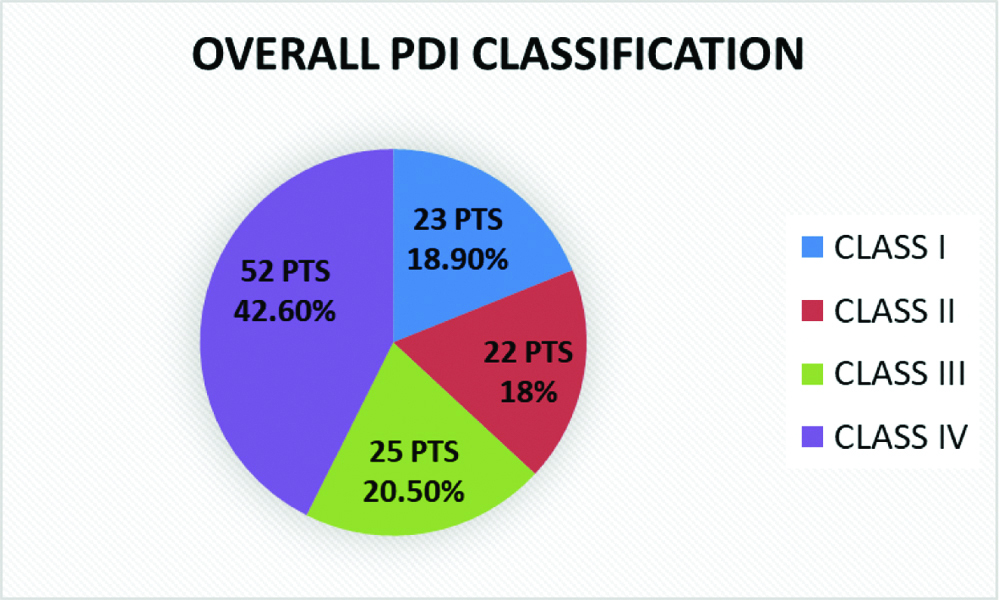
[Table/Fig-14] shows the allotment of cases according to the PDI. The majority of 52 (42.6%) patients were allotted to specialist prosthodontists or referred to specialist centers (Class IV), 25 (20.5%) were allotted to teaching assistants (Class III), 22 (18%) were allotted to 6th year and interns (Class II) and 23 (18.9%) were allotted to 4th and 5th year students (Class I).
Allotment of cases to students.
PTS: Patients
Discussion
The dental school where the study was conducted is located in an impoverished locality of Jeddah City; which is home to many expatriate communities from low socio-economic backgrounds and neglected oral health [30] who are completely edentulous. Therefore, the result is a myriad of nationalities with a large range of complex clinical conditions of edentulism based on each individual’s anatomy and modified by several other factors such as psychosocial problems and systematic disease, and the need for complete dentures [27,31]. Thus, there are a considerable number of patients available to undergraduate students for the training of complete dentures; similar to those reported in different countries [19-22,26,32].
The development of PDI by American College of Prosthodontists (ACP) is a boon to Prosthodontists who must perform diagnosis and treatment planning for all patients. The use of a standardised classification system such as PDI, offers many advantages in the treatment planning of edentulous patients [7]. The most important advantage of using PDI is the screening that can be performed in a dental school and provides an accurate classification of patients that can be used to allocate the treatment of the patients to the students, or referral to a specialist according to the complexity of the case [7].
In the study, authors found that the mandibular bone height as seen in OPG in the majority of patients was Class III (39.4%), but Shaik S et al., reported that the majority were in Class I (39.4%) [33], whereas Ntala PC et al., showed that the majority of patients were from Class IV (42.7%) [7]. No studies have compared the other three parameters such as maxillary residual ridge morphology, mandibular muscle attachments, and maxillomandibular relationships.
In our study, authors observed that 77 out of 122 (73%) patients were classified as complex (Class III and IV), were in the largest number, which is similar to studies conducted by Ntala PC et al., in Greece, 62 out of 110 patients (56.4%) [7], Mazurat RD and Mazurat NM in Canada, 49 out of 76 patients (64.5%) [28] and Elfadil S et al., in Ireland, 86 out of 125 patients (69%) [34]. Only Chaudary MAU et al., in Pakistan reported the majority in the Class I and II categories (57%) [27]. Mazurat RD and Mazurat NM reported that the most common factors for classifying the cases as the complex were the ridge height and muscle attachments in the mandibular arch [28], and authors found that the most common factor determining the complexity of the cases was mandibular ridge height which is similar to the study by Ntala PC et al., [7].
Undergraduate dentistry in Saudi Arabia is a seven-year course. In the third year, the students study preclinical course in removable prosthodontics. From the fourth year to the internship, students are required to make complete dentures as part of their requirements. Therefore, PDI Class I patients were allotted to the fourth and fifth year students and PDI Class II patients were allotted to the sixth year and interns. Teaching assistants were allotted PDI Class III and they treated these patients under the supervision of prosthodontic staff and since postgraduate students are not there, Prosthodontists treated some Class IV patients and some were referred to specialist centers since PDI Class IV patients were the highest in number. Our study is similar to Chaudary MAU et al., who allotted Class I to undergraduate students, Class II and Class III to postgraduate students, and Class IV were treated by specialists [27]. But Ntala PC et al., and Mazurat RD and Mazurat NM, were of the opinion that most of the complex Class III and IV could be treated by undergraduate students but under the strict supervision of specialists [7,28].
Thus, PDI should be used at an early stage in outpatient screening clinics. The collection of all data (radiographic, clinical, physical, and medical) and classification according to PDI will allow the suitable dispersal of patients, particularly those with an unfavourable prognosis [27]. Prosthodontists usually handle the management of complex cases such as Class IV, but Class III can be managed by postgraduate students under the supervision of staff members or special clinics/units [28].
Limitation(s)
The sample in the present study does not represent the entire population of Jeddah City in Saudi Arabia, as it included patients seeking treatment at Ibn Sina National College only. However, this study provides baseline data for further studies. There is a learning curve on using the PDI worksheet, especially for non-specialists so there has to be a specialist all the time when the edentulous patients were screened. Hence, it was decided to train students early during their undergraduate curriculum.
As the dental school where the study was conducted did not have postgraduate students and the referral hospitals had a long waiting period, the majority of the patients (Class IV) had to be treated by prosthodontists so that retreatment could be avoided and which put a lot of pressure on them as they were also involved in other teaching activities.
Conclusion(s)
The majority of the edentulous patients screened in the dental school using the PDI were categorised as Class IV, which is a complex category, therefore, the treatment had to be provided by the specialists. Thus, the PDI classification system can help to identify patients who are most likely to require treatment by a specialist. PDI provides a basis from which an accurate diagnosis can be obtained along with proper treatment planning. For easy and suitable networks between dental professionals, PDI has certain terminologies that help in establishing a proper channel of communication. These standardised indices can be useful for dental professionals during their private practice, as they allow better communication between specialists and dentists. In our dental school, authors have incorporated the PDI system and managed to screen, allot, treat, and refer completely edentulous patients based on the complexity successfully and continue to do so.