Supracondylar Humerus Fracture (SCHF) is common in paediatric age group and constitute majority of the elbow fractures [1,2]. According to the direction of distal fragment, SCHFs in children is divided into extension type and flexion type. Gartland’s classification is used to describe this fracture based on displacement in coronal plane radiographs and are of three types [2]. Type I are treated conservatively with an above-elbow plaster cast for three weeks with radiographs to look for displacements [3]. Type II and Type III usually go for malunion if treated with cast hence, they are treated with closed reduction and pinning [3]. Completely displaced supracondylar humeral fractures in children can present with brachial artery injury [4,5] and nerve injury in 20% of cases.
Percutaneous K-wire pinning techniques have become the preffered treatment in most of the supracondylar fractures because of difficulty in closed reduction and maintaining the reduction [6]. The commonly used pinning configurations are crossed pinning and only lateral pinning. A crossed pin configuration provides increased stability which is not the case with lateral pin fixation, while the disadvantage is ulnar nerve injury with the former that can be avoided with the latter [7-10].
Lateral only fixation is good enough for maintaining reduction while simultaneously avoiding injury to the ulnar nerve [11] but biomechanically less stable if not used in the proper configuration. The choice of pinning configuration is a surgeon’s preference, as both configuration have their advantages and disadvantages.
This retrospective study was performed to find the advantages and safety of percutaneous pinning techniques with respect to functional and radiological outcome in the management of displaced supracondylar humerus fractures in children; and to note the associated complications with this method of fixation.
Materials and Methods
This was a retrospective study, performed on patients admitted to Department of Orthopaedics, Hassan Institute of Medical Sciences, Hassan, between January 2017 to December 2019. This study was approved by Institutional Ethical Committee {IEC-RR107/2019 (18-10-19)}.
Inclusion criteria:
Age 3-15 years
Gartland Type II and Type III fractures
Closed fractures
Fresh cases of fracture (within one week)
Exclusion criteria:
Associated other injuries at elbow
Malunited fractures
Floating elbow
Patients with inadequate follow-up and incomplete records
The patients with acute presentation to emergency department or outpatient department were admitted. As per protocol, primary splintage is done after assessing distal neuro-vascular status and patient sent for radiography. The study involved collecting data regarding the age of the patient, time to surgery from injury and duration of surgery using past records. Radiographs (anterior-posterior and lateral views) were reviewed to determine the type of Gartland fracture.
Radiographs were also used to determine the type of wire configuration used. All patients who were available for follow-up till 12 weeks with records were reviewed and 30 patients were included in the study. Postoperative complications along with their management were also noted. Union of fracture was assessed by absence of pain on movements and abnormal mobility clinically and radiological by adequate callus formation. The functional outcomes were assessed as per Flynn criteria [Table/Fig-1] [7].
| Result | Carrying angle loss (Degrees) | Functional factor motion loss (Degrees) |
|---|
| Excellent | 0-5 | 0-5 |
| Good | 6-10 | 6-10 |
| Fair | 11-15 | 11-15 |
| Poor | >15 | >15 |
Statistical Analysis
Statistical analysis was done using IBM Statistical Package for the Social Science (SPSS) software package for windows.
Results
The study incuded 30 patients, of which 21 were males and 9 were females. The age of patients were in the range 4-12 years with a mean age of 7.4 years; 22 (73.3%) patients had left sided fracture and 8 (26.7%) patients had fracture on right side [Table/Fig-2].
Age distribution of the study subjects.
| Age (Years) | No. of patients | Percentage |
|---|
| 4-6 | 12 | 40 |
| 7-9 | 8 | 26.7 |
| 10-12 | 10 | 33.3 |
Most (90%) of the injuries were the result of trauma including fall. Out of the 30 cases, nine patients had Type II fracture and 21 of them had Type III fracture [Table/Fig-3]. Out of 30 patients, three had nerve injury due to fracture. Median nerve injury in 2 patients, radial nerve injury in 1 patient. All these nerve injuries did not require any separate surgical procedure as they recovered completely after fracture fixation within 6-12 weeks (mean 10 weeks). This was clinically assessed on follow-up by return of motor and sensory deficits but at the end of 12 weeks all had satisfactory results.
Gartlands classification.
| Type of fracture | No. of patients | Cross pinning | Lateral-only pinning | Mean time for maximum ROM | Mean time for Union±SD |
|---|
| Type II | 9 (30%) | 4 (13.3%) | 5 (16.6%) | 8 weeks | 4.1 weeks |
| Type III | 21 (70%) | 17 (56.6%) | 4 (13.3%) | 12 weeks | 4.5 weeks |
| Total | 30 | 21 (70%) | 9 (30%) | | 4.2±0.7 weeks |
ROM: Range of motion
There was one patient with absent radial pulse and grossly displaced supracondylar fracture but well perfused. This patient was managed on an urgent basis with closed reduction and fixation of the fracture. The radial pulse was palpable after reduction. Out of 30 patients, associated fracture of ipsilateral distal radius and ulna was seen in 3 patients.
In this study, patients with both pin configuration were included cross K-wire was in 21 patients and lateral-only pin in nine patients. Of the 21 patients, who had type III fracture, 4 were treated with lateral only K-wire pinning and 17 were treated with crossed K-wire pinning configuration [Table/Fig-3,4].
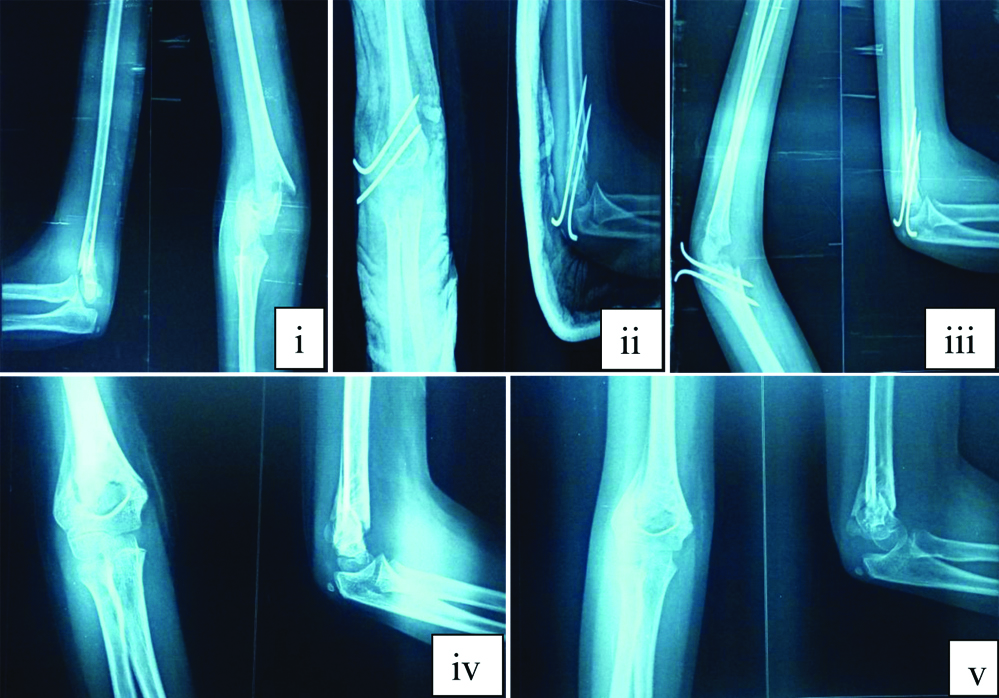
Shows x-ray of patient at follow-up (i) Preoperative; (ii) Postoperative; (iii) Three weeks postoperative; (iv) Six weeks postoperative; and (v) 12 weeks postoperative.
Superficial pin tract infection was most common postoperative complication, observed in 4 (13.3%) patients after a mean time 12 weeks of follow-up. This was treated with removal of pin, oral antibiotics and daily cleaning and dressing, without any need for hospitalisation. All wounds healed well after removal of pins. Ulnar nerve injury was observed in 1 patient immediately after surgery due to medial K-wire. This recovered after removal of medial pin in 6 weeks. Stiffness of elbow was seen in 3 (10%) patients. Cubitus varus deformity was observed in 1 patient with cross pinning, and loosening of K-wire was seen in 1 patient [Table/Fig-5].
Postoperative complications.
| Complications | Number of patients (%) | Cross pinning | Lateral-only pinning |
|---|
| Superficial pin tract infection | 4 (13.3%) | 3 | 1 |
| Restriction of movements | 3 (10%) | 1 | 2 |
| Iatrogenic ulnar nerve palsy | 1 (3.3%) | 1 | 0 |
| Implant loosening | 1 (3.3%) | 1 | 0 |
| Cubitus varus | 1 (3.3%) | 0 | 1 |
The average time for maximum range of movement recovery was eight weeks for type II fracture and 12 weeks for type III fractures (excluding patients with fixed flexion deformity).
Functional outcome was analysed according to Flynn’s criteria. Out of 30 patients included in the study, 25 patients (83.3%) had excellent outcome, 3 (10%) patients had good, 1 (3.3%) had fair and 1 (3.3%) patients had poor functional outcome [Table/Fig-6]. The patients with unsatisfactory results were advised active physiotherapy and reassured. Majority in the cross pin group showed excellent outcome, compared to lateral-only pin.
Functional results based on Flynn’s Grading System.
| Results | Number of patients | Cross pinning | Lateral-only pinning |
|---|
| Excellent | 25 (83.3%) | 19 (90.4%) | 6 (66.6%) |
| Good | 3 (10%) | 1 (4.7%) | 2 (22.2%) |
| Fair | 1 (3.3%) | 1 (4.7%) | 0 |
| Poor | 1 (3.3%) | 0 | 1 (11.1%) |
Discussion
The supracondylar humerus fractures is most commonly seen in children between 5 and 10 years of age. In the present study, the mean age was 7.4 years, which is similar to other studies [12,13]. Supracondylar humerus fracture has higher incidence in males [12,14]. In the present study also had higher incidence in male patients, 21 (70%) male and 9 (30%) female. Most common mode of injury is by fall on outstretched hand in supracondylar fractures [15]. In the present study, 27 (90%) had fall while playing, which is similar to other studies [16,17].
The non-dominant extremity is most commonly affected. In the present study, 22 (73.3%) had left-sided injury and 8 (26.7%) of them had right-sided injury. The findings are reflected in other studies too that show a preponderance of left-sided fractures [12,14,16].
These fractures are mostly caused by low energy trauma and are categorised on the basis of injury pattern, which are extension and flexion types, respectively. Injury caused by extension occurs due to fall on the palm of hand with hyperextended elbow (most common), while direct fall onto fixed elbow results in flexion type of these injuries [18]. In the present study, based on the Gartland’s classification, majority had type III fracture (70%) and were of extension type (93.3%).
Controversy persists regarding the optimal pin fixation technique. Commonly used techniques are lateral only pin and cross pinning with one medial and lateral k-wire [19]. Cross pinning configuration with medial pin involved iatrogenic ulnar nerve injury with incidence rate of 0-6% [20]. Lateral pinning technique was observed to have loss of reduction and cubitus varus in 3-5% of patients [20]. Some authors found crossed (medial/lateral) pinning to be superior than two parallel lateral pin fixations [21,22]. However, Reynolds RA and Jackson H, have observed in their study that both type of pin configurations have good outcome in the management of displaced supracondylar humerus fractures in children [23].
In the present study, out of the 30 cases, 21 of them were treated with cross K-wire pinning, 9 of them with lateral only pinning. Out of the 21 patients, who had type III fracture, 4 of them underwent lateral K-wire pinning and 17 underwent crossed K-wire crossed pinning configuration. Supracondylar humerus fractures in children treated commonly with crossed K-wire fixation and is the preffered configuration. Weinberg AM et al., observed in their study that biomechanically crossed K-wires showed more stiffnes and least loss of reduction on cyclic loading. The external fixators fixation good alternatives [24]. Zionts LE et al., [25] on comparison between crossed K-wire technique with lateral K-wire fixation, found great stability in cross pinning technique. But the authors did not give any clear advantage to lateral technique alone as there were less number of participants in the study.
According to a study, the functional outcome in cross pinning group was excellent in 66.7% and good outcome in 33.3% of patients, and lateral pinning group had 73.3% excellent results and 26.6% good results with no poor results [26]. There was no significant difference in functional outcome between the two groups. This is comparable to present study in which, out of the total 30 cases, 21 (70%) treated with crossed K-wire crossed pinning cases 19 (66.3%) showed excellent results.
Wang YL in their study found mean time to restore elbow range of motion (ROM) recovery after removal of long arm cast without physical therapy in uncomplicated distal humerus supracondylar and lateral condylar fractures was 5 weeks [27]. In the present study, the mean time for maximum range of movement recovery was 8 weeks for type II fracture and 12 weeks for type III fractures.
Govindasamy R et al., in a retrospective study on cross pinning versus lateral pinning in supracondylar fracture in children and concluded that there was no difference in stability of fixation and both groups had similar outcome functionally and cosmetically [28]. They noticed iatrogenic ulnar nerve injury in 11% of patients in cross pinning group due to medial pin and hence concluded that lateral pinning technique is safer than cross pinning technique. In present study also, 1 case of iatrogenic ulnar nerve injury was noted in cross pinning technique which recovered after K-wire removal.
Pin tract infection occurred in 4 patients (13.3%) in the present study which is comparable with study by Mostafavi HR and Spero C, having 5% incidence of infection around pins [29]. Shannon FJ studied 20 children and found an infection rate of 5%, and granulation tissues were reported in five children out of 20 with no varus deformity [30]. El-Adl WA et al., showed an infection rate and varus deformity of the elbow joint in 8.6% of their patients [31]. In 2011, Dua A et al., showed that in their series of 40 children superficial pin-tract infection rate was 7.5%, with no varus deformity, and a total success rate within 90% [32].
In the present study of 30 cases, the clinical outcome grading was measured as per the Flynn JC et al., criteria for grading outcomes; 25 (83.3%) of the patients observed excellent results. Almohrij SA compared casting and percutaneus pinning in treatment of displaced supracondylar fracture of humerus and concluded percutaneus pinning is a preferable method because it shortens hospitalization time, the elbow can be splinted in a safe and comfortable position, and decrease the risk of compartment syndrome [33].
Skaggs DL et al., studied consequences of pin placement in operative treatment of supracondylar fracture of humerus in children and concluded that lateral pinning is safe and effective for displaced supracondylar fractures; moreover it prevents iatrogenic injury to the ulnar nerve. They also mention that if medial pin is to be used in cross pinning then hyperflexion of elbow is avoided during inserting medial pin [34].
Limitation(s)
The present study has limitations as it is a retrospective study. There was no statistical comparison between cross pin and lateral-only pin configurations and also at the number of K-wires used in lateral only pinning or sizes of K-wire. There are studies showing more stability with three lateral wires than two lateral wires [35,36], and more stability with thicker (1.6 mm) wires [37,38]. Also, a small sample size prevents to come to a significant conclusion on outcomes.
Conclusion(s)
The present study concludes that displaced supracondylar fracture of humerus in children can be managed safely and effectively with closed reduction and percutaneous K-wire pinning. It was also found that both lateral pinning and cross pinning are safe and effective to get excellent outcomes in supracondylar fracture of humerus in children but lateral pinning is comparatively safe and reliable considering ulnar nerve injury which is more commonly associated with cross pinning. With both techniques, good functional outcome related to early mobilisation of the elbow with a very few complications can be achieved. Displaced supracondylar fractures of the humerus in children treated with closed reduction and percutaneous pin fixation gives excellent functional and cosmetic results.
ROM: Range of motion