Introduction
COVID-19 has a wide range of symptoms ranging from asymptomatic infection to pneumonia which can progress to Acute Respiratory Distress Syndrome (ARDS), Multiple Organ Failure (MOF) and death [1]. A strong and durable immunity against COVID-19 is considered to be the basis of herd immunity that is expected to help in controlling the pandemic. At individual level, the immunity is considered protective and believed to prevent reinfection in the recovered patients. Data from UK showed that out of 11,000 healthcare workers who had proven evidence of infection during the first wave of the pandemic between March 2020 and April 2020, none had symptomatic reinfection in the second wave of the virus between October 2020 and November 2020 [2]. However, despite the proposed protective advantage of immunity, there have been cases of repeat infection with Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) which has questioned the significance of immunity conferred by the initial infection [3,4].
This phenomenon of repeat COVID-19 disease is now being considered a new threat to adequate control of the pandemic. There is scarcity of data on characteristic features of repeat COVID-19 as well as the factors that might predict or influence its occurrence. It is not known whether dynamic changes in the immunity after initial infections might play a role in the pathophysiology of the recurrent disease [5]. This article reports three patients who developed COVID-19, the second time, after their initial recovery from the first infection.
Case Series
Case 1
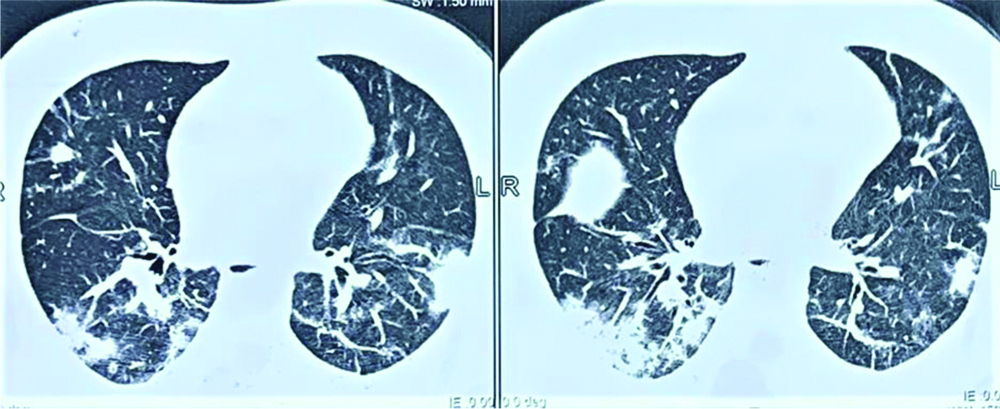
A 49-year-old male presented with fever and cough for 3 days. On examination, his vitals were stable with Oxygen Saturation (SpO2) of 97% at room air. Nasopharyngeal swab was tested for COVID-19 Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) which came out to be positive. On investigation, he had leucopenia (Total Leucocyte Count was 3.9/mm3) with increased neutrophil to lymphocyte ratio. Inflammatory markers at baseline were elevated with C-Reactive Protein (CRP) was 70.6 mg/dl, Interleukin-6 (IL-6) 152.7 pg/ml, ferritin was 601.1 ng/mL and Lactate Dehydrogenase (LDH) was 641 IU/L. Computed Tomography (CT) chest showed multiple ground glass opacities in bilateral upper and lower lobes with Cycle Threshold (CT) severity score of 8/25 [Table/Fig-1a] [6].
CT Chest done during first infection showing bilateral multifocal ground glass opacities and patchy consolidation.
In view of mild symptoms, patient was managed conservatively and advised home isolation as per guidelines issued by Government of India (GOI) [7]. Patient showed gradual improvement in his symptoms and recovered in two weeks with a negative RT-PCR report. He stayed at home and avoided contact with others even after recovery.
After about 3 weeks of recovery he again developed high grade fever, cough with haemoptysis and chest pain. His SpO2 was 96% at room air. Chest X-ray was done which showed patchy consolidation. Considering it to be bacterial pneumonia, patient was initially treated with oral antibiotics, but there was no improvement in symptoms. So, admission was planned and as per hospital protocol COVID-19 by RT-PCR was done which turned out to be positive.
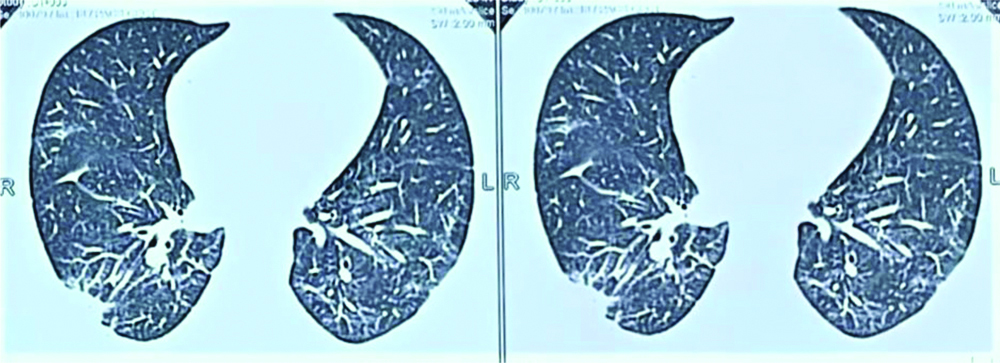
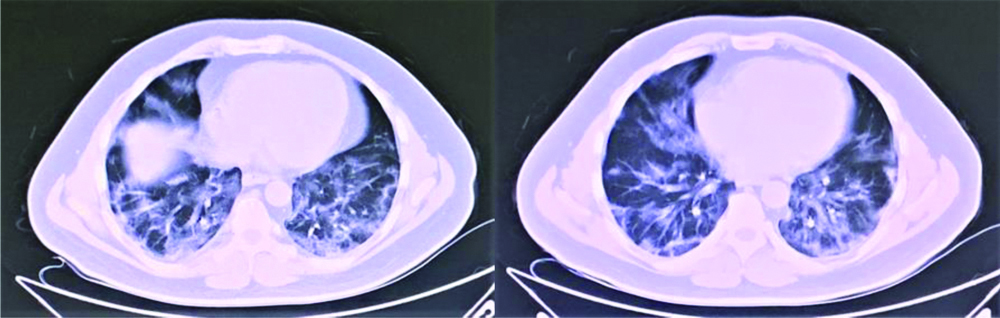
Inflammatory markers were found to be significantly raised. CRP was 296 mg/dL, ferritin was raised to 1447 ng/mL and IL-6 was 12.5 pg/mL. CT chest showed multifocal ground glass opacities in bilateral upper and lower lobes with CT severity score of 8/25 [Table/Fig-1b]. Because of worsening of oxygen saturation level, patient was managed with antiviral remdesevir (200 mg intravenous on day 1 followed by 100 mg once a day for 5 days), injection dexamethasone (6 mg intravenous BD for 5 days), oxygen therapy and supportive treatment. D-dimer levels were raised to 0.77. Despite high D-dimer levels, anticoagulants were not initiated as patient was having haemoptysis.
CT Chest done during repeat infection bilateral ground glass opacities and patchy consolidation bilateral lower lobe.
Patient showed improvement in fever and breathlessness. Inflammatory markers also showed an improving trend. He was discharged after ten days and advised further home isolation as per Government of India guidelines [7]. After 1 month of recovery IgG antibodies to nucleocapsid protein of SARS-CoV-2 were tested by Chemiluminescent Immunoassay (CLIA) and were found to be raised to 12.67 index (>1.4 is positive).
Case 2
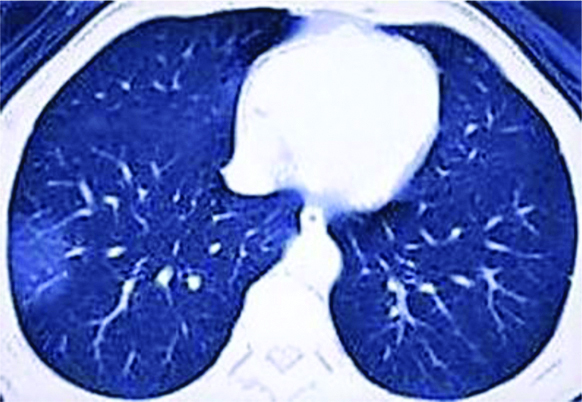
A 45-year-old male with no co-morbidities presented with fever, sore throat and cough for 4 days. On examination, SpO2 was observed to be 97% at room air. Nasopharyngeal swab was tested for COVID-19 by RT-PCR which came out to be positive. Inflammatory markers (CRP, IL-6, ferritin, D-dimer and LDH) were within normal limits. High Resolution Computed Tomography (HRCT) chest showed subtle subpleural patchy area of ground glass opacification in right lower lobe with CT severity score of 1/25 [Table/Fig-2a].
CT Chest done during first infection.
Patient was managed with vitamin C, zinc and symptomatic treatment with home isolation as per protocol [7]. There was improvement in his symptoms within a week. A week later, after full recovery, the patient joined his duty in his office and his job involved public dealing.
Two weeks after recovery patient got himself tested for antibodies against SARS-CoV-2 antigen which were found to be 0.01 index by CLIA. After two months patient again developed fever, cough and sore throat. On examination, patient was tachypneic with respiratory rate of 34. However, he was maintaining SpO2 of 97% at room air. Patient was tested for COVID-19 by RT-PCR which was found to be positive. CT chest showed ground glass opacities in peripheral part of both lungs (Left>Right) suggestive of interstitial pneumonitis with CT severity score of 7/25 [Table/Fig-2b]. Inflammatory markers such as CRP, IL-6, ferritin, D-dimer and LDH were significantly raised.
CT Chest done during repeat infection.
Patient was managed with injection ceftriaxone, injection dexamethasone and other supportive treatment. Patient showed improvement in fever and cough within a week and was discharged after 10 days.
Case 3
A 40-year-old male, a healthcare worker with no co-morbidities presented with complaints of high-grade fever, cough and myalgia for three days. His SpO2 at room air was 97%. Nasopharyngeal swab was taken and tested for COVID-19 RT-PCR which turned out to be positive. Chest radiograph showed infiltrates in left upper zone [Table/Fig-3a]. Patient was managed symptomatically and advised home isolation. There was improvement in his symptoms in five to 6 days. After 1 month of the symptom onset, Immunoglobulin G (IgG) antibodies to nucleocapsid protein of SARS-CoV-2 were tested and these were found to be raised to 10 index by CLIA.
a) Chest X ray during first infection; b) Chest X ray during repeat infection.
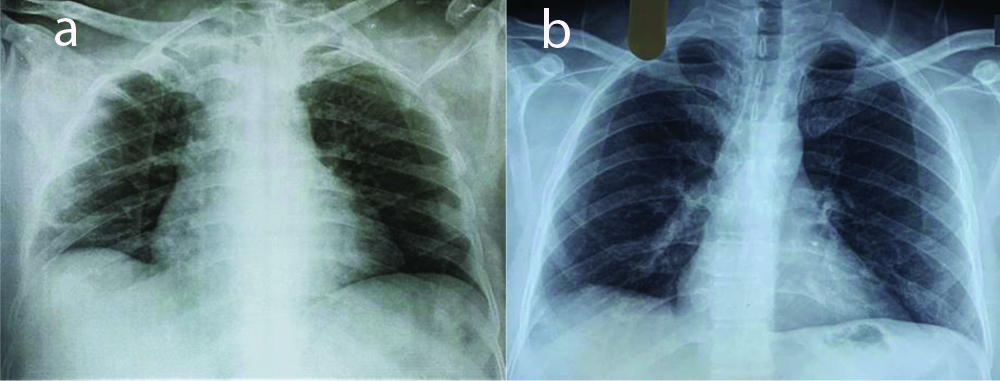
After four months patient again developed fever and sore throat. On examination, SpO2 was 98% at room air. Nasopharyngeal swab was positive for COVID-19. The severity of symptoms was milder during repeat infection. Chest radiograph was done which was normal [Table/Fig-3b]. Patient was managed with vitamin C, zinc and symptomatic treatment with home isolation as per protocol and he recovered in a week.
Discussion
Most coronaviruses confer a degree of immunity to reinfection [8]. But recently there were various reports of few people contracting COVID-19 for the second time [9-11]. Causes/risk factors for reinfection, time to development severity and final outcome are the few areas that need to be explored for better clarity on the topic.
Acquired immunity has been known to develop after COVID-19 as in case with other viral infections by humoral and cell-mediated immune responses [12]. The humoral response includes antibodies directed against S and N proteins. Antibodies-including Immunoglobulin M (IgM), Immunoglobulin G (IgG), and Immunoglobulin A (IgA)-against S and its subunits can be detected within 1-3 weeks after infection [13,14]. IgM and IgG antibodies can arise nearly simultaneously [14]; however, IgM and IgA antibodies decay more rapidly than IgG [13,15]. A study was conducted by public health England which suggested that antibodies provide 83% protection against COVID-19 reinfections over a five month period [16].
However, the intensity of immune response has been highly variable that might be dependent on severity of initial infection, immunocompetence of the host and time to recovery [17]. Compounding the issue, it is also hypothesised that instead of being protective, the SARS-CoV-2 antibodies generated after first infection may even enhance the entry/replication of virus into monocytes/macrophages and granulocytic cells, thus worsening the subsequent infection as in SARS-CoV infection [18,19]. This phenomena, known as Antibody Dependent Enhancement (ADE) may be catastrophic to control of COVID-19 as well as deter the vaccination drive against the virus.
Variable antibody responses as was seen after 1st and 2nd infection in the present series represent these complexities and uncertainties. In the present series, time to development of reinfection varied from 3 weeks to 4 months. In contrast, in a previous case series of 11 patients, the time interval between the two symptomatic episodes was less than 2 weeks. In another case series by Elzein F et al., the duration between the two episodes in the patients varied between 27 and 85 days [11]. Host factors, immunosuppressive therapy and viral dynamic can be the contributory factors. Importantly, the time gap between the two infections was not dependent on the severity of initial infection in any of the three patients in the present report. Even though, it is difficult to conclude any relationship from the three cases, but longer time duration between the two episodes as seen in two of our patients may point towards reinfection as the cause of 2nd episode.
Another question that needs to be answered is the severity of reinfection. It has been speculated that in most of the cases, the reinfection would be less severe because of a degree of immune memory and T-cell mediation [20]. In the present series, symptoms during reinfection were mild in 1st and 3rd case, whereas they were severe in the 2nd case. In another case series by Elzein F et al., all the four patients had mild infection in the first episode. However, three of them developed a severe disease during the second episode [11]. According to a review by British Society for Immunology, it has been observed that patients who experience mild symptoms in their initial infection or are immunosuppressed tend to have both a higher likelihood of reinfection as well as more chances of severe disease [21]. Advanced age particularly more than 60 years, hypertension, coronary artery disease, diabetes mellitus and other immunocompromised states like chronic kidney/liver/lung disease, obesity are high risk factors for severe disease [22]. However, in the present series; all patients were immunocompetent and had mild symptoms during their first infection. Hence, further studies are required to understand the predictors of severity of COVID-19 reinfection.
The other question which arises is that whether the repeat infection is reinfection or reactivation. This can be confirmed if one compares the genetic sequence of SARS-CoV-2 during initial and reinfection phase. The genomes from the two samples will be different if it is a reinfection. With the genetic sequence, one can also ascertain if it was the same variant or a different one. But genetic sequencing in itself is a huge task, due to scarce laboratory resources in this ongoing pandemic. A research conducted at the University of Oxford suggested that many of the cases of reinfection may actually be reactivation [23]. This is supported by the fact that the virus, due to its large genomic structures, can remain in the body at low levels to remain undetected but ready to strike once more. Persistent loss of smell and taste is possible evidence that the virus remains within the body, replicating at a low level for a long time [24]. On the other hand, a case report by Tillett RL et al., according to which a patient was infected by SARS-CoV-2 on two separate occasions by a genetically distinct virus, which suggests that the second episode was due to reinfection [10].
Another question is to differentiate reinfection from the prolonged viral shedding. Viral shedding via the respiratory has been detected up to 63 days after symptom onset. A study documented 41 severe cases of COVID-19 with a median viral shedding period of 31 days [25]. These are outliers as most individuals clear the virus in the first two weeks following symptom onset [26]. One factor that affects the duration of viral shedding is immunocompromised state such as in transplant recipients, who exhibit prolonged SARS-CoV-2 viral shedding [25]. According to the Centers for Disease Control and Prevention (CDC) guidance, a positive SARS-CoV-2 PCR test within 90 days of an initial infection may represent sustained viral shedding rather than reinfection [27]. Therefore, based on the guidance of the CDC, those who are asymptomatic during the 90-day period do not need to be retested for COVID-19. In case of prolonged viral shedding patient will generally be asymptomatic [28]. Thus, for previously infected individuals in this 90-day time frame who develop respiratory symptoms and without an alternative aetiology identified on evaluation, it would be reasonable to evaluate for SARS-CoV-2 reinfection [27].
There are several limitations in this case series. SARS-COV-2 virus was not isolated on culture and genotyping was not performed. However; the long interval between the first and second episode and the raised inflammatory markers point towards an active infection or reactivation than a prolonged viral shedding. A through research and analysis of cases is required to study the factors and mechanisms underlying reinfection and recurrences of COVID-19.
Conclusion(s)
Reinfection and/or reactivation with SARS-CoV-2 may hinder effective control of COVID-19 pandemic. The reinfection has a variable course and severity, but the prognosis seems to be better due to immunity to preceding infection. Further research is required to assess reinfection/ reactivation risk, its predisposing factors, clinical features and treatment options. Nevertheless, we should continue to take all the precautions like social distancing and wearing masks to prevent occurrence and transmission of this disease.
[1]. Alimohamadi Y, Sepandi M, Taghdir M, Hosamirudsari H, Determine the most common clinical symptoms in COVID-19 patients: A systematic review and meta-analysisJ Prev Med Hyg 2020 61(3):E304-12.Published 2020 Oct 610.18502/ijph.v49i7.357433083287 [Google Scholar] [CrossRef] [PubMed]
[2]. Stokel-Walker C, What we know about covid-19 reinfection so farBMJ 2021 372:n9910.1136/bmj.n9933468457 [Google Scholar] [CrossRef] [PubMed]
[3]. Madan M, Kunal S, COVID-19 reinfection or relapse: An intriguing dilemmaClin Rheumatol 2020 39(11):318910.1007/s10067-020-05427-332980985 [Google Scholar] [CrossRef] [PubMed]
[4]. Gousseff M, Penot P, Gallay L, Batisse D, Benech N, Bouiller K, Clinical recurrences of COVID-19 symptoms after recovery: Viral relapse, reinfection or inflammatory rebound?J Infect 2020 81(5):816-46.10.1016/j.jinf.2020.06.07332619697 [Google Scholar] [CrossRef] [PubMed]
[5]. Sekine T, Perez-Potti A, Rivera-Ballesteros O, Strålin K, Gorin JB, Olsson A, Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID-19Cell 2020 83(1):158-68.e14.10.1016/j.cell.2020.08.01732979941 [Google Scholar] [CrossRef] [PubMed]
[6]. Francone M, Iafrate F, Masci GM, Coco S, Cilia F, Manganaro L, Chest CT score in COVID-19 patients: Correlation with disease severity and short-term prognosisEuropean Radiology 2020 30(12):6808-17.10.1007/s00330-020-07033-y32623505 [Google Scholar] [CrossRef] [PubMed]
[7]. Government of India, Ministry of Health & Family Welfare. (2nd July, 2020). Revised guidelines for Home Isolation of very mild/pre-symptomatic/asymptomatic COVID-19 cases Retrieved from https://www.mohfw.gov.in/pdf/RevisedHomeIsolationGuidelines.pdf [Google Scholar]
[8]. Huang AT, Garcia-Carreras B, Hitchings MDT, Yang B, Katzelnick LC, Rattigan SM, A systematic review of antibody mediated immunity to coronaviruses: Kinetics, correlates of protection, and association with severityNat Commun 2020 11:470410.1038/s41467-020-18450-432943637 [Google Scholar] [CrossRef] [PubMed]
[9]. Adrielle Dos Santos L, Filho PGG, Silva AMF, Santos JVG, Santos DS, Aquino MM, Recurrent COVID-19 including evidence of reinfection and enhanced severity in thirty Brazilian healthcare workersJournal of Infection 2021 82:399-406.10.1016/j.jinf.2021.01.02033589297 [Google Scholar] [CrossRef] [PubMed]
[10]. Tillett RL, Sevinsky JR, Hartley PD, Kerwin H, Crawford N, Gorzalski A, Genomic evidence for reinfection with SARS-CoV-2: A case studyLancet Infect Dis 2020 21:52-58.10.1016/S1473-3099(20)30764-7 [Google Scholar] [CrossRef]
[11]. Elzein F, Ibrahim A, Alshahrani F, Mahrous M, Murshid E, Aldhehyan T, Reinfection, recurrence, or delayed presentation of COVID-19? Caseseries and review of the literatureJournal of Infection and Public Health 2021 14:474-77.10.1016/j.jiph.2021.01.00233743368 [Google Scholar] [CrossRef] [PubMed]
[12]. Lumley SF, O’Donnell D, Stoesser NE, Matthews PC, Howarth A, Hatch SB, Antibody status and incidence of SARS-CoV-2 infection in health care workersN Engl J Med 2021 384:533-40.10.1056/NEJMoa203454533369366 [Google Scholar] [CrossRef] [PubMed]
[13]. Qu J, Wu C, Li X, Zhang G, Jiang Z, Li X, Profile of immunoglobulin G and IgM antibodies against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)Clin Infect Dis 2020 71(16):2255-58.10.1093/cid/ciaa48932337590 [Google Scholar] [CrossRef] [PubMed]
[14]. Wolfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Muller MA, Virological assessment of hospitalized patients with COVID-2019Nature 2020 581(7809):465-69.10.1038/s41586-020-2196-x32235945 [Google Scholar] [CrossRef] [PubMed]
[15]. Iyer AS, Jones FK, Nodoushani A, Kelly M, Becker M, Slater D, Persistence and decay of human antibody responses to the receptor binding domain of SARS-CoV-2 spike protein in COVID-19 patientsSci Immunol 2020 5(52):eabe036710.1126/sciimmunol.abe036733033172 [Google Scholar] [CrossRef] [PubMed]
[16]. Wilkinson E, Covid-19 reinfection “rare” says NHS study but some may still pass the virus on, Pulse 2021 www.pulsetoday.co.uk/news/coronavirus/covid-19-reinfectionrare-says-nhs-studybut-some-may-still-pass-the-virus-on [Google Scholar]
[17]. Pulendran B, Li S, Nakaya HI, Systems vaccinologyImmunity 2010 33:516-29.10.1016/j.immuni.2010.10.00621029962 [Google Scholar] [CrossRef] [PubMed]
[18]. Peiris JS, Chu CM, Cheng VC, Chan KS, Hung IF, Poon LL, Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: A prospective studyLancet 2003 361:1767-72.10.1016/S0140-6736(03)13412-5 [Google Scholar] [CrossRef]
[19]. Halstead SB, Dengue hemorrhagic fever: Two infections and antibody dependent enhancement, a brief history and personal memoirRev Cubana Med Trop 2002 54:171-79. [Google Scholar]
[20]. Dan JM, Mateus J, Kato Y, Hastie KM, Yu ED, Faliti CE, Immunological memory to SARS-CoV-2 assessed for up to eight months after infectionScience 2021 371(6529):eabf406310.1126/science.abf406333408181 [Google Scholar] [CrossRef] [PubMed]
[21]. BSI 2020. The ageing immune system and COVID-19. British Society for Immunology. published 10 November 2020 [Google Scholar]
[22]. Hu J, Wang Y, The clinical characteristics and risk factors of severe COVID-19Gerontology 2021 :01-12.10.1159/00051340033406518 [Google Scholar] [CrossRef] [PubMed]
[23]. Simmonds P, Williams S, Harvala H, Understanding the outcomes of COVID-19-does the current model of an acute respiratory infection really fit?J Gen Virol 2020 10.1099/jgv.0.00154533331810 [Google Scholar] [CrossRef] [PubMed]
[24]. Sun J, Xiao J, Sun R, Tang X, Liang C, Lin H, Prolonged persistence of SARS-CoV-2 RNA in body fluidsEmerging Infectious Diseases 2020 26(8):1834-38.10.3201/eid2608.20109732383638 [Google Scholar] [CrossRef] [PubMed]
[25]. Widders A, Broom A, Broom J, SARS-CoV-2: The viral shedding vs infectivity dilemmaInfect Dis Health 2020 25:210-15.10.1016/j.idh.2020.05.00232473952 [Google Scholar] [CrossRef] [PubMed]
[26]. He X, EHY L, Wu P, Temporal dynamics in viral shedding and transmissibility of COVID-19 [published correction appears in Nat Med. 2020;26(9):1491-93]Nat Med 2020 26:672-75.10.1038/s41591-020-0869-532296168 [Google Scholar] [CrossRef] [PubMed]
[27]. Centers for Disease Control and Prevention. Duration of isolation and precautions for adults with COVID-19, August 16, 2020 [Google Scholar]
[28]. Tuan J, Spichler-Moffarah A, Ogbuagu OA, New positive SARS-CoV-2 test months after severe COVID-19 illness: Reinfection or intermittent viral shedding?BMJ Case Reports CP 2021 14:e24053110.1136/bcr-2020-24053133542020 [Google Scholar] [CrossRef] [PubMed]