Introduction
Abnormal Uterine Bleeding (AUB) is very common and major public health issue. AUB along with its sub-group often affects 14.25% women of reproductive age and have a major impact on their physical, social, emotional and material quality of life. It not only has direct impact on the woman and her family, but also on both the economy and health services.
Aim
To compare Magnetic Resonance (MR) hysterography and Sonohysterography (SSHG) for detection of uterine pathologies in women with AUB.
Materials and Methods
An interventional cross-sectional study was conducted over a period from July 2019 to July 2020, among 30 patients with severe AUB. SSHG and MR hysterography were used to assess endometrial pathology, which was assessed by both the diagnostic modality and considering histopathology as gold standard. The sensitivity, specificity, positive predictive value and negative predictive value for both diagnostic modalities was calculated.
Results
A very good agreement was noted in case of the cervical carcinoma whilst fibroid and endometrial hyperplasia showed good and fair agreement respectively by both the diagnostic modalities. Sensitivity of fibroid and cervical carcinoma was 100%, polyp was 33.33%, and endometrial hyperplasia was 87.50%. Whereas specificity of fibroid was 91.67%, endometrial hyperplasia was 86.30% and cervical carcinoma was 100%. Polyp and submucosal fibroid both showed 96.30% specificity. For pathology like cervical carcinoma, endometrial hyperplasia, fibroid had very high agreement with kappa value 1, 0.684 and 0.814 respectively, whereas agreement for two tests for pathology like submucous fibroid, dual pathology was less.
Conclusion
MR Hysterography and Sonohysterography were having almost equal sensitivity and specificity for abnormal uterine bleeding and can be used as per patient preference, patient discomfort, and availability of investigation.
Abdominal sonography, Adenomyosis, Endometrial carcinoma, Flair sequencing
Introduction
The AUB is very common and a major public health issue. AUB along with its sub-group often affects 14.25% women of reproductive age and have major impact on their physical, social, emotional and material quality of life. It not only has direct impact on the woman and her family, but also on both economy and health services [1].
The aetiology of AUB varies from simple dysfunctional uterine bleeding without any organic cause to the endometrial carcinoma. Complete workup is needed to point out various causes in perimenopausal and postmenopausal patients as the risk of endometrial carcinoma is 10% to 15% in this age group [2].
Generally for the effective management of AUB, noninvasive medical treatments are preferred which are mainly focused on the source of bleeding. Most common medical therapy is hormonal contraceptives since a long time, and the 52 mg Levonorgestrel Intrauterine System (LNG IUS) is increasingly used to control difficult bleeding before a surgical management. The most common aetiology is mostly benign in reproductive group females [3].
One of the reference standard investigations for AUB is hysteroscopy with biopsy over the years. However, it is invasive and expensive. It is an accurate method for diagnosing and treating endometrial abnormalities, but not able to give accurate information on size and extent of the lesion, which precludes its use as a primary diagnostic procedure in patients with AUB [4].
Saline SSHG is a minimally invasive, cost-effective and acceptable diagnostic modality. It delineates better intracavitary structures and hence improves the diagnostic accuracy. Saline Infusion sonohysterogram may cause intracavitary infection if aseptic precautions are not taken else it is virtually devoid of procedural complications [5].
MRI for diagnosing abnormalities of the female genital tract has potential for replacing hystography/laparoscopy. As MRI is non-invasive and non-hazardous form of ionizing radiation and also having improved soft tissue contrast resolution and with multidirectional imaging capacity, it can also do multiple sections simultaneously [6].
MRI offers optimum imaging of the uterus due to its intrinsic tissue contrast and helps to represent three different layers on T2-weighted MR sequences: the endometrium of high signal intensity, the junctional zone of low signal intensity, and the myometrium of moderate signal intensity. MRI is more capable than radiographic hysterography or sonography in reflecting the size and number of myomas and separating myomas from adenomyosis. These results are important for surgical planning [7]. However, with MRI, cavity contrast differentiation, which is very important for determining the percentage of mass that is intracavitary, is reduced.
This information was essential for diagnosis and surgical planning. Rouanet De Lavit JP et al,. has tried to overcome this limitation by developing a technique called MR hysterography which consists of injecting saline solution into the uterine cavity followed by Fluid Attenuated Inversion Recovery (FLAIR) sequences to null the bright signal of the saline [8].
They observed that the use of this technique, helped in better depiction and delineation of small endometrial pathologies against the background of contrast provided by saline. Based on this observation this study was carried out to compare the ability of Saline SSHG and MR hysterography to evaluate pathologies in women with AUB.
Materials and Methods
An interventional cross-sectional study was conducted in Department of Radiodiagnosis, Mahatma Gandhi Medical College and Research Institute, Pondicherry, India, over a period from July 2019 to July 2020. Written informed consent from each study subject was taken and ethical permission was taken from Institutional Ethical Committee (IEC NO-MD/MS/45).
A total of 30 patients with clinical evidence of AUB which was severe and needed further investigation was diagnosed on the basis of history and clinical examination such as pallor with no obvious other reason, were sent to the Department of Radiodiagnosis for the Transabdominal Scan (TAS). Based on the TAS findings further investigation with saline SSHG and MR hysterography was done.
Inclusion Criteria
Patients with complaint of AUB for any duration which was not controlled by medical management and need further evaluation.
Age range 21-60 years.
Adenomyosis, Endometriosis, Polyps, cervical or endometrial, Submucosal fibroids
Exclusion Criteria
Previous transcervical endometrial resection,
Malignant diagnosis,
Acute or subacute indications for hysterectomy.
Ectopic pregnancy, puerperium
Systemic disease, Cirrhosis, Coagulation disorder, Hypothyroidism
Any condition Contraindicated for MRI
Sample size calculation: Sample size was calculated by using sensitivity and specificity for the diagnostic test. In previous study (Aslam M et al., [9]), sensitivity of SSHG was found to be 92.9% and specificity was 89.7% for diagnosing AUB. On calculation of sample size minimum of 22 subjects were required. However, a sample size of 30 was taken. Thirty women with complaints of vaginal bleeding, which was severe and needed further diagnostic evaluation were included in the study. Convenient sampling method was followed.
The study was performed between the 4th and 10th day of the patient’s menstrual cycle, which is in the secretory phase at that time. Cannulation was achieved before ovulation in women with a normal menstrual cycle, which ruled out the possibility of flushing out a fertilised ovum during the operation. A pre-procedure pregnancy test was performed in patients with an abnormal menstrual cycle unless the woman recently had a menstrual period or the use of effective contraception was verified. All patients were first evaluated with transabdominal {GE Voluson 730 Pro ultrasound systems with the linear transducer (7-12 MHz)} followed by MRI using Spectral Attenuated Inversion Recovery (SPAIR), T1 and T2 axial, T2 sagittal and FLAIR sequence. The plane of imaging was decided on the basis of the initial screening scan based on the orientation of the uterus. In both these studies the uterus was scanned in the sagittal and coronal planes for the presence of any myometrial and endometrial pathology.
Saline SSHG and MR hysterography was then performed after cannulating the patient with hysteron salphingo graphy catheter which was pre-instilled with saline to prevent artifacts due to air bubble. The anterior lip of the cervix was held with a vulsellum speculum and uterine sound was introduced to check for the position of the uterus. Following which the hysterosalphingography balloon catheter was inserted through the cervix and the balloon was inflated with air to seal the external OS of the cervix tightly to prevent any leakage into the vagina. The catheter was obturated and left in place so that re-injections could be performed if necessary.
A 10 mL of sterile saline solution was injected after transvaginal ultrasound probe was inserted slowly through the catheter under direct sonographic visualisation, after proper distension of the cavity, multiple sagittal and coronal images of the uterus were obtained and full details of any pathology if found was assessed and recorded. After Saline SSHG was finished the patient were taken for MR hysterography which was carried by placing the patient in the center of the magnet, survey sequences were taken and if needed additional volumes of saline was instilled through the catheter with help of extension cannula to overcome difficulty in instillation due to the shape of MRI gantry. The endometrial cavity was distended with saline, which allowed better delineation and characterisation of the lesion. Presence of polyps, submucous fibroids, focal endometrial thickenings and other pathologic conditions of the uterus like fibroids and adenomyosis were recorded. Patients with pathology were advised to undergo hysteroscopy directed biopsy or endometrial sampling. The appearance of the endometrium (atrophic, polypoidal, proliferative, secretory, or hyperplasic) and the presence of myometrial pathology like polyps, fibroids, synechiae, adenomyosis or carcinoma were recorded.
Outcome: Myometrial pathology and endometrial pathology were assessed by both the diagnostic modality and considering histopathological examination as gold standard, sensitivity, specificity, positive predictive value and negative predictive value were calculated.
Statistical Analysis
The accuracy of MR hysterography and Saline salphingography for assessment of AUB was determined by comparing the results with final diagnosis. Sensitivity, specificity, and positive and negative predictive values for predicting the disease were calculated. Z-test for two proportions was used to determine significance. Statistical significance was defined as a probability value of <0.05.
Results
In this study, the mean age of patients ranged from 39.50±8.05, out of which majority were in the age group of 30-50 years i.e., 73.3% (22/30 patients). Remaining 16.75% patients were in the age group of 21-30 while 10% were in age group of 51-60 [Table/Fig-1]. Location of lesion in myometrium could be well demarcated in both SSHG and MR hysterography compared to the TAS. Endometrial lesions were picked up better in MR hysterography compared to SSHG and TAS i.e., 56.7% vs. 46.7% and 20%, respectively. Multiple locations of the lesion and cervical lesions were picked up in all three modalities. Among 9 patients (30%) on TAS and 10% patients on SSHG, there was no pathology seen but was detected in MR hysterography.
Distribution of study subjects according to age.
| Age group (years) | N | % |
|---|
| 21-30 | 5 | 16.7 |
| 31-40 | 13 | 43.3 |
| 41-50 | 9 | 30 |
| 51-60 | 3 | 10 |
[Table/Fig-2] shows diagnosis in all the cases in this study. MR Hysterography was able to detect pathology in all the 30 (100%) study subjects, whereas in SSHG 10% had normal study subjects. Adenomyosis and endometrial carcinoma were better detected with MR Hysterography. Except for differential pathology all are statistically not significant.
Comparison of diagnosis of Saline Sonohysterography (SSHG), and MR Hysterography.
| Findings | SSHG (n %) | MR hysterography (n %) | p-value* |
|---|
| Normal | 3 (10%) | 0 (0) | 0.07 |
| Fibroid | 8 (26.7%) | 6 (20%) | 0.54 |
| Polyp | 2 (6.7%) | 3 (10%) | 0.64 |
| Focal adenomyosis | 0 (0) | 2 (6.7%) | 0.15 |
| Diffuse adenomyosis | 0 (0) | 2 (6.7%) | 0.15 |
| Submucosal fibroid | 1 (3.3%) | 3 (10%) | 0.30 |
| Endometrial hyperplasia | 10 (33.3%) | 8 (26.7%) | 0.57 |
| Endometrial carcinoma | 0 (0) | 2 (6.6%) | 0.15 |
| Cervical carcinoma | 1 (3.3%) | 1 (3.3%) | 1 |
| Differential pathology | 5 (16.7%) | 0 (0) | 0.02 |
| Dual pathology# | 0 (0) | 3 (10%) | 0.07 |
#Acute Uterus is included in the Dual Pathology, *- z test for two proportion
Sensitivity of fibroid and cervical carcinoma was 100%, polyp was 33.33%, Endometrial hyperplasia was 87.50%. Whereas specificity of fibroid was 91.67%, endometrial hyperplasia was 86.30% and cervical carcinoma was 100%. Polyp and submucosal fibroid both showed 96.30% specificity [Table/Fig-3].
Findings of Saline Sonohysterography (SSHG) diagnosis of study subjects.
| Findings of SSHG | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|
| Fibroid | 100.00 | 91.67 | 75.00 | 100.00 | 93.33 |
| Polyp | 33.33 | 96.30 | 50.00 | 92.86 | 90.00 |
| Submucosal fibroid | 0.00 | 96.30 | 0.00 | 89.66 | 86.67 |
| Endometrial hyperplasia | 87.50 | 86.30 | 70.00 | 95.00 | 86.67 |
| Cervical carcinoma | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 |
| Differential pathology | 0.00 | 83.33 | 0.00 | 100.00 | 83.3 |
| Dual pathology | 0.0 | 100.00 | 50.00 | 90.00 | 90.00 |
PPV: Positive predictive value; NPV: Negative predictive value
[Table/Fig-4] shows the sensitivity of fibroid and cervical carcinoma was 100%, polyp was 63.33% whereas specificity of fibroid was 96.36%.
Findings of MR Hysterography diagnosis of study subjects.
| Findings of MR | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|
| Fibroid | 100.00 | 96.36 | 79.17 | 100.00 | 96.36 |
| Polyp | 63.33 | 96.30 | 50.00 | 92.86 | 93.33 |
| Submucosal fibroid | 86.36 | 96.30 | 0.00 | 89.66 | 86.67 |
| Endometrial hyperplasia | 87.50 | 86.30 | 70.00 | 95.00 | 86.67 |
| Cervical carcinoma | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 |
| Differential pathology | 0.00 | 83.33 | 0.00 | 100.00 | 83.3 |
| Dual pathology | 0.0 | 100.00 | 50.00 | 90.00 | 90.00 |
PPV: Positive predictive value; NPV: Negative predictive value
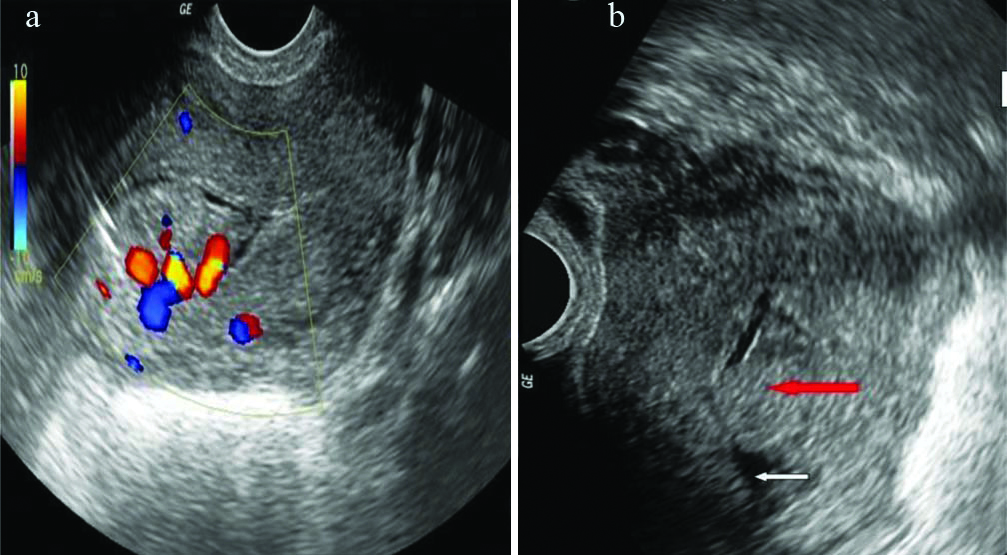
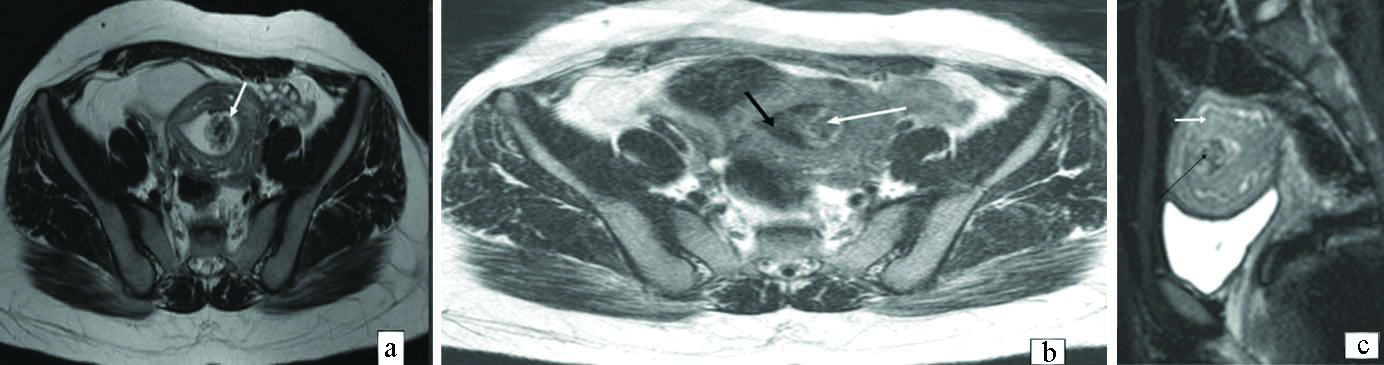
[Table/Fig-5] shows Agreement between Saline Sonohysterography (SSHG) diagnoses with MR Hystergraphy. For pathology like cervical carcinoma, endometrial hyperplasia, fibroid had very high agreement with kappa value 1, 0.684 and 0.814, whereas agreement for two test for pathology like submucous fibroid, dual pathology was found to be less. Few representative images are shown in [Table/Fig-6,7].
Agreement between Saline Sonohysterography (SSHG) diagnosis with MR hystergraphy.
| Findings of SSHG | Kappa value | p-value |
|---|
| Fibroid | 0.814 | <0.001** |
| Polyp | 0.348 | 0.050* |
| Submucosal fibroid | 0.00 | 0.734 |
| Endometrial hyperplasia | 0.684 | 0.001** |
| Cervical carcinoma | 1.00 | <0.001** |
| Differential pathology | 0.0 | 1.000 |
| Dual pathology | 0.00 | 1.000 |
*Significant; **Highly significant
a and b: Saline Sonohysterography (SSHG) depicts the saline filled endometrium (white arrow) clearly showing an intraluminal lesion (Red arrow) with presence of vascular pedicle on colour Doppler.
a) T2 WI axial scans, b) postsaline infusion FLAIR (White arrow indicates presence of heterogeneous polypoidal intraluminal lesion and Black arrow indicate contrast provided by saline followed by flair), c) T2 WI sagittal scans.
Discussion
This is study conducted for comparison of MR hysterography and saline SSHG in the case of AUB. In this study, on investigating the cases of AUB by MR hysterography it was found that 6 cases had fibroids, 3 cases had polyps, 2 cases had the endometrial carcinoma, 1 case had the cervical carcinoma and 3 cases had dual pathology. In 3 cases, no pathology was detected on Saline SSHG. But in MR hysterography, two of the cases had mucosal endometrial polyps, which was seen as high-signal-intensity lesions projecting into the endometrial cavity and was better appreciated with the dark outline of saline in FLAIR sequence. In the other case, early diffuse adenomyotic changes were seen as endometrial invaginations, which appeared, as high signal intensity lesion in the background of low signal intensity myometrium. Similarly, Rouanet De Lavit JP et al., in his study MR hysterography performed with saline injection and FLAIR sequences [8]. Initial experience conducted a prospective study over a period of 2 months in 10 women in whom abnormality of endometrium was suspected and had observed similar findings.
In this present study, very good agreement was noted in case of the cervical carcinoma whilst fibroid and endometrial hyperplasia showed good and fair agreement respectively. Sensitivity of fibroid and cervical carcinoma was 100%, polyp was 33.33%, endometrial hyperplasia was 87.50%. Whereas specificity of fibroid was 91.67%, endometrial hyperplasia was 86.30% and cervical carcinoma was 100%. Polyp and submucosal fibroid both showed 96.30% specificity. Other studies done to show the comparison of MR hysterography with saline SSHG such as by Dueholm M et al., shows the overall sensitivity was for MRI 0.76, for HSE 0.83 [10]. The specificity was MRI 0.92, HSE 0.90, which is almost in accordance to our study [Table/Fig-8] [10-12]. Malek KA et al., shows MRI was superior to HSG in diagnosing uterine anomalies (accuracy 100% vs. 96%), but failed to diagnose any case of intrauterine adhesions or peritubal adhesions which is almost similar to our study affirming superiority of MRI over saline SSHG [6]. Moradan S et al., shows SIS probably is a proper method for detecting endometrial focal lesion including polyps and myomas [12]. Study by Saini S et al., found sensitivity, specificity, positive predictive value and negative predictive value of SIS for the diagnosis of endometrial atrophy was 79.16%, 100%, 100% and 83.87% respectively which is higher than that of hysteroscopy and equivalent to histopathology, the high sensitivity and specificity were almost in accordance to present study [13]. MRI is not always available and is not always appropriate as a first-line investigation of abnormal bleeding, maximising recognition of adenomyosis at SSHG is important.
Comparison of present study with other studies.
| Study | Sensitivity of MR for fibroid | Specificity of MR for fibroid |
|---|
| Present study | 100% | 96.36% |
| Dueholm M et al., [10] | 76% | 92% |
| Rosa Moghadam et al., [11] | 94% | 33% |
| Moradan S et al., [12] | 79.6% | 89.1% |
Limitation(s)
The major drawbacks of this study was that factors like cost-effectiveness, time spent, patient preference, patient discomfort and treatment effects of saline salphingography and MR hysterography were not taken into account. Selection bias may be there.
Conclusion(s)
On the basis of this study we can conclude that both MR Hysterography and Sonohysterography had almost equal sensitivity and specificity for abnormal uterine bleeding and can be used as per patient preference, patient discomfort, and availability of investigation.
#Acute Uterus is included in the Dual Pathology, *- z test for two proportion
PPV: Positive predictive value; NPV: Negative predictive value
PPV: Positive predictive value; NPV: Negative predictive value
*Significant; **Highly significant
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 01, 2020
Manual Googling: Feb 13, 2021
iThenticate Software: Mar 13, 2021 (16%)
[1]. Whitaker L, Critchley HO, Abnormal uterine bleedingBest Pract Res Clin Obstet Gynaecol 2016 34:54-65.10.1016/j.bpobgyn.2015.11.01226803558 [Google Scholar] [CrossRef] [PubMed]
[2]. Mishra D, Sultan S, FIGO’s PALM–COEIN Classification of abnormal uterine bleeding: A clinico-histopathological correlation in Indian SettingJ Obstet Gynaecol India 2017 67(2):119-25.10.1007/s13224-016-0925-828405119 [Google Scholar] [CrossRef] [PubMed]
[3]. Marnach ML, Tommaso SK, Evaluation and management of abnormal uterine bleedingMayo Clin Proc 2019 94(2):326-35.10.1016/j.mayocp.2018.12.01230711128 [Google Scholar] [CrossRef] [PubMed]
[4]. Vathanan V, Armar NA, A comparative observational study of the use of saline uterine hydrosonography for the diagnosis and assessment of uterine cavity lesions in womenInternational Journal of Reproductive Medicine 2016 2016:931719410.1155/2016/931719427597989 [Google Scholar] [CrossRef] [PubMed]
[5]. Khan F, Jamaat S, Al-Jaroudi D, Saline infusion sonohysterography versus hysteroscopy for uterine cavity evaluationAnn Saudi Med 2011 31(4):387-92.10.4103/0256-4947.8321321808116 [Google Scholar] [CrossRef] [PubMed]
[6]. Malek KA, Hassan M, A prospective comparative study to assess the accuracy of MRI versus HSG in tubouterine causes of female infertilityMiddle East Fertility Society Journal 2005 10(3):01-07. [Google Scholar]
[7]. Kido A, Togashi K, Uterine anatomy and function on cine magnetic resonance imagingReprod Med Biol 2016 15:191-99.10.1007/s12522-016-0235-y29259437 [Google Scholar] [CrossRef] [PubMed]
[8]. Rouanet De Lavit JP, Maubon AJ, Thurmond AS, MR hysterography performed with saline injection and fluid attenuated inversion recovery sequences: Initial experienceAJR Am J Roentgenol 2000 175:774-76.10.2214/ajr.175.3.175077410954465 [Google Scholar] [CrossRef] [PubMed]
[9]. Aslam M, Ijaz L, Tariq S, Shafqat K, Un-Nisa M, Ashraf R, Comparison of transvaginal sonography and saline contrast sonohysterography in women with abnormal uterine bleeding: Correlation with hysteroscopy and histopathologyInt J Health Sci (Qassim) 2007 1(1):17-24. [Google Scholar]
[10]. Dueholm M, Lundorf E, Hansen ES, Ledertoug S, Olesen F, Evaluation of the uterine cavity with magnetic resonance imaging, transvaginal sonography, hysterosonographic examination, and diagnostic hysteroscopyFertil Steril 2001 76(2):350-57.10.1016/S0015-0282(01)01900-8 [Google Scholar] [CrossRef]
[11]. Moghadam R, Lathi RB, Shahmohamady B, Saberi NS, Nezhat CH, Nezhat F, Predictive value of magnetic resonance imaging in differentiating between fibroid and adenomyosisJSLS 2006 10(2):216-19. [Google Scholar]
[12]. Moradan S, Darzi SN, Ghorbani R, Diagnostic value of saline infusion sonohysterography for detecting endometrial focal lesionPan Afr Med J 2019 33:21110.11604/pamj.2019.33.211.1656331693718 [Google Scholar] [CrossRef] [PubMed]
[13]. Saini S, Jain S, Saini S, Bhardwaj M, Diagnostic value of saline infusion sonohysterography for detecting endometrial lesion and comparing it with hysteroscopy and histopathology in postmenopausal bleedingInt J Reprod Contracept Obstet Gynecol 2020 9(8):3320-25.10.18203/2320-1770.ijrcog20203316 [Google Scholar] [CrossRef]