A Randomised Clinical Trial to Compare the Efficacy of Tramadol and Nalbuphine for Treatment of Shivering after Spinal Anaesthesia in Patients Posted for Lower Limb Orthopaedic Surgery
Sara Mary Thomas1, Ananya Pradhan2, Dinesh Chauhan3
1 Associate Professor, Department of Anaesthesia, Smt. BK Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Piparia, Vadodara, Gujarat, India.
2 MD Resident, Department of Anaesthesia, Smt. BK Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Piparia, Vadodara, Gujarat, India.
3 Professor and Head, Department of Anaesthesia, Smt. BK Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Piparia, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dinesh Chauhan, Professor and Head, Department of Anaesthesiology, SBKS MIRC, Dhiraj Hospital, At & PO Piparia, Waghodia, Vadodara-391760, Gujarat, India.
E-mail: drdinesh77@gmail.com
Introduction
Shivering is a frequent complication after regional anaesthesia and the primary cause of shivering is perioperative hypothermia. Nalbuphine and tramadol are opioids which have been used to control postanaesthetic shivering.
Aim
To compare the efficacy of nalbuphine and tramadol in the treatment of postspinal anaesthesia shivering.
Materials and Methods
This was a randomised clinical trial conducted on 60 patients of either gender (20-60 years age group) from January 2019 to June 2020, American Society of Anaesthesiologists (ASA) Grade I or II, having postspinal anaesthesia shivering. The total sample was divided into two groups of 30 patients each. Group T received injection inj. tramadol 1 mg/kg intravenously (IV) and Group N received Inj. nalbuphine 0.1 mg/kg IV. Grade of shivering was assessed with a five point scale. The time taken for disappearance of shivering, assessment of improvement of shivering (complete- if grade of shivering becomes 0, partial- if grade of shivering deceased but not zero), recurrence rate and side-effects such as nausea, vomiting, deep sedation were noted. Independent t-test and Chi-square test were used to analyse the data. A p-value <0.05 were considered statistically significant.
Results
The time taken for disappearance of shivering was shorter in group N than T (3.20±0.96 minutes and 6.43±0.97 minutes respectively, p=0.001). Significantly better sedation (p-value 0.04) was seen in nalbuphine group as grade 3 sedation were seen in 15 patients of nalbuphine group as compared to none in tramadol group. All the patients in group N had complete improvement of shivering and there was no recurrence, while in group T six patients had partial improvement in shivering and four (13%) had recurrence. Complications such as nausea (three patients) and vomiting (one patient) were seen in Group T while none were seen in Group N.
Conclusion
The efficacy of nalbuphine is greater than tramadol in controlling postspinal anaesthesia shivering, with minimal side-effects.
Anti-shivering effect, Opioids, Sedation, Subarachnoid block
Introduction
Shivering is a frequent complication after regional anaesthesia and is reported in 40% to 70% of cases [1]. The primary cause of shivering is perioperative hypothermia [2]. Hypothermia in regional anaesthesia results from redistribution of body heat from the core to the periphery and patients who are given central neuraxial block have difficulty in re-establishing core temperature equilibrium as peripheral vasoconstriction remains impaired and there is inhibition of thermoregulatory mechanism [2-4].
Shivering increases oxygen consumption by 200-500% along with a rise in carbon dioxide production which is detrimental in patients with limited myocardial oxygen reserve or coronary disease as it further compromise myocardial function [5-7]. Shivering is associated with substantial adrenergic activation and discomfort [8]. It also results in increased metabolic rate, delayed wound healing, arterial hypoxemia, lactic acidosis, increased intraocular, intracranial pressure and interferes with pulse rate, blood pressure and electrocardiographic monitoring [3,9,10].
Tramadol is one of the drugs which is used in the treatment of postspinal anaesthesia shivering. It is a synthetic opioid with its predominant effect on μ receptor with minimal effects on kappa or delta binding sites [11]. It also inhibits the reuptake of norepinephrine and serotonin, hence activating the descending inhibitory spinal pathways [11,12]. Dhimar AA et al., explored the efficacy and potency of tramadol in comparison to pethidine for control of shivering under regional anaesthesia. It was found that both tramadol and pethidine were efficacious, but tramadol was more potent with respect to control of shivering and its recurrence [13].
Nalbuphine a semisynthetic opioid is also used for controlling postspinal shivering. It has μ antagonist and k-agonist activities and data suggests that k-opioid receptors may play a more important role than μ opioid receptors in the treatment of postanaesthetic shivering. This explains the anti-shivering properties of nalbuphine as it has a high affinity for k-opioid receptors in the central nervous system [14-16]. Chowdhury MS et al., compared nalbuphine (5 mg IV) and pethidine (25 mg IV) in the treatment of postspinal anaesthesia shivering and concluded that nalbuphine was more potent than pethidine as it took shorter time to control shivering and there was no recurrence of shivering [17].
Tramadol, even though is an effective drug in the treatment of shivering under regional anaesthesia [13], was found to have high incidence of side-effects like nausea, vomiting and dizziness [18]. Thus, there was a need to search for a drug which is as efficacious as tramadol but with fewer side-effects. Nalbuphine was thought as a viable alternative to tramadol and review of literature showed few studies comparing both drugs for this indication. So, this study was undertaken with the primary objective to compare the efficacy of nalbuphine and tramadol in the treatment of postspinal shivering. The secondary objective of this study was to evaluate the haemodynamic profile and side-effects of these drugs.
Materials and Methods
This randomised clinical study was conducted in Dhiraj Medical Hospital, Piparia, Gujarat, India from January 2019 to June 2020, after obtaining permission of the Institutional Ethics Committee (no- SVIEC/IN/MEDI/BNPG19/D20073) and patients’ written informed consent.
Inclusion criteria: Sixty patients belonging to ASA grade l and II of either gender aged 20 to 60 years undergoing spinal anaesthesia for elective lower limb surgeries and those which developed shivering grade 1 or more [19] during the study time period were enrolled in this study after taking informed consent.
Exclusion criteria: Patients with history of allergy to tramadol or nalbuphine, having cardiovascular diseases, hyperthyroidism, psychological disorder, uncontrolled diabetes or autonomic neuropathies, having history of alcohol or substance abuse were excluded from the study.
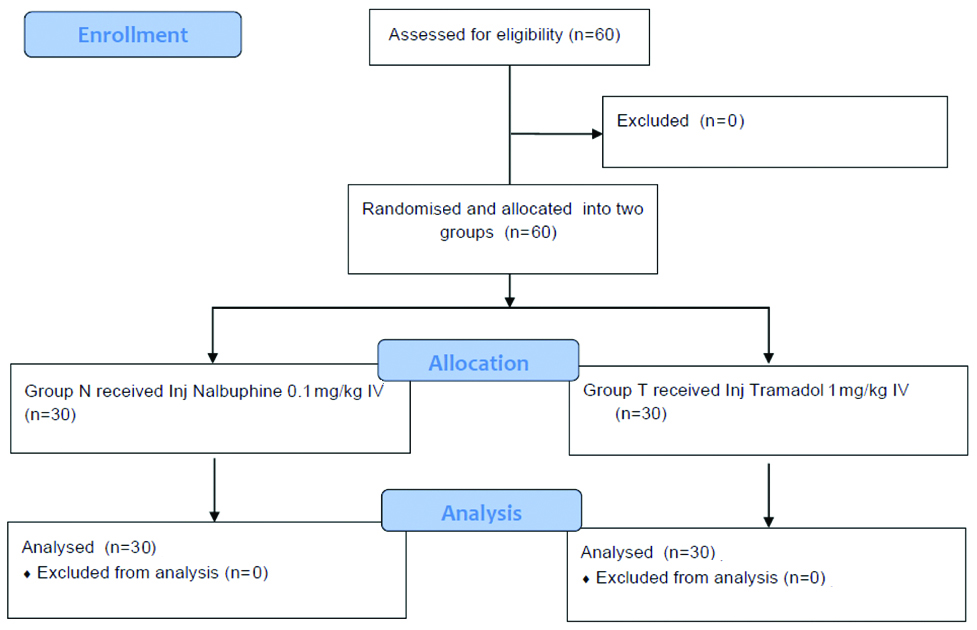
The CONSORT diagram is shown in [Table/Fig-1].
Sample size calculation: Sample size was calculated on the basis of previous studies. Incidence of shivering recurrence was 45-60% and taking into consideration an α error of 0.05 and power of the study of 80%, the number of patients required in each group was calculated as 30 [20-22].
In the Operation Room (OR), intravenous (IV) access was secured and all standard ASA monitors were attached including body temperature (axillary). Heart Rate (HR), Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Oxygen Saturation (SpO2), temperature were recorded at baseline, every 2 minutes till 5 minutes then every 5 minutes till half an hour, thereafter every 30 minutes till completion of surgery. Under aseptic precautions, spinal anaesthesia was given in L3-L4 interspinous space with 15-18 mg of 0.5% hyperbaric bupivacaine using a 25-gauge Quincke spinal needle and blockage upto T10 dermatome was achieved. A single layer surgical draping was used to cover all the patients and the ambient temperature of OR was maintained constant (24-26°C). All the patients were observed for shivering, and was graded with a five point scale as per Crossly and Mahajan in study of Shukla U et al., [Table/Fig-2] [18].
| Grades of shivering |
|---|
| 0 | No shivering |
| 1 | No visible muscle activity, but one or more of piloerection, peripheral vasoconstriction or peripheral cyanosis (other causes excluded). |
| 2 | Muscular activity in only one muscle group. |
| 3 | Moderate muscular activity in more than one muscle group, but not generalised shaking. |
| 4 | Violent muscular activity that involves the entire body. |
Patients were randomly allocated to one of the two groups (Group N or Group T) by drawing sequential numbered opaque sealed envelopes containing a code based on computer generated number list. The study drug was prepared by an anaesthesiologist who was not involved in the study. The primary researchers conducting the study and recording the data were unaware of the preparation administered. Decoding was done at the end of the study.
Group N received Injection (Inj.) nalbuphine 0.1 mg/kg IV and group T received Inj. tramadol 1 mg/kg IV, drugs were diluted to 10 mL with normal saline for both the study groups. The following criteria were monitored and noted:
Grade of shivering [19] [Table/Fig-2]. Grade of shivering was monitored for 15 minutes and assessed whether the improvement in shivering was complete or partial. Complete improvement of shivering was when grade of shivering returned to grade 0 and partial improvement of shivering was when grade of shivering had decreased but not reached grade 0.
Time taken for disappearance of shivering was noted as time from administration of study drug till grade of shivering becomes 0.
Recurrence of shivering was noted which was defined as the reappearance of shivering after its full resolution, before completion of the surgery. If grade of shivering remained unchanged for 15 minutes, the treatment was considered to be non-effective. Patients who did not respond or had partial improvement in shivering or had recurrence, were given a repeat dose of the study drug which was prepared by the same anaesthesiologist who had prepared it before [13].
Side-effects such as hypotension (SBP <90 mm of Hg), bradycardia (HR <50 beats/min), nausea, vomiting, respiratory depression and sedation were noted. Hypotension, bradycardia and vomiting were treated with Inj. mephentermine, atropine and ondansetron respectively.
Sedation was assessed according to Ramsay Sedation Score (RSS) [23] and occurrence of deep sedation RSS >3 was noted [Table/Fig-3].
Ramsay Sedation Score (RSS).
| Score | Response |
|---|
| 1 | Anxious or restless or both |
| 2 | Cooperative, oriented and tranquil |
| 3 | Responding to verbal commands |
| 4 | Brisk response to stimulus |
| 5 | Sluggish response to stimulus |
| 6 | No response to stimulus |
Statistical Analysis
Descriptive statistics such as mean, standard deviation or percentages were calculated for the variables. Statistical Package for Social Sciences (SPSS, IBM version 22.0) was used to compare continuous variables between the two groups. To test the hypothesis, Student’s t-test and Chi-square tests were used at 5% level of significance.
Results
A total of 60 patients were enrolled in the study and were randomised into two groups of 30 each. The patient characteristics were comparable in both groups with respect to age, sex, weight, ASA grade and duration of surgery [Table/Fig-4].
Demographic profile of patients of both groups.
| Demographic characteristics | Mean±SD | p-value (Student’s t-test) |
|---|
| Group T | Group N |
|---|
| Age (years) | 38.43±11.70 | 38.33±11.58 | 0.895 |
| Sex (male/female) | 19/11 | 21/9 | 0.632 |
| Weight (kg) | 59.26±8.60 | 59.56±9.16 | 0.896 |
| ASA grade (I/II) | (22/8) | (20/10) | 0.78 |
| Duration of surgery (minutes) | 155.00±34.41 | 151.00±44.20 | 0.697 |
Shivering Grades 3, 2, 1 were present in 3%, 77% and 20% of patients of Group N and 0%, 77% and 23% in patients of Group T, which were comparable. The mean time taken for disappearance of shivering (i.e., time from administration of study drug till grade of shivering became 0) was lesser in group N as compared to group T (3.20±0.96 minutes and 6.43±0.97 minutes, respectively). Complete improvement of shivering was noted in 100% of cases in nalbuphine group and 80% of cases in tramadol group within 15 minutes of administration of study drug. There was only partial improvement in shivering in 20% of patients in tramadol group. Recurrence of shivering was seen in four patients (13%) of Group T and none in Group N as shown in [Table/Fig-5]. Ten patients in tramadol group (6 with partial improvement of shivering and 4 with recurrence of shivering) were given repeat dose of tramadol (1 mg/kg).
Parameters of postspinal shivering and its response.
| Variables | Group T (n=30) | Group N (n=30) | p-value (Chi-square) |
|---|
| Shivering grade (I/II/III) | (7/23/0) | (6/23/1) | 0.177 |
| Time taken for disappearance of shivering (minutes) (Mean±SD) | 6.43±0.97 | 3.20±0.96 | 0.001 |
| Improvement in shivering |
| Not improved | - | - | |
| Partially improved | 6 | - | |
| Completely improved | 24 | 30 | |
| Recurrence of shivering | 4 | - | |
Intraoperative vitals i.e., HR, mean arterial pressure, SpO2 and temperature were comparable in both groups [Table/Fig-6].
Evaluation of the intraoperative vitals among the study groups.
| Heart rate | Tramadol (beats/min) Mean±SD | Nalbuphine (beats/min) Mean±SD | p-value (Student’s t-test) |
|---|
| 0 minute | 82.80±8.04 | 83.86±6.47 | 0.574 |
| 1 minute | 82.20±7.58 | 82.46±5.92 | 0.880 |
| 3 minutes | 84.53±7.18 | 88.46±8.11 | 0.06 |
| 5 minutes | 81.13±8.31 | 83.46±5.25 | 0.192 |
| 10 minutes | 80.53±7.92 | 83.06±5.99 | 0.168 |
| 15 minutes | 79.60±7.34 | 83.00±6.38 | 0.061 |
| 20 minutes | 81.46±7.66 | 81.86±6.92 | 0.833 |
| 25 minutes | 82.33±8.00 | 81.83±6.90 | 0.796 |
| 30 minutes | 83.33±8.05 | 81.46±5.92 | 0.309 |
| 60 minutes | 82.06±7.39 | 79.6±9.02 | 0.252 |
| 90 minutes | 82.66±7.03 | 79.60±8.93 | 0.145 |
| 120 minutes | 81.80±6.48 | 79.33±8.98 | 0.227 |
| 150 minutes | 80.33±6.88 | 80.86±7.74 | 0.779 |
| 180 minutes | 80.33±5.83 | 81.73±5.40 | 0.538 |
| SpO2 | Tramadol (%) Mean±SD | Nalbuphine (%) Mean±SD | p-value (Student’s t-test) |
| 0 minute | 98.3±.98 | 98.26±1.01 | 0.876 |
| 1 minute | 98.3±.88 | 98.43±.67 | 0.522 |
| 3 minutes | 98.76±.50 | 98.76±.43 | 1.00 |
| 5 minutes | 98.4±.89 | 98.73±.44 | 0.103 |
| 10 minutes | 98.76±.50 | 98.80±.40 | 0.733 |
| 15 minutes | 98.83±.46 | 98.86±.34 | 0.774 |
| 20 minutes | 98.6±.46 | 98.43±.45 | 0.153 |
| 25 minutes | 98.70±.59 | 98.90±.30 | 0.103 |
| 30 minutes | 98.6±.93 | 98.84±.69 | 0.261 |
| 60 minutes | 98.76±.50 | 98.86±.34 | 0.368 |
| 90 minutes | 98.76±.30 | 98.65±.32 | 0.174 |
| 120 minutes | 98.66±.89 | 98.80±.36 | 0.427 |
| 150 minutes | 98.73±.52 | 98.66±.80 | 0.689 |
| 180 minutes | 98.83±.46 | 98.80±.48 | 0.805 |
| SBP | Tramadol (mmHg) Mean±SD | Nalbuphine (mmHg) Mean±SD | p-value (Student’s t-test) |
| 0 minute | 125.13±6.31 | 128.13±9.20 | 0.146 |
| 1 minute | 123.66±9.24 | 126.86±8.81 | 0.175 |
| 3 minutes | 121.13±11.92 | 121.46±10.04 | 0.907 |
| 5 minutes | 118.06±10.32 | 121.06±9.16 | 0.239 |
| 10 minutes | 118.26±10.32 | 121.86±10.64 | 0.189 |
| 15 minutes | 118.06±9.16 | 121.13±12.14 | 0.274 |
| 20 minutes | 121.60±11.40 | 120.06±8.96 | 0.565 |
| 25 minutes | 122.53±12.24 | 118.80±8.42 | 0.174 |
| 30 minutes | 122.13±11.38 | 119.60±6.46 | 0.294 |
| 60 minutes | 121.70±8.58 | 119.53±7.38 | 0.299 |
| 90 minutes | 123.33±8.32 | 119.73±6.55 | 0.068 |
| 120 minutes | 118.40±7.48 | 116.33±8.53 | 0.321 |
| 150 minutes | 123.66±6.45 | 120.26±7.78 | 0.071 |
| 180 minutes | 122.86±6.84 | 121.40±6.93 | 0.413 |
| DBP | Tramadol (mmHg) Mean±SD | Nalbuphine (mmHg) Mean±SD | p-value (Student’s t-test) |
| 0 minute | 81.26±6.18 | 82.8±6.84 | 0.364 |
| 1 minute | 79.10±7.35 | 82.46±5.95 | 0.06 |
| 3 minutes | 76.60±7.84 | 80.4±8.42 | 0.07 |
| 5 minutes | 78.33±6.60 | 80.1±7.20 | 0.325 |
| 10 minutes | 78.13±6.94 | 79.26±8.02 | 0.561 |
| 15 minutes | 75.93±8.02 | 78.13±9.54 | 0.338 |
| 20 minutes | 79.66±8.61 | 79.4±8.78 | 0.906 |
| 25 minutes | 78.6±8.40 | 79.46±8.30 | 0.689 |
| 30 minutes | 78.06±8.05 | 79.33±7.37 | 0.528 |
| 60 minutes | 79.26±5.52 | 78.33±6.39 | 0.547 |
| 90 minutes | 79.46±5.70 | 77.8±5.95 | 0.273 |
| 120 minutes | 77.73±4.74 | 78.4±6.64 | 0.657 |
| 150 minutes | 78.00±5.30 | 79.2±4.74 | 0.360 |
| 180 minutes | 78.26±6.05 | 78.93±5.19 | 0.649 |
| Temperature | Tramadol (°F) Mean±SD | Nalbuphine (°F) Mean±SD | p-value (Student’s t-test) |
| 0 minute | 98.76±0.74 | 98.60±0.51 | 0.336 |
| 1 minute | 98.63±0.67 | 98.39±0.63 | 0.0158 |
| 3 minutes | 97.25±1.94 | 97.80±0.65 | 0.143 |
| 5 minutes | 97.48±0.58 | 97.66±0.65 | 0.283 |
| 10 minutes | 97.78±0.58 | 97.85±0.80 | 0.699 |
| 15 minutes | 97.48±0.64 | 97.55±0.97 | 0.317 |
| 20 minutes | 98.57±0.67 | 98.09±0.76 | 0.097 |
| 25 minutes | 97.63±0.75 | 97.90±0.70 | 0.158 |
| 30 minutes | 98.61±0.76 | 98.50±0.72 | 0.560 |
| 60 minutes | 98.47±0.77 | 98.32±0.87 | 0.482 |
| 90 minutes | 97.64±0.77 | 97.98±0.91 | 0.128 |
| 120 minutes | 97.64±0.71 | 97.75±0.84 | 0.587 |
| 150 minutes | 97.61±0.73 | 97.86±0.72 | 0.183 |
| 180 minutes | 97.88±0.78 | 97.95±0.65 | 0.707 |
a) Heart rate; b) Oxygen saturation (SpO2); c) Systolic blood pressure (SBP); d) Diastolic blood pressure (DBP); e) Temperature; p-value <0.05 to be considered significant
Better sedation was seen in nalbuphine group as grade 3 sedation were seen in 15 patients of nalbuphine group as compared to none in tramadol group. The mean duration of sedation was reported to be significantly longer in Group N than Group T. Complications such as nausea and vomiting were seen in Group T (three and one patient, respectively) and none in Group N [Table/Fig-7].
Comparison of side-effects and sedation of both groups.
| Comparative analysis | Group N | Group T | p-value (Chi-square) |
|---|
| Side-effects |
| Bradycardia | - | - | |
| Hypotension | - | - | |
| Nausea | - | 3 | |
| Vomiting | - | 1 | |
| Respiratory depression | - | - | |
| Sedation (RSS) |
| 1 | - | 12 | |
| 2 | 15 | 18 | 0.04 |
| 3 | 15 | - | |
| Duration of sedation (minutes) | 36±5.78 | 21.33±5.71 | 0.001 |
RSS: Ramsay sedation score
Discussion
Anaesthesia-induced impairment of thermoregulatory mechanism is one of the most likely causes of postoperative shivering. Duration of anaesthesia, age, sex and temperature of Operation Theatre (OT) are other contributing factors of shivering [24]. The neurotransmitter pathways related to shivering involves opioids, α2 adrenergic agonists, serotonergic and anticholinergic receptors and the drugs acting on these were used in the treatment of shivering [25-27].
In this current study, results inferred that both tramadol and nalbuphine were effective in treatment of postspinal shivering but nalbuphine was better than tramadol. Consistent to this study were the observations made by Kumar V et al., who did a comparative study between nalbuphine and tramadol for the treatment of postspinal shivering. Ninety patients who developed shivering were randomly divided into two equal groups and were given either 0.06 mg/kg IV of nalbuphine or 1 mg/kg IV of tramadol. The time taken for cessation of shivering was significantly less with nalbuphine (3.84±1.23 minutes) in comparison with tramadol (4.84±1.23 minutes, p-0.009) [28]. Sun J et al., did a randomised study in which nalbuphine (0.07 mg/kg IV) and dexmedetomidine (0.5 μg/kg IV) were compared with saline for the treatment of postneuraxial shivering in 120 pregnant ladies undergoing caesarean section. The mean time for cessation of shivering after treatment in nalbuphine and dexmedetomidine group were significantly shorter than the control group (3.8±2.6 and 4.7±3.5 versus 14.8±0.6 minutes, p<0.0001). The success rate of shivering treatment in nalbuphine and dexmedetomidine groups were significantly higher than the control group (95%, 90% and 17.5% respectively, p<0.0001) [29].
Many researches have compared tramadol with other drugs to evaluate its anti-shivering properties. Wang J et al., did a meta-analysis of randomised controlled trials comparing intravenous dexmedetomidine versus tramadol for treatment of shivering after spinal anaesthesia. Thirteen randomised controlled trials including 864 subjects were included. The results showed that dexmedetomidine had higher effective rate of shivering control, shorter time to cease shivering and lower recurrent rate of shivering [30]. Similarly, Kundra TS et al., did a double blind, randomised trial in which 100 patients who developed postspinal shivering were randomly divided into two groups of 50 patients each: Group A received Inj. dexmedetomidine 0.5 mcg/kg IV and Group B received Inj. tramadol 0.5 mg/kg IV. The duration for cessation of shivering was significantly shorter in Group A (dexmedetomidine) as compared to Group B (tramadol) and Group A also had lower rate of recurrence of shivering. Side-effects such as nausea and vomiting were significantly more in Group B. Hence the study concluded that dexmedetomidine offered better results than tramadol with fewer side-effects [21]. Fern L and Misirian K did a study in which patients who developed shivering after neuraxial anaesthesia were randomly allocated to receive intravenously either dexmedetomidine 0.5 μg/kg (n=20), pethidine 0.5 mg/kg (n=20) or tramadol 0.5 mg/kg (n=20) intravenously. In dexmedetomidine group, shivering was controlled in all the patients while in tramadol group only 11 patients had abolition of shivering which was statistically significant (p=0.0012). Thus, it was observed that dexmedetomidine 0.5 μg/kg was more effective than tramadol 0.5 mg/kg and pethidine 0.5 mg/kg and both tramadol and pethidine were found to have similar efficacy [20]. In concordance to the above studies, it was observed in the present study that tramadol took longer time for disappearance of shivering with complete improvement of shivering, seen in only 80% of patients and 13% of patients had recurrence of shivering as compared to nalbuphine group. Side-effects such as nausea and vomiting were also observed in tramadol group. Better sedation was seen in nalbuphine group which made the patients more comfortable. In view of all these observations, nalbuphine was found to be more superior to tramadol in controlling postspinal shivering.
Limitation(s)
Shivering was monitored for the intraoperative period only. Axillary temperature was monitored and not core temperature. Monitoring of core temperature was not feasible as it would have been uncomfortable to the patient.
Conclusion(s)
In conclusion, nalbuphine 0.1 mg/kg IV was better than tramadol 1 mg/kg IV in treating postspinal shivering as it controlled shivering faster with complete improvement and had no recurrence of shivering. Nalbuphine also gave better sedation with lesser side-effects.
a) Heart rate; b) Oxygen saturation (SpO2); c) Systolic blood pressure (SBP); d) Diastolic blood pressure (DBP); e) Temperature; p-value <0.05 to be considered significant
RSS: Ramsay sedation score
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 24, 2021
Manual Googling: Apr 14, 2021
iThenticate Software: Mar 27, 2021 (17%)
[1]. Larry JC, Donal JB, Shivering and neuraxial anaesthesiaReg Anesth Pain Med 2008 33(3):241-52.10.1016/j.rapm.2007.11.00618433676 [Google Scholar] [CrossRef] [PubMed]
[2]. Sessler Daniel I, Temperature Monitoring. Millar RD (ed)Textbook of Anaesthesia 1994 5th edition edNew YorkChurchill Livingstone Inc:1367-89.10.1097/00000542-199511000-000087486181 [Google Scholar] [CrossRef] [PubMed]
[3]. Matsukawa T, Sessler DI, Christensen R, Ozaki M, Schroeder M, Heat flow and distribution during epidural anesthesiaAnesthesiology 1995 83(5):961-67. [Google Scholar]
[4]. Bhattacharya PK, Bhattacharya L, Jain RK, Agarwal RC, Post Anesthetic Shivering (PAS): A reviewIndian Journal Anaesthesia 2003 47(2):88-93. [Google Scholar]
[5]. Krithika V, Selvarajan R, Nileena S, Anandan H, Control of shivering with butorphanol and tramadol under spinal anesthesia- A comparative studyInt J Sci Stud 2017 5(3):98-101. [Google Scholar]
[6]. Dal D, Kose A, Honca M, Akinci SB, Basgul E, Aypar U, Efficacy of prophylactic ketamine in preventing postoperative shiveringBr J Anaesth 2005 95(2):189-92.10.1093/bja/aei14815849207 [Google Scholar] [CrossRef] [PubMed]
[7]. Buggy DJ, Crossley AW, Thermoregulation, mild perioperative hypothermia and postanaesthetic shiveringBr J Anaesth 2000 84(5):615-28.10.1093/bja/84.5.61510844839 [Google Scholar] [CrossRef] [PubMed]
[8]. Frank SM, Higgins MS, Breslow MJ, Fleisher LA, Gorman RB, Sitzmann JV, The catecholamine, cortisol, and hemodynamic responses to mild perioperative hypothermia: A randomised clinical trialAnesthesiology 1995 82(1):83-93.10.1097/00000542-199501000-000127832339 [Google Scholar] [CrossRef] [PubMed]
[9]. Bhatnagar S, Saxena A, Kannan TR, Punj J, Panigrahi M, Mishra S, Tramadol for postoperative shivering: A double blind comparison with PethedineAnaesth Intensive care 2001 29(2):149-54.10.1177/0310057X010290020911314834 [Google Scholar] [CrossRef] [PubMed]
[10]. Katyal S, Tewari A, Shivering: Anesthetic considerationsJ Anaesth Clin Pharmacol 2002 18(4):363-76. [Google Scholar]
[11]. Raffa RB, Friderichs E, Reimann W, Shank RP, Codd EE, Vaught JL, Opioid and nonopioid components independently contribute to the mechanism of action of tramadol, an “atypical” opioid analgesicJ Pharmacol Exp Ther 1992 260(1):275-85. [Google Scholar]
[12]. Chan AM, Ng KF, Tong EW, Jan GS, Control of shivering under regional anesthesia in obstetric patients with tramadolCan J Anaesth 1999 46(3):253-58.10.1007/BF0301260510210050 [Google Scholar] [CrossRef] [PubMed]
[13]. Dhimar AA, Patel MG, Swadia VN, Tramadol for control of shivering (Comparison with pethidineIndian J Anaesth 2007 51:28-31. [Google Scholar]
[14]. Kurz M, Belani KG, Sessler DI, Kurz A, Larson MD, Schroeder M, Naloxone, meperidine, and shiveringAnesthesiology 1993 79(6):1193-201.10.1097/00000542-199312000-000098267194 [Google Scholar] [CrossRef] [PubMed]
[15]. Schmidt LG, Kuhn S, Smolka M, Schmidt K, Rommelspacher H, Lisuride, a dopamine D2 receptor agonist, and anticraving drug expectancy as modifiers of relapse in alcohol dependenceProg Neuropsychopharmacol Biol Psychiatry 2002 26(2):209-17.10.1016/S0278-5846(01)00214-7 [Google Scholar] [CrossRef]
[16]. Hoskin PJ, Hanks GW, Opioid agonist-antagonist drugs in acute and chronic pain statesDrugs 1991 41(3):326-44.10.2165/00003495-199141030-000021711441 [Google Scholar] [CrossRef] [PubMed]
[17]. Chowdhury MS, Ahmed S, Haque MM, Hossain MM, Shivering control in Subarachnoid block by Nalbuphine-A comparative study with PethidineJ Bangladesh Soc Anaesthesiol 2009 20(2):66-69.10.3329/jbsa.v20i2.3994 [Google Scholar] [CrossRef]
[18]. Shukla U, Malhotra K, Prabhakar T, A comparative study of the effect of clonidine and tramadol on post-spinal anaesthesia shiveringIndian J Anaesth 2011 55(3):242-46.10.4103/0019-5049.8266621808395 [Google Scholar] [CrossRef] [PubMed]
[19]. Crossley AW, Mahajan RP, The intensity of postoperative shivering is unrelated to axillary temperatureAnaesthesia 1994 49(3):205-07.10.1111/j.1365-2044.1994.tb03422.x8147511 [Google Scholar] [CrossRef] [PubMed]
[20]. Fern L, Misiran K, Comparison of dexmedetomidine, pethidine and tramadol in the treatment of post-neuraxial anaesthesia shiveringSouth Afr j Anaesth Analg 2015 21(1):14-18.10.1080/22201181.2015.1013323 [Google Scholar] [CrossRef]
[21]. Kundra TS, Kuthiala G, Shrivastava A, Kaur P, A comparative study on the efficacy of dexmedetomidine and tramadol on post-spinal anesthesia shiveringSaudi J Anaesth 2017 11(1):02-08.10.4103/1658-354X.19734428217045 [Google Scholar] [CrossRef] [PubMed]
[22]. Crowley L, Buggy D, Shivering and neuraxial anesthesiaReg Anesth Pain Med 2008 33(3):241-52.10.1016/j.rapm.2007.11.00618433676 [Google Scholar] [CrossRef] [PubMed]
[23]. Ramsay MAE, Savege TM, Simpson BRJ, Goodwin R, Controlled sedation with alphaxalone-alphadoloneBMJ 1974 2(5920):656-59.10.1136/bmj.2.5920.6564835444 [Google Scholar] [CrossRef] [PubMed]
[24]. Sessler DI, Ponte J, Shivering during epidural anesthesiaAnesthesiology 1990 72(5):816-21.10.1097/00000542-199005000-000082339797 [Google Scholar] [CrossRef] [PubMed]
[25]. Mathews S, Al Mulla A, Varghese PK, Radim K, Mumtaz S, Postanaesthetic shivering: A new look at tramadolAnaesthesia 2002 57(4):387-403.10.1046/j.1365-2044.2002.2457_3.x11949644 [Google Scholar] [CrossRef] [PubMed]
[26]. Kamibayashi T, Maze M, Clinical uses of alpha2-adrenergic agonistsAnesthesiology 2000 93(5):1345-49.10.1097/00000542-200011000-0003011046225 [Google Scholar] [CrossRef] [PubMed]
[27]. Bock M, Sinner B, Göttlicher M, Simon E, Martin E, Motsch J, Involvement of serotonergic pathways in postanesthetic cold defence: Dolasetron prevents shiveringJ Therm Biol 2002 27:159-66.10.1016/S0306-4565(01)00080-8 [Google Scholar] [CrossRef]
[28]. Kumar V, Nirala D, Prakash J, Ram B, Bhattacharya P, Priye S, Randomised double-blinded comparative study of intravenous nalbuphine and tramadol for the treatment of postspinal anesthesia shiveringAnesth Essays Res 2020 14(3):51010.4103/aer.AER_95_2034092867 [Google Scholar] [CrossRef] [PubMed]
[29]. Sun J, Zheng Z, Li YL, Zou LW, Li GH, Wang XG, Nalbuphine versus dexmedetomidine for treatment of combined spinal-epidural post-anesthetic shivering in pregnant women undergoing cesarean sectionJ Int Med Res 2019 47(9):4442-53.10.1177/030006051986506331353989 [Google Scholar] [CrossRef] [PubMed]
[30]. Wang J, Wang Z, Liu J, Wang N, Intravenous dexmedetomidine versus tramadol for treatment of shivering after spinal anesthesia: A meta-analysis of randomised controlled trialsBMC Anesthesiol 2020 20(1):10410.1186/s12871-020-01020-y32366218 [Google Scholar] [CrossRef] [PubMed]